First Aid Basics - Valley Stream Soccer Club
advertisement

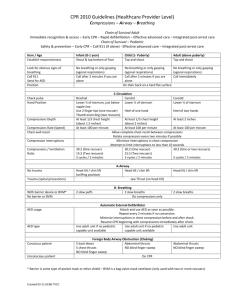
Valley Stream Soccer Club First Aid Basics An informational document for VSSC coaches and parents Contents Sprains and Strains Treatment......................................................................................................... 5 1. Control Swelling With RICE Therapy...................................................................................... 5 2. Manage Pain and Inflammation................................................................................................ 5 3. See a Health Care Provider ....................................................................................................... 5 4. Follow Up ....................................................................................................................................... 5 Cuts or Lacerations Treatment......................................................................................................... 6 1. Stop the Bleeding ........................................................................................................................ 6 2. Clean and Protect ........................................................................................................................ 6 3. Call a Health Care Provider if: .................................................................................................. 6 4. Follow Up ....................................................................................................................................... 6 Insect Sting Allergy Treatment ......................................................................................................... 7 1. Remove the Stinger..................................................................................................................... 7 2. Control Swelling........................................................................................................................... 7 3. Treat Symptoms ........................................................................................................................... 7 4. Follow-Up ....................................................................................................................................... 7 5. Call 911 if: ...................................................................................................................................... 7 Dizziness Treatment ............................................................................................................................ 9 1. Treat Symptoms ........................................................................................................................... 9 2. Call a Health Care Professional if: .......................................................................................... 9 3. Follow Up ....................................................................................................................................... 9 CPR for Children .................................................................................................................................. 10 1. Call 911 ......................................................................................................................................... 10 1. Check to see if the child is conscious. ...................................................................................... 10 3. Check Breathing........................................................................................................................... 10 4. Begin Chest Compressions ........................................................................................................ 10 5. Do Rescue Breathing .................................................................................................................. 10 2 6. Repeat Compressions and Rescue Breathing if Child Is Still Not Breathing...................... 11 7. Use AED as Soon as Available ................................................................................................. 11 Hands-Only CPR for Adults ................................................................................................................ 12 1. Check Responsiveness .............................................................................................................. 12 2. Do Chest Compressions ............................................................................................................. 12 3. Stop Only if: .................................................................................................................................. 12 4. Use an AED As Soon As It's Available ..................................................................................... 12 Heat Exhaustion Treatment ............................................................................................................. 13 Call 911 if:......................................................................................................................................... 13 1. Lower Body Temperature ........................................................................................................ 13 2. Rehydrate..................................................................................................................................... 13 3. Rest ............................................................................................................................................... 13 4. See a Health Care Provider ..................................................................................................... 13 Heat Stroke Treatment ...................................................................................................................... 14 Call 911 if the person has the following symptoms: ............................................................ 14 1. Call 911 ......................................................................................................................................... 14 2. Lower Body Temperature Quickly ........................................................................................ 14 3. Treat Symptoms ......................................................................................................................... 14 4. Follow Up ..................................................................................................................................... 14 Nosebleeds Treatment ...................................................................................................................... 15 1. Stop the Bleeding ...................................................................................................................... 15 2. Call a Health Care Provider ..................................................................................................... 15 3. Medical Treatment ..................................................................................................................... 15 4. Follow Up ..................................................................................................................................... 15 Concussion Treatment ........................................................................................................................ 16 1. Prevent Swelling and Further Injury .......................................................................................... 16 2. Treat Symptoms ........................................................................................................................... 16 3. Monitor Symptoms ....................................................................................................................... 16 4. When to Call a Doctor ................................................................................................................. 16 5. Follow-Up ...................................................................................................................................... 16 Choking Treatment............................................................................................................................... 17 Ankle Sprain Treatment .................................................................................................................... 18 3 1. Control Swelling......................................................................................................................... 18 2. Manage Pain and Inflammation.............................................................................................. 18 3. See a Health Care Provider ..................................................................................................... 18 Treating Bruises in Children ........................................................................................................... 19 Call Doctor If: .................................................................................................................................. 19 1. Apply Ice ...................................................................................................................................... 19 2. Elevate the Area ......................................................................................................................... 19 3. Reduce Pain ................................................................................................................................ 19 Treating Dehydration in Children Under 12 Years Old............................................................. 20 1. Call a Doctor ............................................................................................................................... 20 2. Replace Fluids ............................................................................................................................ 20 3. Follow Up ..................................................................................................................................... 20 Treating Dehydration in Adults and Children Over 12 .................................................................... 22 1. Replace Fluids .............................................................................................................................. 22 2. When to Call a Doctor for Mild Dehydration ............................................................................ 22 3. Follow Up ...................................................................................................................................... 22 Dislocated Elbow Treatment ........................................................................................................... 23 1. Don't Move the Elbow ............................................................................................................... 23 2. Treat Symptoms ......................................................................................................................... 23 3. Follow Up ..................................................................................................................................... 23 4 Sprains and Strains Treatment 1. Control Swelling With RICE Therapy Rest the sprained or strained area. If necessary, use a sling for an arm injury or crutches for a leg or foot injury. Splint an injured finger or toe by taping it to an adjacent finger or toe. Ice for 20 minutes every hour. Compress by wrapping an elastic (Ace) bandage or sleeve lightly (not tightly) around the joint or limb. Elevate the area above heart level. 2. Manage Pain and Inflammation Give an over-the-counter NSAID (non-steroidal anti-inflammatory drug) like ibuprofen (Advil, Motrin) or aspirin. Do not give aspirin to anyone under age 18. 3. See a Health Care Provider All but the most minor strains and sprains should be evaluated by a health care provider. Consult a health care provider as soon as possible if there are symptoms of a possible broken bone: There is a "popping" sound with the injury. The person can't move the injured joint or limb. The limb buckles when the injured joint is used. There is numbness. There is significant swelling, pain, fever, or open cuts. 4. Follow Up Continue RICE for 24 to 48 hours, or until the person sees a health care provider. The health care provider may want to do X-rays or an MRI to diagnose a severe sprain or strain or rule out a broken bone. The health care provider may need to immobilize the limb or joint with a splint, cast, or other device until healing is complete. In severe cases, surgery may be needed. 5 Cuts or Lacerations Treatment Call 911 if: A Cut Is Bleeding Severely Blood Is Spurting Out Bleeding Can't Be Stopped after 10 Minutes of Firm and Steady Pressure In general, a cut that needs stitches has to be repaired within 6 hours of the injury. The exception is cuts to the face and scalp, which generally can be repaired up to 24 hours after the injury. Take the following steps for minor cuts. 1. Stop the Bleeding Apply direct pressure on the area. 2. Clean and Protect Clean the area with warm water and gentle soap. Apply an antibiotic ointment to reduce chance of infection. Put a sterile bandage on the area. 3. Call a Health Care Provider if: The cut is deep or over a joint You cannot get the cut or laceration clean The injury is a deep puncture wound or the person has not had a recent (within the last 5 to 10 years) tetanus shot or booster The cut is from a human or animal bite 4. Follow Up For a minor cut or laceration, remove bandage after a couple of days to promote healing. See a health care provider if the cut doesn't heal or shows signs of infection, including redness, swelling, pus, or excessive pain. 6 Insect Sting Allergy Treatment Call 911 if the person has: Trouble breathing, feels faint or dizzy, has hives or a swollen tongue A history of severe allergy reaction to insect stings If the person does not have severe allergy symptoms: 1. Remove the Stinger Scrape the area with a fingernail or use tweezers to remove it. Don't pinch the stinger -- that can inject more venom. 2. Control Swelling Ice the area. If you were stung on your arm or leg, elevate it. Remove any tight-fitting jewelry from the area of the sting. As it swells, rings or bracelets might become hard to get off. 3. Treat Symptoms For pain, take an over-the-counter painkiller like acetaminophen or ibuprofen. Do not give aspirin to anyone under age 18. For itchiness, take an antihistamine. You can also apply a mixture of baking soda and water or calamine lotion. 4. Follow-Up It might take 2-5 days for the area to heal. Keep it clean to prevent infection. If the person does have severe allergy symptoms (anaphylaxis): 5. Call 911 if: Seek emergency care if the person has these symptoms or a history of severe allergic reactions (anaphylaxis), even if there are no symptoms: Difficulty breathing or wheezing Tightness in the throat or a feeling that the airways are closing Hoarseness or trouble speaking Nausea, abdominal pain, or vomiting Fast heartbeat or pulse 7 Skin that itches, tingles, swells, or turns red Anxiety or dizziness Loss of consciousness 1. Inject Epinephrine Immediately If the person has an anaphylaxis action plan from a doctor for injecting epinephrine and other emergency measures, follow it. Otherwise, if the person carries an epinephrine shot or one is available: Inject epinephrine if the person is unable to. If the person has a history of anaphylaxis, don't wait for signs of a severe reaction to inject epinephrine. Read and follow patient instructions carefully. Inject epinephrine into outer muscle of the thigh. Avoid injecting into a vein or buttock muscles. Do not inject medicine into hands or feet, which can cause tissue damage. If this happens, notify emergency room staff. The person may need more than one injection if there's no improvement after the first. For an adult, inject again after 10 to 20 minutes. For a child, inject again after 5 to 30 minutes. 2. Do CPR if the Person Stops Breathing For a child, start CPR for children For an adult, start adult CPR. 3. Follow Up Make sure that someone stays with the person for 24 hours after anaphylaxis in case of another attack. Report the reaction to the person's doctor. 8 Dizziness Treatment Call 911 if the Person Has: A Change in Vision or Speech Chest Pain Shortness of Breath Convulsions or Ongoing Vomiting Dizziness that Comes after a Head Injury Double Vision Fainting or Loss of Consciousness High Fever and Stiff Neck Inability to Move an Arm or Leg Slurred Speech 1. Treat Symptoms The person should sit down or lie still. If the person gets light-headed when standing up, the person should stand up slowly. Avoid sudden changes in position. If the person is thirsty, have him or her drink fluids. Avoid bright lights. 2. Call a Health Care Professional if: This is the first time the person has been dizzy. The dizziness is different than before or doesn't go away quickly. 3. Follow Up At the health care provider's office or hospital, the next steps depend on the particular case. The person may get oxygen or IV fluids to treat dehydration. If blood tests reveal abnormal blood chemistry (electrolyte levels), this will be corrected. Health care providers may start emergency treatment for heart attack or stroke, blood transfusion, or surgery. 9 CPR for Children Call 911 For adult CPR, see Hands-Only CPR for Adults. This article is a guideline. It is important to learn CPR to know how to do it correctly. For more information about a CPR course, go to redcross.org or heart.org. 1. Call 911 If you’re alone with a child or baby who is unresponsive and not breathing (or only gasping), call 911 after you’ve done 2 minutes of cardiopulmonary resuscitation (CPR). If someone else is present, shout for the person to call 911 and locate an AED (a defibrillator) right away while you begin CPR. If a child or baby is unconscious but you see regular breathing, call 911 and wait for help. A breathing child or baby does not need CPR, but one that is gasping does. 1. Check to see if the child is conscious. Make sure you and the child are in safe surroundings. Tap the child gently. Shout, “Are you OK?" Look quickly to see if the child has any injuries or medical problems. 3. Check Breathing Place your ear near the child’s mouth and nose. Is there breath on your cheek? Is the child’s chest moving? 4. Begin Chest Compressions If the child doesn’t respond and isn’t breathing: Carefully place child on back. For a baby, be careful not to tilt the head back too far. If you suspect a neck or head injury, roll baby over, moving entire body at once. For a baby, place two fingers on breastbone, For a child, place heel of one hand on center of chest at nipple line. You also can push with one hand on top of the other. For a child, press down about 2 inches. Make sure not to press on ribs. For a baby, press down about 1 1/2 inches, about 1/3 to 1/2 the depth of chest. Make sure not to press on the end of the breastbone. Do 30 chest compressions, at the rate of 100 per minute. Let the chest rise completely between pushes. Check to see if the child has started breathing. Continue CPR until emergency help arrives. 5. Do Rescue Breathing To open airway, lift child’s chin with one hand. At the same time, tilt head by pushing down on forehead with other hand. Do not tilt the head back if the child may have a neck or head injury. For a child, cover mouth tightly with yours. Pinch nose closed and give breaths. For a baby, cover mouth and nose with your mouth and give breaths. 10 Give child two breaths, watching for chest to rise each time. Each breath should take one second. 6. Repeat Compressions and Rescue Breathing if Child Is Still Not Breathing Two breaths can be given after every 30 chest compressions. If someone else is helping you, you should give 15 compressions, then 2 breaths. Continue this cycle of 30 compressions and 2 breaths until the child starts breathing or emergency help arrives. If you are alone with the child and have done 2 minutes of CPR (about 5 cycles of compressions and breathing), call 911 and find an AED. 7. Use AED as Soon as Available For children under 9 years old, use a pediatric automated external defibrillator (AED), if available. If a pediatric AED is not available, or for children age 1 and older, use a standard AED. Turn on AED. Wipe chest dry and attach the pads. The AED will give you step-by-step instructions. Continue compressions and follow AED prompts until emergency help arrives or the child starts breathing. 11 Hands-Only CPR for Adults Call 911 if a Person: Collapses Becomes Unresponsive 1. Check Responsiveness Tap the person's shoulder and shout, "Are you OK?" Look for normal breathing. Call 911 if there is no response. Start hands-only CPR. Hands-Only CPR should not be used for adults whose cardiac arrest is due to drug overdose, near-drowning, or an unwitnessed cardiac arrest. In these cases, do a conventional CPR combination of chest compressions and rescue breathing. 2. Do Chest Compressions Place the heel of your hand on the center of the person's chest. Place the heel of your other hand on top of your first hand, lacing fingers together. Keep arms straight and your shoulders directly over your hands. Push hard and fast, compressing chest at least 2 inches. Let chest rise completely before pushing down again. Compress at least 100 times per minute. 3. Stop Only if: The person starts breathing normally. A trained responder or emergency help takes over. You are too exhausted to continue. There is an automated external defibrillator (AED) to use. 4. Use an AED As Soon As It's Available Turn on the AED. It will give you step-by-step instructions. Wipe chest dry. Attach the pads. Plug in connector, if needed. Make sure no one is touching the person. Push the "Analyze" button if necessary. If a shock is advised, push the "Shock" button. Resume compressions and follow AED prompts. Note: For Hands-Only CPR instructions, go to www.redcross.org to download a free instruction guide. You can also call the American Heart Association at (800) AHA-USA1 or visit www.heart.org. 12 Heat Exhaustion Treatment Call 911 if: The person has a very high, weak pulse rate and rapid shallow breathing, especially when combined with high or low blood pressure The person is unconscious, disoriented, or has a high body temperature The person has warm, dry skin, elevated or lowered blood pressure, and hyperventilation 1. Lower Body Temperature Get the person out of the heat and into a cool environment. If air-conditioning is not available, fan the person. Spray the person with a garden hose, get him into a cool shower, apply cool compresses, or give the person a sponge bath 2. Rehydrate Give cool, nonalcoholic beverages as long as the person is alert. 3. Rest Have the person avoid physical activity for the rest of the day. Give over the counter acetaminophen if the person has a mild headache. 4. See a Health Care Provider Untreated heat exhaustion can progress to heat stroke. See a doctor that day if: Symptoms get worse or last more than an hour The person is nauseated or vomiting 13 Heat Stroke Treatment Call 911 if the person has the following symptoms: Body temperature above 103° F Rapid pulse Reduced sweating Disorientation Unconsciousness Seizures Warm, red, dry skin 1. Call 911 Heat stroke is a medical emergency. 2. Lower Body Temperature Quickly Get the person out of the sun. Immerse the person in a cool bath, spray the person with cool water, or apply cold wet cloths to the armpits, neck, and groin. Fan air across the person to increase cooling. These methods help cool the person quickly. Continue cooling efforts until the person's body temperature drops to 101º to 102° F. Do not give the person anything to drink. 3. Treat Symptoms If the person experiences seizures, keep him or her safe from injury. If the person vomits, turn the person on his or her side to keep the airway open. 4. Follow Up At the hospital, health care providers will rehydrate the person and continue cooling as needed. 14 Nosebleeds Treatment 1. Stop the Bleeding Have the person sit up straight and lean forward slightly. Don't have the person lie down or tilt the head backward. With thumb and index finger, firmly pinch the nose just below the bone up against the face. Apply pressure for 5 minutes. Time yourself with a clock. If bleeding continues after 5 minutes, repeat the process. 2. Call a Health Care Provider See a health care provider immediately if: Nosebleed doesn't stop after 10 minutes of home treatment. The person is taking blood thinners, such as warfarin (Coumadin) or aspirin, or has a bleeding disorder Nosebleed happens after a severe head injury or a blow to the face. 3. Medical Treatment The health care provider may use specialized cotton material, insert a balloon in the nose, or use a special electrical tool to cauterize the blood vessels. 4. Follow Up Broken noses often are not fixed immediately. The health care provider will refer the person to a specialist for a consultation once the swelling goes down. The person should avoid strenuous activity; bending over; and blowing, rubbing or picking the nose until it heals. 15 Concussion Treatment Call 911 if the Person: Is Vomiting Repeatedly Has Unequal Pupils Is Confused Has Weakness on One Side of the Body Passes Out or Is Unconscious for More Than 1 Minute Inability to Wake Up Seizure 1. Prevent Swelling and Further Injury Have the person stop activity and rest. Apply ice wrapped in a washcloth. 2. Treat Symptoms For pain, take over-the-counter acetaminophen (Tylenol). Aspirin or ibuprofen (Advil, Motrin) may make bruising worse. 3. Monitor Symptoms If possible, stay with the person for 24 hours. 4. When to Call a Doctor Drive the injured person to the doctor or hospital for: A headache that seems to be getting worse Continued vomiting Increased drowsiness or dizziness Increased confusion Heart palpitations, seizures, or loss of consciousness Neck pain after a fall 5. Follow-Up Symptoms will likely improve in 7 to 10 days. If they last longer, see a doctor. 16 Choking Treatment Call 911 if: The person is choking. The person is unconscious. For infants 12 months of age and younger, see Choking in Children. While Waiting for 911 If the Person Is Conscious but Not Able to Breathe or Talk: 1. Give Back Blows Give up to 5 blows between the shoulder blades with the heel of your hand. 2. If Person Is Still Choking, Do Thrusts If the person is not pregnant or obese, do abdominal thrusts: Stand behind the person and wrap your arms around the waist. Place your clenched fist just above the person’s navel. Grab your fist with your other hand. Quickly pull inward and upward. Continue cycles of 5 back blows and 5 abdominal thrusts until the object is coughed up or the person starts to breathe or cough. Take the object out of his mouth only if you can see it. Never do a finger sweep unless you can see the object in the person's mouth. If the person is obese or pregnant, do high abdominal thrusts: Stand behind the person, wrap your arms them, and position your hands at the base of the breast bone. Quickly pull inward and upward. Repeat until the object is dislodged. 3. Give CPR, if Necessary If the obstruction comes out, but the person is not breathing or if the person becomes unconscious: For a child, start CPR for children. For an adult, start CPR for adults. 4. Follow Up When emergency medical personnel arrive, they will take over and may do CPR or take the person to the hospital, if needed. 17 Ankle Sprain Treatment Go to the emergency room if: Pain, bruising, or swelling is severe, the ankle looks deformed or seems dislocated, or the person can't put any weight on the ankle. 1. Control Swelling Remove ankle bracelets or toe rings. Do RICE therapy: Rest the ankle. Use crutches if necessary. Ice the ankle for 20 to 30 minutes several times a day for the first 2 days. Compress by wrapping the ankle lightly -- not tightly -- with an Ace bandage or elastic ankle brace. Elevate the ankle above heart level for the first 48 hours. 2. Manage Pain and Inflammation Take ibuprofen (Advil, Motrin), acetaminophen (Tylenol), or aspirin for pain. 3. See a Health Care Provider Make an appointment as soon as possible for any ankle sprain, mild or severe. Do not give aspirin to anyone younger than 18 unless told to do so by a doctor. 18 Treating Bruises in Children Bruises are not very common in infants. They're more common on the lower legs and foreheads of toddlers just learning to walk. Call Doctor If: The bruised area seems very painful, swollen, or infected. Your child has a bruise after a serious accident or head or abdominal injury. Your child has a large number of bruises or unexplained bruises. Your child has a fever. 1. Apply Ice Wrap a cold pack in a towel or washcloth and hold it against the bruise for 10 to 15 minutes. Repeat, but no more than once an hour. Do not hold ice or anything frozen directly against a child's skin. 2. Elevate the Area If possible, raise the bruised area above the heart to reduce swelling. 3. Reduce Pain Use infant or child-formula acetaminophen (Tylenol). Don't use ibuprofen (Advil, Motrin) because it may prolong bleeding. Follow the dosing instructions on the label. If your child has never taken this medication before, call your pediatrician first. Don't give aspirin to a child under 16. 19 Treating Dehydration in Children Under 12 Years Old Call 911 if the Child: Has Extremely Dry Mouth or No Tears Is lethargic Is Older and Does Not Urinate in 12 or More Hours Isn't Alert or Able to Think Clearly Passes Out Is too Weak or Dizzy to Stand 1. Call a Doctor In young children, mild to moderate dehydration can happen very easily, particularly if the child has diarrhea or is vomiting. Contact your child's pediatrician if your child: Is not drinking enough or eating enough Looks tired Has dark yellow urine or decreased urination Has dry mouth and eyes Is cranky or irritable Vomits more than once Is under 1 year old 2. Replace Fluids For dehydration in an infant up to 1 year old: If you breast-feed, nurse more often. If you bottle feed, give your baby the usual amount of fluid, unless the baby is vomiting. If your baby is vomiting, give smaller amounts more frequently. For example, instead of 6 ounces every 4 hours, give 3 ounces every 2 hours. If she vomits more than once, call your doctor. If your baby eats solid food, cereal, strained bananas, and mashed potatoes, also provide fluids. Give an oral rehydration solution such as Pedialyte, if possible. It replaces salt, sugar, potassium, and other nutrients. Ask your doctor what type and quantity to use. For mild dehydration in a child age 1 to 11: Give extra fluids in frequent, small sips, especially if the child is vomiting. Choose clear soup, clear soda, or Pedialyte, if possible. Give popsicles, ice chips, and cereal mixed with milk for added water or fluid. Continue a regular diet. 3. Follow Up 20 For mild dehydration, have your child rest for 24 hours and keep drinking fluids, even if symptoms get better. Fluid replacement may take up to a day and a half. Continue on your child's regular diet as well. For severe dehydration, the child may need IV fluids in the hospital. If you feel, that your child is not improving or is getting worse, see your doctor right away. 21 Treating Dehydration in Adults and Children Over 12 Call 911 if the Person Has: Extreme Thirst Dry Skin, Mouth, and Mucous Membranes Little or No Urination for 12 Hours or More Increased Heart Rate and Breathing Fatigue Light-Headedness, Dizziness, or Confusion Dehydration due to heat stroke. 1. Replace Fluids For mild dehydration or while waiting for medical care for an adult with severe dehydration that is not due to heat stroke: The person should try to drink 2 quarts of rehydration drinks, water, juice, or sports drinks in 2 to 4 hours. The person should drink at least 10 glasses of liquid a day to replace lost fluids. If the person is elderly, fluid replacement may need to be done slowly. Consult a doctor. If the person is vomiting, try ice chips, popsicles, and small sips of fluid. 2. When to Call a Doctor for Mild Dehydration Seek medical help if: The person’s symptoms get worse or don’t improve within 24 hours The person is elderly You think a prescription medication such as a diuretic caused the dehydration 3. Follow Up For mild dehydration, the person should rest for 24 hours and keep drinking fluids, even if symptoms improve. Fluid replacement may take up to a day and a half. If dehydration is moderate to severe, fluids may need to be replaced intravenously (IV) in the hospital. 22 Dislocated Elbow Treatment Call 911 if the Arm: Is Deformed Cannot Be Moved after Injury 1. Don't Move the Elbow Moving the elbow or trying to put it back into place could cause more damage. 2. Treat Symptoms Apply ice to reduce swelling while waiting for medical care. Give acetaminophen (Tylenol) or ibuprofen (Advil, Motrin) for pain. 3. Follow Up The health care provider will examine the arm, check for damage to arteries and nerves, and X-ray the area to check for a broken bone or dislocation. A simple dislocation can be realigned and stabilized in an emergency room using strong pain medication and possibly sedation medication. Sometimes surgery is needed. 23