INFECTION CONTROL/COMMUNICABLE DISEASES TABLE OF
advertisement

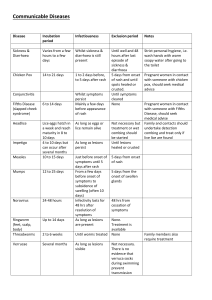
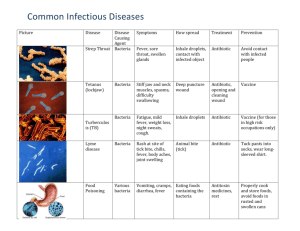
INFECTION CONTROL/COMMUNICABLE DISEASES TABLE OF CONTENTS COMMUNICABLE DISEASES: INTRODUCTION COMMUNICABLE DISEASE REFERENCE CHART COMMUNICABLE DISEASES Chicken Pox (Varicella Virus, Herpes Zoster) Common Cold Cytomegalovirus (CMV) Fifth Disease (Slapped-Cheek Disease) Hand, Foot and Mouth Disease (Coxsackievirus) Head Lice (Pediculosis) Hepatitis A Hepatitis B Hepatitis C Herpes Simplex (Cold Sore, Fever Blister) HIV/Aids Impetigo (Sand Sores) Influenza Measles (Red Measles, Rubeola) Meningitis Mononucleosis (Kissing Disease) MRSA Mumps Pink Eye (Conjunctivitis) Pinworms Ringworm Rubella (German Measles, 3-Day Measles) Scabies (Itch Mites) Staphylococcal Infections Streptococcal Infections – Group A (Scarlet Fever, Strep Sore Throat) Tuberculosis Whooping Cough (Pertussis) STANDARD PRECAUTIONS Introductions Hand washing Handling of Body Fluids Personal Hygiene Personal Contacts Environmental Factors Equipment and Supplies DIAPER CHANGING General Information Supplies Needed Procedure COMMUNICABLE DISEASES INTRODUCTION The widespread use of immunizations and antibiotics has tremendously reduced the incidence of common childhood communicable diseases and infections. However, infectious diseases do occur, and school personnel have the opportunity for early detection of the student suspected of having a communicable disease. While school personnel may not have the medical training to make a diagnosis of a specific disease, their judgment, based upon daily observations of the student, enables them to detect deviations from normal health. Student with serious communicable diseases do not always have a fever. Likewise, many students with temperature elevations above normal (100 degrees in a normal environmental setting, when quiet) may not have a communicable disease. Any of the following signs and symptoms may indicate the beginning of a communicable disease: -Temperature above 101 -Obvious rash -Repeated episodes of vomiting or diarrhea -Headache accompanied by fever, vomiting, or stiffness of neck -Prolonged cough without history of asthma Once the classroom teacher has identified a student suspected of having a communicable disease, it is their responsibility to bring it to attention of the school nurse/administrator who should then evaluate and contact the parent/guardian. Administrators are required to notify the Supervisor of School Health Services, who will notify the local Department of Health immediately by telephone of suspected cases of measles, rubella, pertussis, haemophilus influenza, hepatitis A, diphtheria, or poliomyelitis. The Department of Health must be notified by the next business day of recognition of any suspected conditions involving mumps, hepatitis B and C, and chicken pox. Administrators should be aware that, in the event of a communicable disease outbreak, the Department of Health may declare a communicable disease emergency and initiate outbreak control measures. A communicable disease emergency outbreak can include cases of immunizable diseases such as measles, diphtheria, rubella (German measles), pertussis (whooping cough), poliomyelitis, haemophilus type b flu, mumps, and chicken pox. If there is noncompliance with the actions requested, the Department of Health may invoke quarantine powers, which could lead to the removal of children without proper immunization documentation or with medical/religious exemptions or, in case of a child care center, to eventual closure. Most students recover uneventfully from communicable disease. However, there are groups of students who are at risk for serious, sometimes fatal, complications. This includes students who are undergoing steroid or other immunosuppressive therapy (including Chemo, or transplantation), students with sickle cell disease or other chronic diseases those who have a generalized malignancy (i.e., leukemia), or those who have an immunologic disorder. School personnel who are aware of such students have the responsibility of informing the parents of recent outbreaks of communicable diseases in order to prevent their exposure to students with the disease. In most cases, the student is kept out of school until the outbreak is over. 1 COMMUNICABLE DISEASES INTRODUCTION (continued) It is inevitable students will get sick. Diseases can spread easily in schools because large numbers of students from different families spend hours together in one place. The problem school staff encounter involve keeping one student’s illness from spreading through the school to the other students, their families, and staff. Factors that contribute to the spread of disease include: -Inadequate hand washing or use of hand sanitizer -Large number of students in one room -Small room size relative to the number of children -Limited bathroom facilities -Staff who circulate among different age groups -Staff who work with children as well as handle food -Failure of staff to observe good hygiene -Failure to segregate a sick student or staff member Additional factors to consider with early childhood populations are: -Mixing diapered students with students not in diapers -Failure to use good diapering practice -Students placing objects in mouth 2 COMMUNICABLE DISEASE REFERENCE CHART The following are general recommendations involving uncomplicated cases. Contacts without symptoms need not stay home from school, unless so advised by their healthcare provider. DISEASE CHICKEN POX - Virus INCUBATION PERIOD Range 14 to 16 days, sometimes as early as 10 days, or as late as 21 days after contact. MODE OF TRANSMISSION Direct contact with persons with disease; occasionally thru airborne respiratory secretions; contact with fluid from lesions. By direct oral contact or by respiratory droplets: spread indirectly by hands and articles freshly soiled by discharges of nose and throat of an infected person. By direct person to person contact with virus-containing secretions (excreted in urine, saliva, breast milk, cervical secretions, and semen); mother to infant before, during, or after birth. Direct contact with respiratory secretions. COMMON COLD – Virus Range 12 to 72 hours, usually 48 hours CYTOMEGALOVIRUS(CMV)-Virus Unknown, but appears to be 3 to 12 weeks FIFTH DISEASE- Virus Range 4 to 20 days HAND, FOOT, MOUTH DISEASE – Virus Range 3 to 6 days Direct contact with respiratory secretions, blister fluid and stool of infected person. HEAD LICE – Parasite Lice can survive only 1 to 2 days away from the scalp. Incubation period of louse egg is 6 to 10 days. Direct head to head contact or through any object used by infected person (comb, hat, towel, clothing etc.). 3 MAY RETURN TO SCHOOL 6 days after onset of rash, or if all lesions are crusted over. Student should rest at home if elevated temperature, too uncomfortable to attend school, or repeated sneezing and coughing. Upon written recommendation of the healthcare provider. Exclusion from school not indicated, as they are not contagious. Student should rest at home if elevated temperature or too uncomfortable to attend school. Exclusion from school is not necessary if student has no symptoms. When student is nit free. Our “No nit” policy requires that student be accompanied by parent on return to school. COMMUNICABLE DISEASE REFERENCE CHART (CONTINUED) DISEASE HEPATITIS A – Virus INCUBATION PERIOD Range 15 to 50 days (average: 28 days) HEPATITIS B – Virus Range 45 to 160 days (average:120 days) HEPATITIS C – Virus Range 14 to 180 days (average: 45 days) HERPES SIMPLEX – Virus Range 2 to 12 days HIV-AIDS – Virus Variable, ranging from months to years MODE OF TRANSMISSION Ingestion of fecal matter. Close personto-person contact and ingestion of contaminated food and drinks. Person to person via sexual contacts, contaminated IV needles (drug use), blood and blood products, and mother to baby. Person to person via sexual contacts, contaminated IV needles (drug use), blood and blood products, and mother to baby. Direct contact with virus in saliva of infected person; contact with fluid from blisters; sexual contact. Predominantly via; 1) Sexual contact 2) Exposure to contaminated needles or other sharp instruments (commonly drug use); 3) Mother-to-infant transmission before or during birth, or breastfeeding; and 4) Blood/blood products. 4 MAY RETURN TO SCHOOL Should be excluded from school for one week after onset of illness. When symptom free and written recommendation from healthcare provider. When symptom free and written recommendation of healthcare provider. Should not be excluded from school. When possible, lesions that are not yet crusted should be covered. Attendance permitted. Refer to Pinellas County School Board Policy. COMMUNICABLE DISEASE REFERENCE CHART (CONTINUED) INFLUENZA – Virus Direct contact, coughing sneezing, hand to mouth, or articles freshly soiled with discharges from nose and throat of infected persons Range 8 to 12 Airborne by droplet or days by direct contact with nasal secretions of infected person from 4 days before rash to 4 days after appearance of rash. Varies REPORT CASES TO SCHOOL HEALTH SERVICES AND SCHOOL NURSE FOR SPECIFIC RECOMMENDATIONS. For Meningitis: Severity of disease and risk of exposure differs greatly depending on the causative agent. Risk is greatest to those people that have close/intimate contact. Range 4 to 6 Contact via saliva. weeks Kissing increases the risk/spread of disease among young adults. May also be transmitted via blood transfusion. 5 days after onset of symptoms or when active signs of illness are no longer present. MRSA - Bacterial Variable, as long as lesions continue to drain. Autoinfection continues for the period of nasal colonization or duration of active lesions. Direct skin-to skin contact or contact with shared items or surfaces with infected person. MUMPS – Virus Range 12 to 25 days(average: 16 to18 days) Direct contact via respiratory route. Exclusion from school and sport activities should be reserved for those with wound drainage that cannot be covered and contained with a clean, dry bandage and those who cannot maintain good personal hygiene. 5 days after onset of swelling. MEASLES-Virus MENINGITIS – Bacterial or Viral MONONUCLEOSIS Virus Range 1 to 3 days 5 7 days after onset of rash and written recommendation from health care provider. Upon written recommendation of healthcare provider. Upon written recommendation of healthcare provider. PINK EYE (CONJUNCTIVITIS)Bacterial or Viral PINWORMS – Parasite Bacterial: 24 to 72 hours. Viral: 12 hours to 3 days Incubation from egg to worm 1 to 2 months. Eggs become infective within a few hours on the skin. Eggs can remain infective indoors for 2 to 3 weeks. Contact with discharge from eyes. Direct transfer of eggs from anal area to mouth, most frequently due to ineffective hand washing. May also be result of ingestion of contaminated dirt, raw vegetables or indirectly from clothing and bedding etc. Because of their small size pinworm eggs can become airborne and ingested while breathing. Direct skin to skin contact with infected humans, animals, and objects (ex., combs, floors, clothing, etc.) RINGWORM- Fungus Range 4 to 21 days RUBELLA – Virus German Measles 3 –day Measles Range 12 to 23 days Direct contact with respiratory secretions from infected person. SCABIES - Parasite Usually 2 to 6 weeks before onset of itching Direct personal contact with infected untreated person. STAPHLOCCOCAL INFECTIONS – Bacteria Variable and undetermined Direct contact. with drainage from open lesions or airborne from a cough of infected person. 6 Not necessary to isolate/exclude student. Advise medical care. Exclusion not required. Encourage good hand washing. Refer student to healthcare provider for treatment No need to exclude. Must be covered while in school. Exception: Ringworm of scalp requires oral medication and written recommendation of healthcare provider. May return 7 days after onset of rash and with written recommendation from health care provider Exclude student until after treatment with prescription medication. After treatment has started and sores are no longer draining. Depending on the diagnosis return to school may require written recommendation of healthcare provider. DISEASE STREPTOCOCCAL INFECTIONS – Bacteria Scarlet fever Strep throat TUBERCULOSISMycobacteria INCUBATION PERIOD Variable: usually 1 to 5 days MODE OF TRANSMISSION Direct or indirect contact with respiratory or wound secretions. MAY RETURN TO SCHOOL 24 hours after treatment with antibiotic with written recommendation of the healthcare provider. 2 to 10 weeks for disease Spread by airborne droplet from infected people by cough, sneeze or forcibly exhaled air. Upon written recommendation of health provider. Close contact with an infected person via coughing and sneezing (respiratory secretions) 5 days after initiation of treatment with an antibiotic and written recommendation of healthcare provider. Note: Positive TB skin test may not indicate presence of active disease, but does require follow-up with healthcare provider. WHOOPING COUGH (PERTUSSIS) Bacteria Range 4 to 21 days Average 7 to 10 days 7 CHICKEN POX (VARICELLA, HERPES ZOSTER) DEFINITION A highly contagious viral disease; rarely fatal, but has been a frequent antecedent of Reye’s syndrome. INCUBATION PERIOD Usually 14 to 16 days; some cases occur as early as 10 or as late as 21 days after contact. PERIOD OF COMMUNICABIITY Most contagious for 1 to 2 days before and shortly after the onset of the rash, and until all lesions are dry and scabbed over. MODE OF TRANSMISSION From person to person by direct contact, droplet or airborne spread of secretions. Indirectly through articles freshly soiled by discharges from vesicles and mucous membranes of infected person. STUDENT COMPLAINTS OR OBSERVABLE SIGNS Slight fever Malaise Severe itching Rash rapidly progresses from red spots to a pimple-like sore which open, drain and crust over. Rash starts on chest, back, arms or neck. NOTE: AVOID USE OF ASPIRIN IN CHILDREN AND ADOLESCENTS TO PREVENT REYE’S SYNDROME. PREVENTION AND CONTROL Preventable with immunization. Current recommendations are for a two dose series of varicella vaccine for persons older than 12 months of age. Exclude from school for one week after eruption first appears or until vesicles become dry. Standard Precautions for all articles soiled by discharge from nose, throat or lesions. RETURN TO SCHOOL May return to school 6 days after onset of rash or if all lesions/sores have crusted over. 8 SHINGLES (ZOSTER OR HERPES ZOSTER) DEFINITION A virus that stays dormant in the body after a person recovers from chickenpox. For reasons that are not fully known, the virus can reactivate years later, causing a painful rash. MODE OF TRANSMISSION Shingles cannot be passed from one person to another. However, the virus that causes shingles, the varicella zoster virus, can be spread from a person with active shingles to a person who has never had chickenpox. In such cases, the person exposed to the virus might develop chickenpox, but they would not develop shingles. The virus is spread through direct contact with fluid from the rash blisters. PERIOD OF COMMUNICABILITY A person with shingles can spread the virus when the rash is in the blister-phase. A person is not infectious before blisters appear. Once the rash has developed crusts, the person is no longer contagious. Shingles is less contagious that chickenpox and the risk of a person with shingles spreading the virus is low if the rash is covered. STUDENT COMPLAINTS OR OBSERVABLE SIGNS Shingles usually starts as a painful rash on one side of the face or body. The rash forms blisters that typically scab over in 1-7 days and clears up within 2-4 weeks. Before the rash develops there is often pain, itching or tingling in the area where the rash will develop. This may happen anywhere from 1-5 days before the rash appears. Other symptoms of shingles can include: Fever Headache Chills Upset stomach PREVENTION AND CONTROL The only way to reduce the risk of developing shingles is to get vaccinated. A vaccine for shingles is licensed for persons aged 60 years and older. RETURN TO SCHOOL No exclusion as long as the rash is covered with no drainage. 9 COMMON COLD DEFINITION Fever is common in children. Tearing, irritated nose and throat, chilliness, coughing lasting 2 to 7 days. INCUBATION PERIOD Between 12 to 72 hours, usually 48 hours. MODE OF TRANSMISSION Presumably, by direct oral contact or by droplet spread. Indirectly by hands and articles freshly soiled by discharges of nose and throat of an infected person. PREVENTION AND CONTROL Avoid crowded living and sleeping quarters. Education in hand washing, coughing or sneezing into your sleeve, and proper disposal of used tissues. RETURN TO SCHOOL Student should rest at home if temperature of 101 degrees or greater, with persistent coughing/sneezing, or too uncomfortable to attend school. 10 CYTOMEGALOVIRUS (CMV) DEFINITION An infection which rarely produces symptomatic disease. The most severe form occurs from congenital infection. Approximately 18% may result in learning disabilities, or physical disabilities such as hearing loss. Infection later in life can cause a mononucleosis-like illness. INCUBATION PERIOD Unknown, but appears to be 3 to 12 weeks. PERIOD OF COMMUNICABILITY Virus may be excreted in urine or saliva for months or years. MODE OF TRANSMISSION Through intimate contact with virus-containing secretions, such as urine, saliva, breast milk, cervical secretions and semen. Mother to infant before, during, or after birth. STUDENT COMPLAINTS OR OBSERVABLE SIGNS Fever Sore throat Swollen lymph nodes May have no complaints or observable signs PREVENTION AND CONTROL Immunization – None Standard Precautions with frequent hand washing. RETURN TO SCHOOL Upon written recommendation of healthcare provider. 11 FIFTH DISEASE (SLAPPED –CHEEK DISEASE) DEFINITION A common disease of school children characterized by a red rash on the cheeks, followed by a lacy rash on the arms and legs. It usually causes very little illness, although adolescents sometimes have mild joint pain or swelling. INCUBATION 4 to 20 days PERIOD OF COMMUNICABILITY Uncertain, but appears to be 1 week before rash. MODE OF TRANSMISSION Presumably direct contact by infected respiratory secretions. STUDENT COMPLAINTS OR OBSERVABLE SIGNS Brief period of elevated temperature, may include headache Rash first appears on face and cheeks---slapped face appearance After first day, red spots appear on extremities with lace-like appearance. Rash fades but may recur for 1 to 3 weeks on exposure to sunlight or heat. PREVENTION AND CONTROL Immunization – None Standard Precautions Measures to control spread by infected respiratory secretions are recommended. Include frequent hand washing and proper disposal of tissues. Pregnant teachers and immunosuppressed students should avoid contact with infected students. Strict hand washing after patient contact. RETURN TO SCHOOL Exclusion from school not indicated, as they are not contagious once rash appears. WARNINGS Children with blood problems, such as sickle cell disease, and those with certain cancers or on chemotherapy can develop severe anemia, usually without a rash. Pregnant women, in contact with an infected child between 3 days and 2 weeks before the rash, should speak with their doctor. Blood tests to check for immunity or infection are available. Fortunately, most adults have had exposure to Fifth Disease (parovirus) during childhood and are no longer at risk of catching the illness. 12 HAND, FOOT AND MOUTH DISEASE (COXSACKIEVIRUS) DEFINITION Most coxsackie viral infections in humans are mild but can produce a variety of illness. INCUBATION PERIOD Usually 3 to 6 days PERIOD OF COMMUNICABILITY During the acute stage of illness and perhaps longer, since these viruses persist in stool for several weeks. MODE OF TRANSMISSION Direct contact with infected respiratory secretions and stool of infected persons. STUDENT COMPLAINTS OR OBSERVABLE SIGNS Fever Sore throat Oral lesions which may persist from 7 to 10 days. These lesions also occur commonly on the palms, fingers and soles. Occasionally, lesions appear on the buttocks. PREVENTION AND CONTROL Standard Precautions Reduce person to person contact. Frequent hand washing and cleaning of shared items. Specific treatment – none RETURN TO SCHOOL Student should rest at home if elevated temperature, persistent drooling or too uncomfortable to attend school. No exclusion is necessary if no symptoms present. 13 HEAD LICE (PEDICULOSIS) DEFINITION Head lice are parasites which infest human hair, articles of clothing and upholstered furniture. Head lice pose no great threat to the general public health but cause considerable public and personal annoyance. INFECTIOUS AGENT The fertile louse lays her eggs at the base of the hair shaft, cementing each egg (nit) on the hair shaft. After 6 to 10 day period the egg hatches, producing a nymph, which requires a blood meal within 24 hours. The nymph undergoes a molt and after 7 to 10 days, becomes an adult louse. In her 30 day lifetime, an adult female will produce 50 to 300 eggs. MODE OF TRANSMISSION Head lice cannot fly or jump, but they use hooked legs to crawl rapidly. They are not transmitted by household pets, but can be transmitted by sharing hats, clothing and personal items. Their presence does not indicate an “unclean” head or home. METHODS OF CONTROL All lice and eggs (nits) on the hair and in the environment must be destroyed. The infestation and reinfestation cycle must be broken by destroying lice through: shampooing of hair with lice shampoo, wash clothing and bedding in hot water and placing in dryer on hot cycle. Non-washable household items (toys and stuff animals, etc.) must be dry cleaned, vacuumed, or “bagged” (in well-sealed plastic bags) for a minimum of 2 weeks. Lice can survive in the environment for 1 to 2 days. Nits hatch in 6 to 10 days but can be dormant for up to 35 days. Pinellas County Schools has a No-Nit Policy A No-Nit Policy calls for The removal of all lice (including nits and egg cases) following application of a lice-killing product. The exclusion of a student from school until such measures have been successfully accomplished. Education to ensure that parent/guardian understands their responsibilities under the No-Nit Policy. Information in hand outs and lice letters to be sent home with student and class. Advantages of a No-Nit Policy Encourages home screening. Eliminates diagnostic confusion. Helps prevent self-re -infestation and transmission. Reduces or eliminates the need for subsequent treatment. 14 HEAD LICE(continued) PEDICULOSIS SCREENING PROCESS Target Population 1. Students, who exhibit the following signs or symptoms of head lice and have suspected infestations, as reported by their classroom teacher, should be examined by school personnel trained in identifying an infestation of head lice. - Student complains of intense head itching. Student is observed scratching head frequently. Reddish papules or tiny bite marks may be present on the neck. A close examination of the scalp will reveal small whitish eggs firmly attached to hair shaft especially at the nape of the neck, above the ears, and frequently on the crown. Although dandruff may resemble eggs, dandruff can easily be removed from the hair. The louse egg is attached to the hair with cement secreted by the louse and cannot easily be removed. 2. When a case of head lice is confirmed, all students who are close associates of the infected student and infected student’s siblings should be examined by trained school personnel. If the student changes classes during the day, a large number of potential contacts may need to be inspected. Process 1. All students found to have head lice should be excluded from school for treatment. Parent/guardian should be notified by school personnel (not volunteers) to pick up the student as soon as possible. 2. When a case of head lice is found in a classroom, lice-alert notes should go home on the day of the exam by school personnel. 3. Parent/guardian should be provided current, accurate impartial information to assist with the treatment process. 4. Treatment and return to school should occur in a timely manner. 5. Parent/guardian should be instructed to come into the school with their lice and nit-free student for a re-admission check. 6. If family circumstances or financial constraints prevent compliance, the Department of Health will provide treatment shampoo at a reasonable cost. 7. If the re-admission check shows evidence of continued infestation (visible lice and/or nits), the parent should be instructed to take the student home and complete the removal of all lice and nits and re-treat clothing and household items. 8. Should the re-examination reveal a few nits that were missed after treatment at home, these can be removed and allow the student to remain in school. 9. When a student is temporarily excluded from school due to head lice infestation, the parent/guardian should be reminded to check everyone in the family and to inform parents/guardians of playmates who may not be students at the school. The parent/guardian should also be advised to check the family for 2 to 3 weeks and then regularly as part of routine home hygiene. NOTE: Parent/guardian MUST accompany child for re-entry head check. 15 HEAD LICE (continued) PREVENTING TRANSMISSON AT SCHOOL 1. At the beginning of school, notify parents/guardians of the school policy, reminding them to check their students regularly and requesting that they send their students to school lice/nits free. Parent/guardian should also be encouraged to report cases of lice in their families to the school. 2. Students can be educated by teachers and parent/guardian not to share coats, scarves, hats, helmets, combs, brushes, hair ribbons, head bands, pillows, ear pieces or other personal items. Head-to-head contact should be avoided. 3. Assigned lockers are the preferred storage for outside clothing. If hooks are used for coats, jackets and sweaters, they should be at least 12 inches apart. If crate-type storage bins are used, students should be encouraged to place towels and clothing inside plastic bags before putting into bins. 4. Caps, gloves and scarves should be stored in individual bags marked with the student’s name and kept at the individual desk. Allow students to hang their jackets on the backs of their seats. 5. School buses should be monitored to keep personal articles separated. 6. Unlike fleas, lice do not live and breed in the environment. However, it is important to vacuum carpets daily (especially where students take naps on carpet flooring using towels or mats), upholstered surfaces, tumbling mats, etc. for the removal of nits. Vacuuming is always a desirable alternative to spraying. Though they usually feed every 3 to 5 hours, lice are capable of surviving about 48 hours without a host. Nits are capable of hatching within 6 to 10 days if the environmental temperature remains constant. 7. In P.E. classes, changes of transmission can be lessened by any of several methods that keep clothing separated: Number all clothes hooks and assign a hook to one student for each period. Assign lockers to one student for each period. Note: Several students may use the same hook of locker during the day, but the numbers of persons at risk will be narrowed to only those few students. If hooks and lockers were used at random, the whole class would be at risk. 8. Students may be more likely to contract lice if they sit on the floor with other students, if they share a table instead of sitting in an individual desk, and if they share headsets for classroom activities. Headsets should be carefully checked before use and cleaned with alcohol as needed. 9. Students who ride crowded buses and those with long hair may be more susceptible. 10. With public attention currently focused on student safety and the quality of student’s health care, the school health program would be incomplete without addressing pediculosis. Because of its highly communicable nature, all students are vulnerable to local outbreaks. The negative effects they suffer range from the discomfort and social stigma of lice to the loss of valuable class time and repeated exposure to potentially toxic pesticidal shampoos and sprays. In turn, families and school communities are victimized by anxiety, frustration, anger and confusion that often accompany pediculosis outbreaks. Our message to parent/guardian must center on the importance of learning how to diagnose and treat head lice properly and on scheduling family head checks as part of routine home hygiene. 16 HEPATITIS A DEFINITION An inflammation of the liver caused by a virus usually resulting in jaundice (yellowish skin and eyes) and, in some instance, liver enlargement. INCUBATION PERIOD 15 to 50 days, average 28 days. PERIOD OF COMMUNICABILITY During the latter half of t he incubation period and continuing for a few days after onset of jaundice. MODE OF TRANSMISSION Person to person via contact with stool of infected person and taken in by mouth (usually a result of ineffective hand washing). Less often spread by swallowing food or water that contains the virus. RISK GROUPS Children in daycare, people who eat raw shellfish, and travelers. STUDENT COMPLAINTS OR OBSERVABLE SIGNS Fever Malaise Loss of Appetite Nausea Abdominal discomfort After a few days, may exhibit jaundice (skin and white of eyes turn yellow) PREVENTION AND CONTROL Standard Precautions Hand washing is the most important preventive practice. Immunization with Hepatitis A Vaccine – recommended for all children at age 1 year RETURN TO SCHOOL Most cases are noninfectious after the first week of jaundice. Student may return to school upon written recommendation of healthcare provider. 17 HEPATITIS B DEFINITION A viral infection of the liver that can become chronic. Symptoms include loss of appetite, vague abdominal discomfort, nausea, vomiting, and often progressing to jaundice (yellowish coloring of skin and eyes). Mild fever may be present, but some people have the disease without observable symptoms. INCUBATION PERIOD Usually: 45 to 160 days, average 120 days. PERIOD OF COMMUNICABILITY During the incubation period and acute stage of the disease. Some persons become chronic carriers of the virus and may be infectious for years to life. MODE OF TRANSMISSION Transmission is primarily sexual and from exposure to blood and body fluids and mother to baby. STUDENT COMPLAINTS OR OBSERVABLE SIGNS Fever Malaise Loss of appetite Nausea Abdominal discomfort After a few days, may exhibit jaundice (skin and white of eyes turn yellow) PREVENTION AND CONTROL Use of Standard Precautions is essential Immunization is required for students for school entrance and available for some staff Frequent hand washing practice is always advisable Since the Hepatitis B virus can live outside the body on surfaces for an indefinite time (days), cleaning of all exposed surfaces with an EPA-approved disinfectant is recommended. RETURN TO SCHOOL May return to school upon written recommendation of healthcare provider. 18 HEPATITIS C DEFINITION A viral inflammation of the liver. INCUBATION PERIOD Range of 14 to 180 days, average 45 days PERIOD OF COMMUNICABILITY From one or more weeks before onset of the first symptoms throughout the acute course of the disease and indefinitely in the chronic carrier stages. MODE OF TRANSMISSION Exposure to contaminated blood through IV drug use, sexual contact, or mother to baby. STUDENT COMPLAINTS OR OBSERVABLE SIGNS low-grade fever nausea or vomiting weight Loss fatigue joint pain or muscle pain headaches abdominal pain and cramps (right upper quadrant) May be followed by jaundice (yellowish coloring of skin or eyes) and dark urine. PREVENTION AND CONTROL Use of Standard Precautions are essential. Immunization is not available at this time. Blood donor screening RETURN TO SCHOOL May return to school upon written recommendation of healthcare provider. 19 HERPES SIMPLEX (COLD SORE, FEVER BLISTER) DEFINITION Viral lesions that form on the face and lips which crust and heal within a few days. INCUBATION PERIOD Range 2 to 12 days PERIOD OF COMMUNICABILITY Usually brief (3 days) until lesions crust. MODE OF TRANSMISSION Direct contact with virus in saliva of infected person, contact with fluid from blisters, and infected respiratory secretions. STUDENT COMPLAINTS OR OBSERVABLE SIGNS Cluster of painful, 1mm to 2mm bumps or blisters on the outer lip Often appear only on one side of the mouth PREVENTION AND CONTROL Use of Standard Precautions Frequent hand washing Personal hygiene and health education Immunization- None available Suggest limiting student’s contact with newborns, children with eczema, or immunosuppressed students Do not allow sharing of objects that are placed in mouth RETURN TO SCHOOL Students with herpes simplex should not be excluded from school. When possible, lesions that are not crusted should be covered. 20 HIV/AIDS (HUMAN IMMUODEFICIENCY VIRUSES/ ACQUIRED IMMUNEDEFICIENCY SYMDROME) DEFINITION HIV- The Human Immunodeficiency Virus (HIV infection). It is the virus that can lead to acquired immune deficiency syndrome, or AIDS. AIDS – HIV may be in the body for many years before there are signs of the illness. As HIV weakens the immune system, symptoms may appear and other illnesses may occur. Acquired Immune Deficiency Syndrome (AIDS) represents the most severe end of the disease spectrum. MODE OF TRANSMISSION HIV is mainly spread through sexual intercourse (vaginal, oral, and anal); sharing needles for drug use, steroids, or other blood rituals with an HIV-infected person; and from HIV-infected mothers to their infants before, during or after birth (through breast feeding). HIV is not spread through day to day activities, such as sharing cooking/eating utensils, shaking hands, hugging, casual kissing, toilet seats, food, pets, or mosquitoes. INCUBATION PERIOD The window period of time it takes a person’s body to create HIV antibodies after being infected is approximately 6 months. A person who has been infected with HIV, but does not yet test positive for the virus, can transmit the virus to others. The incubation period refers to the length of time between becoming infected with the virus and being diagnosed with AIDS. It is variable, ranging from months to years. A person can be infected with HIV for many years before any signs of illness develop. PERIOD OF COMMUNICABILITY From the time of infection with the HIV virus STUDENT COMPLAINTS OR OBSERVABLE SIGNS The signs and symptoms may vary from asymptomatic to severe. 2 or more signs/symptoms need to be present in adolescents and children. -fever -loss of appetite/failure to thrive -weight loss -chronic fatigue -skin rashes -swollen lymph glands -night sweats -hepatitis -recurrent upper respiratory tract infections -chronic /recurrent diarrhea -recurrent bacterial and viral infections PREVENTION AND CONTROL use of Standard Precautions abstinence from drug use and sex safe sex- latex condoms during each and every sexual encounter (vaginal, oral or anal) RETURN TO SCHOOL Student may not be excluded due to diagnosis of HIV/AIDS School personnel are to maintain strict confidentiality. See Pinellas County School Board Policy 11/11 21 IMPETIGO (SAND SORES) DEFINITION Bacterial infection which causes skin lesions/sores which begin as small blisters which break and form yellow crusts. INCUBATION PERIOD Variable: range is commonly 1 to 10 days. PERIOD OF COMMUNICABIITY While sores are draining. MODE OF TRANSMISSION Spread by direct contact with drainage from open sores or nasal secretions. STUDENT COMPLAINTS OR OBSERVABLE SIGNS Onset of small red skin blisters. Pustules form, open and discharge fluid, which forms crusts. Multiple lesions/sores are common. These can rapidly spread to other areas of the body. May complain of itching PREVENTION AND CONTROL Use of Standard Precautions Regular personal hygiene. Refer to healthcare provider for antibiotic treatment RETURN TO SCHOOL May return 24 hours after treatment with topical or oral antibiotics. Areas with lesions/sores should be covered (band aid) during school hours. 22 INFLUENZA DEFINITION This is an acute viral disease of the respiratory system with seasonal patterns in the winter months most common. INCUBATION PERIOD Usually 1 to 3 days. PERIOD OF COMMUNICABILITY From 1 day before symptoms to 7 days after symptoms MODE OF TRANSMISSION Spread through air by coughing, sneezing, hand to mouth or nose discharge of infected persons. STUDENT COMPLAINTS OR OBSERVABLE SIGNS stuffy nose, sore throat, cough muscle pain, headache, fatigue fever- It is important to note that not everyone with the flu will have a fever. nausea, vomiting, diarrhea NOTE: AVOID USE OF ASPIRIN IN CHILDREN AND ADOLESCENTS TO PREVENT REYE’S SYNDROME. PREVENTION AND CONTROL Use of Standard Precautions. Immunization is recommended for people of all ages. Recommend measures to control spread of droplet infections-coughing, sneezing, and proper disposal of tissues. Recommend frequent hand washing. RETURN TO SCHOOL May return 5 days after onset of symptoms or when active signs of illness are no longer present. If fever was present, at least 24 hours after fever is gone. 23 MEASLES (RED MEASLES, RUBEOLA) DEFINITION An acute, highly communicable viral disease INCUBATION PERIOD Symptoms usually begin 8 to 12 days after exposure to the virus. PERIOD OF COMMUNICABILITY From 4 days before the beginning of cold symptoms until 4 days after appearance of the rash. MODE OF TRANSMISSION Spread by airborne droplet infection and direct contact with nasal or throat secretions of infected persons. STUDENT COMPLAINTS OR OBSERVABLE SIGNS 3-4 days of red eyes, runny nose, fever and cough before the rash begins. Pronounced blotchy red rash starting on the face and spreading downward over the entire body. Rash can last from 3 to 7 days. White specks (Koplik’s spots) on the buccal mucosa of the mouth. Especially near the molars. PREVENTION AND CONTROL Required immunization given after the age of one year, with booster before kindergarten. Older children or adults may receive a booster dose at any age. When a case of measles is reported, contact Pinellas County Schools Health Services Supervisor for further instructions. RETURN TO SCHOOL 7 days after onset of rash with written recommendation of healthcare provider. 24 MENINGITIS (BACTERIAL or VIRAL) DEFINITION Inflammation of the meninges that may be caused by either a virus (rarely a serious disease) or bacteria (more serious). VIRAL MENINGITIS DEFINITION A relatively common, but rarely serious, form of meningitis. Viral meningitis no longer requires reporting to the Department of Health. INCUBATION PERIOD/ PERIOD OF COMMUNICABILITY Vary with specific viral causative agent MODE OF TRANSMISSION Most commonly spread by respiratory secretions of person with a recent viral infection. STUDENT COMPLAINT OR OBSERVABLE SIGNS Early symptoms are very similar to the more serious bacterial form of meningitis, and include: abrupt onset with fever, chills, headache light sensitivity may have back or neck stiffness PREVENTION AND CONTROL No immunization available for viral form of meningitis Use of Standard Precautions Avoid sharing food, drink, utensils and cigarettes. RETURN TO SCHOOL Upon written recommendation of healthcare provider. BACTERIAL MENINGITIS DEFINITION Meningococcal meningitis is an acute bacterial disease. It requires early diagnosis and prompt, aggressive antibiotic treatment in the individual in order to prevent serious complications and possible death. INCUBATION PERIOD Varies from 2 to10 days, commonly 3 to4-days. PERIOD OF COMMUNICABILITY Until meningoccocci bacteria are no longer present in discharges from nose and mouth, usually within 24 hours after appropriate treatment started. 25 BACTERIAL MENINGITIS (continued) MODES OF TRANSMISSION By direct contact, including respiratory secretions, saliva, and discharges from nose and throat of infected persons. Healthy carriers may also be the source of infection. STUDENT COMPLAINT OR OBSERVABLE SIGNS Abrupt onset with fever, chills, headache, back or neck stiffness and vomiting, quickly followed by changes in alertness, consciousness or orientation to person, place, or time. Extreme irritability and agitation. Seizures may occur. Neck stiffness may be marked. PREVENTION AND CONTROL Use of Standard Precautions Vaccine against invasive meningococcal disease is recommended for children aged 2 – 11 years of age for certain high-risk groups and for all persons aged 11 years and older. Avoid sharing food, drinks, utensils, cigarettes, etc. Household and intimate contacts of the infected person may be at higher risk of exposure to develop the disease. Contact Pinellas County Schools Health Services supervisor with any reported/suspected cases of Bacterial Meningitis for investigation and further directions. RETURN TO SCHOOL Upon written recommendation of healthcare provider. 26 MONONUCLEOSIS (KISSING DISEASE) DEFINITION A viral infection most commonly caused by the Epstein-Barr virus.Ninety percent (90%) of the people who have mononucleosis are asymptomatic. In children, it is generally mild and difficult to recognize. INCUBATION PERIOD Range: 4 to 6 weeks. PERIOD OF COMMUNICABILITY Indeterminate: prolonged as communicability may exist for a year or more after the infection. MODE OF TRANSMISSION Virus is spread from person to person via saliva. Kissing and sharing drinks, utensils, etc. increases the spread of disease. STUDENT COMPLAINT OR OBSERVABLE SIGNS fatigue sore throat fever nasal congestion enlarged lymph nodes A skin rash may occur, especially in young children and those taking ampicillin. PREVENTION AND CONTROL Use Standard Precautions Immunization – None available Education regarding transmission Sanitary disposal of articles soiled with nose and throat discharges Medical evaluation of symptoms Report to school personnel. RETURN TO SCHOOL Upon written recommendation of healthcare provider. Return to active physical activity should also be under recommendation of healthcare provider. 27 MRSA (METHICILLIN-RESISTANT STAPHYLOCOCCUS AUREUS) DEFINITION A bacterial skin infection, which must be treated with appropriate antibiotics. INCUBATION PERIOD Variable and indefinite PERIOD OF COMMUNICABILITY As long as wounds/lesions continue to drain. MODE OF TRANSMISSION Direct skin- to- skin contact with draining lesion or contact with shared items or surfaces with infected person. STUDENT COMPLAINTS OR OBSERVABLE SIGNS Skin infections or sores which may be red, swollen, painful, and/or have pus or other drainage. PREVENTION AND CONTROL Use of Standard Precautions Wash hands frequently and thoroughly with soap and water. Antibiotic therapy as prescribed by healthcare provider. Clean all surfaces and equipment used by infected person with 1:10 bleach solution (1 part bleach and 9 parts water that would be 1 2/3 cups of chlorine bleach in 1 gallon of water) daily. Keep sores clean and covered and dry at all times until healed. Do not share personal items like towels, washcloths, clothing or sports equipment. Avoid contact with wounds or soiled bandages. RETURN TO SCHOOL Student may return to school after being treated by a healthcare provider. Wounds must be covered and have no drainage through bandage. 28 MUMPS (PAROTITIS) DEFINITION An acute viral disease characterized by fever and swelling and tenderness of one or more salivary/parotid glands. INCUBATION PERIOD Range 12 to 25 days with an average of 16 to 18 days. PERIOD OF COMMUNICABILITY Usually 1-2 days, but has been reported to be as long as 7 days before swelling appears and until 9 days after. MODE OF TRANSMISSION Virus is spread by direct contact with airborne or droplets of respiratory secretions or saliva. STUDENT COMPLAINTS OR OBSERVABLE SIGNS Swollen tender salivary/parotid gland, in front of the ear and crossing the corner of the jaw under the chin. Pain increased by jaw movement- such as eating, chewing, talking Fever (over 100 Fahrenheit) PREVENTION AND CONTROL Use of Standard Precautions Immunization with single vaccine or combination vaccine with rubella and measles (MMR) after 1 year of age- 2nd dose prior to kindergarten (older children and adults are recommended to receive a 2nd dose at any age). Report to Pinellas County Schools Health Services supervisor for further investigation and directions. RETURN TO SCHOOL May return to school 5 days after onset of swelling. 29 PINK EYE (CONJUNCTIVITIS) DEFINITION An acute, highly-contagious infection of one or both eyes. May be a viral or bacterial infection. INCUBATION PERIOD Bacterial: 24-72 hours Viral: 12 hours to 3 days PERIOD OF COMMUNICABILITY During course of active infection. MODE OF TRANSMISSION Contact with discharges from the conjunctivae or upper-respiratory tract of infected person. STUDENT COMPLAINTS OR OBSERVABLE SIGNS Redness of the white part of the eye Redness of eyelids White or yellow discharge Crusting at corners of the eye and along eyelashes Sensitivity to light PREVENTION AND CONTROL Use of Standard precautions. Immunization - none Good and frequent hand washing practices. Discourage sharing eye make-up and applicators. RETURN TO SCHOOL Infected students should be allowed to remain in school once indicated therapy is implemented, except when viral or bacterial conjunctivitis is accompanied by systemic signs of illness. 30 PINWORMS DEFINITION A very common, but not serious, parasitic infection. INCUBATION PERIOD Life cycle requires 2-6 weeks to be completed. Symptomatic disease usually evident some months after initial exposure. Egg to worm 1 to 2 months. Eggs become infective within a few hours on the skin. Eggs can remain infective indoors for 2 to 3 weeks. PERIOD OF COMMUNICABILITY As long as gravid females are discharging eggs on perianal skin, usually about 2-6 weeks. MODE OF TRAMSMISSIONS Direct transfer of eggs from anal area to mouth, most frequently due to ineffective hand washing or ingestion of infested dirt. Indirectly through clothing, bedding, or food contaminated with eggs or parasite. STUDENT COMPLAINTS OR OBSERVABLE SIGNS The child may awaken during the night complaining of itching around the anal area. The itching causes scratching which contaminates the hands with eggs, especially under finger nails. Females may develop irritation around the vulva or vagina. PREVENTION AND CONTROL Refer to healthcare provider for treatment. Frequently, all household members are treated. Education in personal hygiene and particularly in proper hand washing techniques after toileting and before eating. RETURN TO SCHOOL Does not require exclusion from school. 31 RINGWORM DEFINTION It is a contagious disease of the hair, nails and skin. INCUBATION PERIOD Range: 4 to 21 days PERIOD OF COMMUNICABILITY As long as active lesions/sores are present. MODE OF TRANSMISSION Skin contact with infected humans, animals, and objects (combs, floors, clothing, etc.) STUDENT COMPLAINTS OR OBSERVABLE SIGNS Ring-shaped pink patch with scaly, raised border. Ring slowly increases in size. May be mildly itchy. Cracking of the skin, especially between the toes. PREVENTION AND CONTROL See healthcare provider for treatment Education regarding personal hygiene and general cleanliness in showers, dressing rooms, and other common areas. Treatment may be topical or oral route- specific drugs for fungal infections RETURN TO SCHOOL No need to exclude. Affected area should be covered (band aid) during school hours. EXCEPTION: Ringworm of the scalp requires oral medication, therefore written recommendation of the healthcare provider is required for return to school. 32 RUBELLA (GERMAN MEASLES, 3 DAY MEASLES) DEFINITION A mild, febrile viral infection characterized by rash, swollen glands, and slight fever INCUBATION PERIOD Range: 12 to 23 days PERIOD OF COMMUNICABILITY One week before and at least 5 to 7 days after onset of rash. MODE OF TRANSMISSION Virus is spread by contact with nose and throat secretions or by direct contact with articles freshly soiled. Highly contagious. STUDENT COMPLAINTS OR OBSERVABLE SIGNS Widespread pink-red spots usually starting on face and spreading down to cover body within 24 hours, not lasting more than 3 days. Enlarged lymph nodes at base of neck and/or behind ears (appears 5-10 days before rash begins) Mild fever May complain of sore throat; no cough. PREVENTION AND CONTROL Use Standard precautions Immunization required- 2 MMRs after the age of 12 months and before entry to kindergarten. Avoid exposure of susceptible pregnant women and immunosuppressed children to infected individuals. School staff of childbearing age should be immunized to prevent the risk of congenital rubella damage to their own unborn children. Report to Pinellas County Schools Health Services supervisor for investigation and directions. RETURN TO SCHOOL May return 7 days after onset of rash and with written recommendation of from healthcare provider. 33 SCABIES (ITCH MITES) DEFINITION An infectious disease caused by a mite that burrows under the skin. Highly contagious. INCUBATION PERIOD Usually 2 to 6 weeks before the onset of itching. Persons with previous infestations develop symptoms 1 to 4 days after re-exposure. MODE OF TRANSMISSION Direct, prolonged, skin to skin contact with a person who is infested. STUDENT COMPLAINTS OR OBSERVABLE SIGNS Intense itching usually becomes unbearable at night. Small red, raised lesions with associated tunnels. Found in folds of the skin: between fingers, waist line, and groin region. PREVENTION AND CONTROL Students with reddened, itching skin should be sent to the health room area for inspection. Because scabies is highly contagious, it is recommended that gloves be worn by school personnel when touching the skin, followed by thorough hand washing. Advise student to be seen by healthcare provider for diagnosis and treatment. Exclude infested individual from school until treated Wash down classroom and clinic area that may have been touched by the student with a disinfectant; vacuum carpeted areas; wash towels and clothing used by infected person in hot water. RETURN TO SCHOOL Once treated by prescribed medication (usually one day) and with written recommendation of healthcare provider. 34 STAPHYLOCOCCUS INFECTIONS DEFINITION Bacteria commonly carried on the skin or in the nose of healthy people. Staph bacteria can cause infections which can be minor (pimple) or serious (see MRSA). INCUBATION PERIOD Variable and undetermined PERIOD OF COMMUNICABILITY Variable depending on the infection. MODE OF TRANSMISSION Direct contact with drainage from lesions or airborne from a cough of infected person. STUDENT COMPLAINTS OR OBSERVABLE SIGNS Skin infections or sores which may be red, swollen, painful and/or have pus or other drainage. See MRSA information for severe infections. PREVENTION AND CONTROL Cover wound Standard precautions Good hand washing technique Do not share personal items See healthcare provider for treatment. Antibiotic therapy may be required RETURN TO SCHOOL After treatment has started and sores are no longer draining. Depending on the diagnosis return to school may require written recommendation. 35 STREPTOCOCAL INFECTIONS – GROUP A (SCARLET FEVER, STREP SORE THROAT) DEFINITION A variety of acute communicable diseases. INCUBATION PERIOD Variable: Usually 1 to 5 days. PERIOD OF COMMUNICABILITY 10-21 days without adequate antibiotic treatment; only 24 hours with antibiotic treatment MODE OF TRANSMISSION Results from direct or intimate contact with patient’s or carrier’s respiratory secretions. Indirect contact through objects or hands is rare. STUDENT’S COMPLAINTS OR OBSERVABLE SIGNS Abrupt onset of high fever, increased pulse rate, vomiting, headache, and chills. Tonsils become enlarged, reddened, and covered with white patches. Tongue may have appearance of strawberry skin. Rash may appear within 12 hours. Severe and sudden sore throat without coughing, sneezing or other cold symptoms. PREVENTION AND CONTROL Use of Standard Precautions. Isolation and exclusion of students with a rash, pending diagnosis. RETURN TO SCHOOL After 24 hours of antibiotic treatment begins and written recommendation from healthcare provider. 36 TUBERCULOSIS (TB) DEFINITION Pulmonary tuberculosis is an infectious disease of the lungs. INCUBATION PERIOD 2 to 10 weeks for disease. PERIOD OF COMMUNICABILITY If untreated, as long as the infectious tubercle bacilli are being discharged. MODE OF TRANSMISSION Spread by airborne droplet produced when infected people cough, sneeze or forcibly exhale. STUDENT COMPLAINTS OR OBSERVABLE SIGNS Positive skin test does not represent presence of disease, but does require follow-up with healthcare provider. May include cough, pain and tightness in the chest, fever, loss of appetite with weight loss. PREVENTION AND CONTROL Use of Standard Precautions Notify Pinellas County Schools Health Services supervisor for investigation and directions. RETURN TO SCHOOL Only with approval of Department of Health and upon written recommendation of healthcare provider. 37 PERTUSSIS (WHOOPING COUGH) DEFINITION This is an acute bacterial infection of the respiratory tract. Whooping cough is characterized by a prolonged period of respiratory symptoms progressing to prolonged episodes of coughing that end with a “whooping ” sound, which may be followed by vomiting. INCUBATION PERIOD 4 to 21 days, usually 7-10 days. PERIOD OF COMMUNICABILITY From 6 days after exposure to 3 weeks after onset of respiratory symptoms. MODE OF TRANSMISSION Close contact with an infected person via coughing, sneezing, respiratory secretions. STUDENT COMPLAINTS OR OBSERVABLE SIGNS Begins with symptoms of upper respiratory infection. Persistent dry hacking cough that becomes more severe, especially at night. Characteristic series of short rapid coughs often followed by high-pitched whoop and vomiting. PREVENTION AND CONTROL Use of Standard Precautions Required immunization- completed 4-5 doses of DPT/DTaP prior to entering kindergarten, with booster of Tdap before entering 7th grade. Education regarding the effectiveness of early immunization (DTaP.) Wash thoroughly all articles soiled with discharges from nose and throat of infected individuals. Antibiotics can shorten the period of communicability but not length or severity of illness. Notify Pinellas County Schools Health Services supervisor for investigation of any possible cases. RETURN TO SCHOOL Upon the written recommendation of the healthcare provider 5 days after beginning antibiotic therapy. 38 STANDARD PRECAUTIONS INTRODUCTION People who work in the educational setting encounter a wide variety of illnesses daily. The common cold, flu, chickenpox, and many other contagious diseases are spread from person to person routinely. Bloodborne pathogens, especially those which cause HIV (Human Immunodeficiency Virus) and HBV (Hepatitis B) present an additional health risk to school district employees. This covers some of the facts concerning bloodborne diseases which can be used to help protect employees against contracting them in the workplace. By exercising the proper precautions against infection, the risk to an employee’s health is minimal. WHAT ARE BLOODBORNE PATHOGENS? Bloodborne pathogens are disease-carrying microorganisms which are present in human blood or other body fluids which can cause several serious diseases such as: HIV/AIDS HBV/Hepatitis B Hepatitis C WHAT SHOULD I KNOW ABOUT THESE DISEASES? HIV/AIDS attacks the body’s immune system, thereby allowing infections to invade the body. HBV is much more easily transmitted than HIV, because it is a stronger and more concentrated virus HIV and HBV are transmitted through direct contact with blood or other body fluids. The usual routes of entry are by mucous membranes, broken skin or puncture by an infected object. They cannot be spread by casual contact (i.e. sharing of work space, using same tools, telephones, or rest rooms) They cannot be spread by hugging, touching, or shaking the hand of an infected individual WHAT IS THE RISK OF WORKPLACE EXPOSURE? Contact with the blood or body fluids of another individual presents the greatest risk of exposure. “Exposure Incidents” occur when the mucous membranes or broken skin of an individual come in contact with the blood of another. The chances of being infected with bloodborne diseases in the educational workplace are small if proper precautions are taken. WHAT PRECAUTIONS SHOULD I TAKE? Use STANDARD PRECAUTIONS – handle all blood and other body fluids as if they were infected. Components of Universal Precautions include: 1. Personal protective equipment e.g. gloves 2. Frequent hand washing using disinfectant soap or antiseptic towelettes. 3. Decontamination- clean contaminated surfaces with 1:10 bleach solution 4. Waste Disposal- dispose of contaminated waste properly. HAND WASHING IS THE MOST EFFECTIVE WAY TO REDUCE THE SPREAD OF DISEASE 39 HAND WASHING HAND WASHING IS CONSIDERED ONE OF THE MOST EFFECTIVE INFECTION CONTROL METHODS. When to wash your hands? Before and after contact with wounds- even though you wear gloves Before and after procedures Before giving medicine Between contact with all patients (students and staff) Before eating After toileting How to Wash your hands Wet hands thoroughly by holding them under running water. Hold your hands lower than your elbows so that the water flows from arms to fingertips. Use warm water. Apply soap to hands. Use firm, rubbing, circular movements. Wash palm, back and wrist of each hand Interface fingers and thumbs and move hands back and forth for 10-15 seconds. Good hand washing should take about 15 seconds- about the time it takes to sing “Happy Birthday to You”. Dry hands and arms thoroughly with paper towels. Turn off water using paper towels to prevent picking up bacteria from the handles. 40 HANDLING OF BODY FLUIDS PURPOSE In order to prevent transmission of infectious agents, such as HIV, Hepatitis B, staph, CMV, etc, personnel must consider ALL blood, blood products, and body fluids potentially infectious. Potentially infectious body fluids include: vomit, oral secretions, sputum, urine, feces, wound drainage, mucus. EQUIPMENT (As needed) 1. Disposable gloves 2. Masks 3. Paper gowns- moisture resistant 4. Eye protection 5. Puncture-resistant containers 6. Impermeable bags 7. Disinfectant PROCEDURE 1. Gloves must be worn whenever blood or other body fluids are handled. 2. Paper gowns, masks and/or eye protection will be worn for procedures that may involve splashing or spraying of body fluids. 3. Hands will be washed thoroughly after removing gloves and immediately after contact with ANY body fluid. When running water is unavailable, hands should be washed with a waterless hand wash, e.g. (62% alcohol-based hand sanitizer), followed by soap and water ASAP. 4. Vomit will be cleaned up by HPO following their procedure. Gloves are supplied for this. Any disinfecting by the nurse will be done with disinfectant solution. 5. Disposable needles and syringes will be placed in a puncture-resistant sharps container or use disintegrators after use. DO NOT RE-CAP, BEND OR CUT NEEDLES. 6. Potentially-infected waste must be placed in plastic bags and covered containers, securely tied prior to disposal. 7. For assistance with sharps containers call: Gerry Lees at 547-7100. PERSONAL HYGIENE 1. Hand washing is the keystone of good hygiene. a. Facilities should be readily available to the classroom. b. Soap should be in a dispenser. When classroom facilities are not available 62% alcohol-based waterless hand sanitizer should be used. c. Hands should be washed between handling children, before eating and handling food and after handling items which have been soiled. 2. Take special care of cuts, burns, or breaks in the skin. Gloves should be worn if these are present. 3. Use disposable paper towels to dry hands and turn off faucets. PERSONAL CONTACTS 1. Kissing and mouth-to-mouth sharing of food, toys and learning aids should be discouraged. 2. Each student should have his/her own personal toiletry items such as toothbrush, comb, rest-mat, dishes and utensils. Disposable eating items are preferred. 41 ENVIRONMENTAL FACTORS 1. Changing tables should have a washable surface and be sanitized with 1:10 bleach solution between students. Disposable examining table paper should also be used. 2. All surfaces involved in food handling should be sanitized at least one time per day, with 1:10 bleach solution. 3. The use of disposable non-sterile gloves is required when contact with blood, other body fluids (vomit, urine, feces), mucous membranes, or handling items or surface soiled with body fluids is anticipated. Double gloving is recommended if a large amount of blood is present. Gloves should be changed after contact with each student. 4. Toys, learning materials, musical instruments, equipment, etc, should be washed daily with 1:10 bleach solution ( 1 tbsp. chlorine bleach in 1 quart of water), and thoroughly rinsed after exposure to saliva (through mouthing toys or drooling). 5. Tiled floors that are contaminated with body fluids should be wet mopped/scrubbed immediately. If Blood, please see HPO procedure. 6. Carpeting contaminated with body fluids should be shampooed immediately. 7. When appropriate, maintain a change of clothing for each child and change the child’s clothing if it has become soiled by vomit, excrement, nasal secretions or extensive drooling. Employees are encouraged to keep a change of clothes available. Areas of skin where body fluids have soaked through, clothing needs to be washed thoroughly with soap and water ASAP. 8. Require plastic pants or long pants for children with diarrhea. Current guidelines state that a student who has more than 2 episodes of diarrhea at school should be sent home early. 9. Diapers, cleaning rags/towels, gauze pads and other materials that are soiled should be discarded in closed plastic bags, stored in bio-hazard storage area, and properly disposed. 10. Hands must be washed thoroughly after removing gloves and immediately after contact with any body fluid. When running water is unavailable, hands should be washed with a waterless hand cleaner (e.g. Cal Stat) followed by soap and water scrub ASAP. EQUIPMENT AND SUPPLIES 1. A dishwasher should be used to sterilize dishes with water temperature between 120-140 degrees. 2. A washer and dryer should be available for soiled clothes and cleaning materials. Clothes soiled with body secretions should be laundered separately. Gloves should be used when handling laundry. 3. Use disposable items when possible (e.g. latex gloves, dishes and utensils, paper towels, examining table paper, face masks). 4. Use washable mats and rugs. 5. Have an approved disinfectant solution available. Compliance with these Standard Precautions is the responsibility of all PCSB employees. Failure to implement these guidelines in everyday work situations may result in disciplinary action. RESOURCE: PCSB Risk Management Department 42 DIAPER CHANGING GENERAL INFORMATION 1. There should be an area separate from each classroom designated for diaper changes. This diaper area could be partitioned from the rest of the classroom or be a separate room, such as the bathroom with a changing table. A sink is recommended in the diaper changing area. No other activities, such as feedings, play, or therapy, should be conducted in this area. 2. It is recommended that the sink used for hand washing after diaper changes or toileting not be the same sink that contains food items such as dishes, wash cloths or water drinking fountains. If only one sink is available to a classroom, all dishes should be collected in a plastic dishpan and carried to the central kitchen for cleaning in an automatic dishwasher. 3. It is highly recommended that the person designated to change a student’s diapers not be the same person involved in any feeding activities of other students. If this cannot occur, close attention to good hand washing is essential. 4. It is the responsibility of the school staff to promote good skin care, including regular diaper changes, while the student is at school. 5. If the student is able, he/she should be encouraged to assist in gathering supplies, carrying the clean diaper or helping with the removal of the diaper. If the student assists with any part of the diaper changing, he/she must wash his/her hands before and after the procedure. Any assistance by the student will enhance his/her self-esteem, make the procedure less embarrassing and aid in progress towards personal care independence. 6. All students should was their hands after toileting. 7. All diapers should be checked every two (2) hours, and BM changes should occur immediately to prevent skin irritations. There could be circumstances when this schedule would be altered due to field trips and other activities. A reasonable alternative plan should be developed for these special occasions. It is suggested that students in diapers have toilet logs. SUPPLIES NEEDED 1. 2. 3. 4. 5. 6. 7. Clean diaper Towelettes, or wet, soapy paper towel Toilet paper Small plastic bag Table, paper and disinfectant Gloves Step-on covered trash can with plastic bag liner 43 DIAPER CHANGING (continued) PROCEDURE 1. Wash hands. 2. Assemble supplies and place clean paper on changing table. 3. Assist or take student to changing area or bathroom. 4. Place student on changing table. DO NOT LEAVE STUDENT UNATTENDED 5. Be sensitive to the fact that some students are uncomfortable with the height of the table or embarrassed by the procedure. 6. Put on gloves. 7. Remove soiled or wet diaper and immediately place in plastic bag and then in trash can. 8. Do not place a wet or soiled diaper on the table, floor, or sink. 9. Remove loose BM with toilet paper. Wash the skin of the genital area gently with antiseptic towelettes, soapy water, or wet paper towels. 10. Dry the area well. Over-the-counter diaper creams, lotions, or powders need a physician’s order. 11. Apply a clean diaper 12. Remove gloves and dispose of in trash can. 13. Secure outer clothes 14. Assist student off the changing table. DO NOT LEAVE STUDENT IN BATHROOM OR CHANGING AREA ALONE. 15. Wash hands of child and self. 16. Clean table with 1:10 bleach solution. 17. Return supplies to designated areas, and put clean table paper in place. 44