Unwritten - Personal Webpages (The University of Manchester)
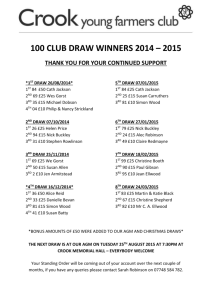
advertisement

ISBE-AstraZeneca Strategic Alliance – Work Plan - Project #43 Comparison of dynamic contrast-enhanced CT (DCE-CT) and dynamic contrast-enhanced MRI (DCE-MRI) in bladder cancer Project commencement date:May 2006 Research Project Period: to Dec 2006 Research and Supervisory Staff: GJM Parker, DL Buckley, D McGrath, B Taylor, J Logue, A Lacey Name of Supervisor: GJM Parker Programme of research work (the “Research Project”) Project Aim We will investigate the strengths and weaknesses of dynamic contrast-enhanced CT (DCE-CT) and dynamic contrast-enhanced MRI (DCE-MRI) in the investigation of bladder tumours. The study will involve 20 patients with primary bladder tumours. Each patient will be scanned with both DCE-CT and DCE-MRI, with the aim of determining tumour blood volume, blood flow, capillary wall permeability, and interstitial volume. We will also investigate the distribution of these properties within the masses, and establish correspondence between the CT and MRI information. Rationale and Background DCE-MRI is the method of choice for monitoring changes in tumour microvascular functional status due to antiangiogeneic and antivascular treatments (see for example [Jayson 2002, Morgan 2003, Jackson 2005, Jayson 2005]). However, DCE-CT is an attractive alternative as it has wider clinical availability, due to which it has attracted considerable recent interest (see for example [Sahani 2005]). DCE-MRI is known to have some advantages over DCE-CT – in particular, it is able to provide volume coverage at high temporal resolution without ionizing radiation. DCE-CT is limited in the total number of slices and number of time points during the dynamic acquisitions due to dose restrictions, which means that potentially important information from spatially heterogeneous tumours may be missed. However, DCE-MRI is thought to have some accuracy limitations due to its sensitivity to variable rates of water exchange across capillary walls [Buckley 2002, Buckley & Parker 2005]. We therefore plan to assess the following key issues in this comparison of methods: 1) Do significant differences exist between DCE-CT and DCE-MRI in the gross parameterization of tumour microvascular functional status?; If so, can these be explained by the limited volume coverage of DCE-CT, or other methodological differences (for example temporal resolution or data noise level differences), hindering the extraction of useful summary parameters? 2) Do subtle intra-tumoural regional differences exist between DCE-CT and DCE-MRI parameterizations? If so, can these be explained by variable water exchange characteristics (caused by variable capillary permeability) within the tumours that affects DCE-MRI only? Do these differences have a significant impact on the accuracy of DCE-MRI? The provision of answers to the above questions will provide guidance for the design of future therapeutic studies involving DCE methods. The identification of either DCE-CT or DCE-MRI as future methods of choice based on the quantitative study we are proposing will influence the quality of data acquired in future clinical trials, which in turn has implications for patient groups that may in future benefit from new therapeutic compounds. If DCE-CT appears inferior to DCE-MRI in our study this will avoid patients in future studies being exposed without justification to ionizing radiation. Alternatively, if DCE-CT is identified as being superior or equivalent to DCE-MRI it then has a strong case for inclusion in future trials due to its relatively high clinical availability, which will improve trial throughput and therefore potentially reduce the treatment development time scale, with associated clinical benefit. Proposed Work Plan DCE-CT scanning Volunteers will be recruited from suitable patients by J Logue at the Christie Hospital. DCE-CT (with Omnipaque 300 (Nycomed)1) will be performed at Christie Hospital (J Logue and B Taylor) Conventional CT scanning of the pelvis will also be performed without contrast agent to identify the location of the mass for the dynamic acquisition. DCE-CT scanning Volunteers will be brought to the University site (WT-CRF) within a time window of 1 week The CT information will be used to guide the DCE-MRI volume; the location of the DCE-CT slices will be incorporated within the 3D DCE-MRI imaging volume to allow optimal correspondence for comparative analysis DCE-MRI will be performed on the University of Manchester Philips Gyroscan 1.5 T system (GJM Parker, D Buckley) A standard DCE-MRI acquisition protocol will be used (high resolution T2weighted and T1-weighted (pre- and post-contrast) acquisitions plus the DCEMRI time series, which will consist of a 3D gradient echo based technique. Contrast agent will be administered as a single dose bolus injection of Omniscan (Nycomed1) for each patient. Data analysis 1 The DCE-CT and DCE-MRI data will undergo tracer kinetic modeling, which will be applied identically to both modalities. We will apply the adiabatic approximation to the tissue homogeneity (AATH) model [St. Lawrence & Lee 1998, Sahani 2005], as implemented at our site [Buckley 2002, Parker 2003, Buckley 2004, Jayson 2005] to provide estimates within the tumour mass of blood flow, blood volume, capillary permeability surface area product, and interstitial volume using each modality. These parameters will be calculated on a pixel-by-pixel basis. The DCE-CT and DCE-MRI data will be spatially aligned to allow identification of the areas of overlap between the two acquisitions. The The Nycomed products Omniscan and Omnipaque 300 will be used for this study, due to the similar molecular weights and osmotic properties of these compounds, allowing the closest possible comparison of contrast agent kinetics between the two imaging modalities. correlation between summary variables (mean, median, standard deviation) extracted from the tumour within the region of overlap will be assessed across the patient group to allow assessment of the gross agreement/disagreement between the modalities. The spatial correlation of each variable will be assessed within the region of overlap of each patient, highlighting any particular regions that may exhibit inconsistencies that may be indicative of water exchange affects in the DCEMRI data. Milestones Outputs (1) Information sought for AstraZeneca: Report on comparison Codes for data analysis Outputs (2) Publication opportunities: ISMRM conference Journals Project Management Payment Schedule Use of University Intellectual Property/third party Intellectual Property Ethical/Home Office approvals and authorisations Subject to approval of ethics committee SIGNATURE PAGE OVERLEAF Signed by Dr. Geoff Parker Signed by Dr Tony Lacey ______________________________ ______________________________ Title: Lecturer Title: Senior Informatician Date: Date: Signed by Chris Taylor Signed by Dr John Waterton ______________________________ ______________________________ Title: Professor Title: Director of Imaging Date: Date: Signed by ______________________________ Title: Date: References 1. Buckley, D. L., 2002. Transcytolemmal water exchange and its affect on the determination of contrast agent concentration. Magn. Reson. Med. 47, 420-421. 2. Buckley, D. L., 2002. Uncertainty in the analysis of tracer kinetics using dynamic contrast-enhanced T1-weighted MRI. Magn. Reson. Med. 47, 601-606. 3. Buckley, D. L., Parker, G. J. M. in Dynamic contrast-enhanced magnetic resonance imaging in oncology (eds. Jackson, A., Buckley, D. L. & Parker, G. J. M.) 69-80 (Springer, Berlin, 2005). 4. Buckley, D. L., Roberts, C., Parker, G. J. M., Logue, J. P., Hutchinson, C. H., 2004. Vascular characteristics of prostate cancer: evaluation with dynamic contrast-enhanced T1-weighted MRI initial experience. Radiol. 233, 709-715. 5. Jackson, A., Buckley, D. L., Parker, G. J. M. (eds.) Dynamic contrast-enhanced magnetic resonance imaging in oncology (Springer, Berlin, 2005). 6. Jayson, G. C., Parker, G. J. M., Mullamitha, S., Valee, J. W., Saunders, M., Broughton, L., Lawrence, J., Carrington, B., Roberts, C., Issa, B., Buckley, D. L., Cheung, S., Davies, K., Watson, Y., Zinkewich-Peotti, K., Rolfe, L., Jackson, A., 2005. Blockade of platelet-derived growth factor receptor-beta by CDP860, a humanized, PEGylated di-Fab', leads to fluid accumulation and is associated with increased tumor vascularized volume. J. Clin. Oncol. 23, 973-981. 7. Jayson, G. C., Zweit, J., Jackson, A., Mulatero, C., Julyan, P., Ranson, M., Broughton, L., Wagstaff, J., Hakannson, L., Groenewegen, G., Bailey, J., Smith, N., Hastings, D., Lawrence, J., Haroon, H., Ward, T., McGowan, A. T., Tang, M., Levitt, D., Marreaud, S., Lehmann, F. F., Herold, M., Zwierzina, H., 2002. Molecular imaging and biological evaluation of HuMV833 anti-VEGF antibody: Implications for trial design of antiangiogenic antibodies. Journal of the National Cancer Institute 94, 1484-1493. 8. Li, K.-L., Zhu, X. P., Waterton, J., Jackson, A., 2000. Improved 3D quantitative mapping of blood volume and endothelial permeability in brain tumours. J. Magn. Reson. Imag. 12, 347-357. 9. Morgan, B., Thomas, A. L., Drevs, J., Hennig, J., Buchert, M., Jivan, A., Horsfield, M. A., Mross, K., Ball, H. A., Lee, L., Mietlowski, W., Fuxius, S., Unger, C., O'Byrne, K., Henry, A., Cherryman, G. R., Laurent, D., Dugan, M., Marme, D., Steward, W. P., 2003. Dynamic Contrast-Enhanced Magnetic Resonance Imaging As a Biomarker for the Pharmacological Response of PTK787/ZK 222584, an Inhibitor of the Vascular Endothelial Growth Factor Receptor Tyrosine Kinases, in Patients With Advanced Colorectal Cancer and Liver Metastases: Results From Two Phase I Studies. J. Clin. Oncol. 21, 3955-3964. 10. Parker, G. J., Clark, D., Watson, Y., Buckley, D. L., Berrisford, C., Anderson, H., Jackson, A., Waterton, J. C., 2003. T1-weighted DCE-MRI applied to lung tumours: Pre-processing and modelling. Proc. Int. Soc. Magn. Reson. Med., 1255. 11. Sahani, D. V., Kalva, S. P., Hamberg, L. M., Hahn, P. F., Willet, C. G., Saini, S., Mueller, P. R., Lee, T.-Y., 2005. Assessing tumour perfusion and treatment response in rectal cancer with multisection CT: initial observations. Radiol. 234, 785-792. 12. St. Lawrence, K. S., Lee, T.-Y., 1998. An adiabatic approximation to the tissue homogeneity model for water exchange in the brain: 1. Theoretical derivation. J. Cereb. Blood Flow. Metabol. 18, 13651377.