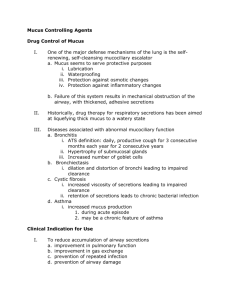
Bronchiectasis

Bronchiectasis
Normal lungs
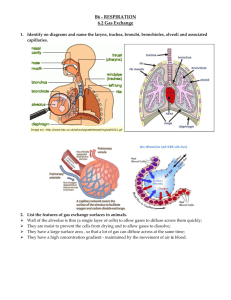
Air is carried into your lungs through a series of branching tubes
(airways, or bronchi). The airway walls produce a small amount of mucus which keeps your lungs moist and traps the dust and germs that you breathe in. The mucus is then normally moved upwards by tiny hairs (cilia) which line the tubes and waft the mucus to your throat, from where it is usually swallowed, unnoticed.
What is bronchiectasis?
This is a chronic condition in which some of your airways have a corrugated lining instead of a smooth lining. Mucus tends to collect in these little pockets.
Chronic means that it is longterm. However, it usually doesn’t get worse, so long as you keep yourself out of this vicious cycle :
Damaged airways
Inflammation Stagnant mucus
Infected mucus
What is the cause of bronchiectasis?
There are several known causes including:
Severe infection such as childhood pneumonia, whooping cough or measles, which can leave scarring in your airways.
Sometimes, inhalation of a small object such as a peanut earlier in life.
Occasionally, lack of immunity to infection, for example a lack of antibodies (proteins in your blood which neutralise viruses and bacteria) which occasionally happens if you get a severe virus infection.
However, over half the people with bronchiectasis in the UK have no obvious cause for it.
What are the symptoms?
The most common symptom is coughing up sputum, often in large amounts, every day. This is tiring and can be a nuisance socially.
Some people with bronchiectasis get short of breath. One third have long-term sinusitis.
Less common symptoms are coughing up blood (haemoptysis) or chest pain.
Bronchiectasis is sometimes associated with inflammatory bowel disease or rheumatoid arthritis, which are also inflammatory diseases.
How is it diagnosed?
If you have a persistent cough, producing infected sputum, some of the following tests may be done:
a high-resolution CT scan (which is painless) to identify damaged airways,
a test of your sputum to see if bacteria are present, which identifies which antibiotics may help,
a bronchoscopy, in which a small, flexible telescope (a bronchoscope) is inserted through your nose and into your lungs, under sedation, to have a closer look at your airways,
blood tests and a test to see how much salt is present in your sweat
(this identifies cystic fibrosis),
How is it treated?
1. You will need to work with your doctor to ensure timely and accurate antibiotic treatment if you get a chest infection, which will work on the
INFECTED MUCUS part of the vicious cycle :
Damaged airways
Inflammation Stagnant mucus
INFECTED MUCUS
2. You will need to work with your physiotherapist to develop a daily chest clearance regime that keeps your lungs pristine without interfering with your daily life more than necessary, which works on the STAGNANT MUCUS part of the vicious cycle :
Damaged airways
Inflammation STAGNANT MUCUS
Infected mucus
3. Some drugs can help loosen your mucus, but optimum fluid intake (2 litres a day) should be tried first.
4. Daily exercise will encourage your cilia to work in order to move the mucus upwards.
5. Some people find that adding 5 drops of tea tree oil to a bowl of boiling water, and inhaling the steam, helps prevent infections.
6. Very occasionally, surgery is used to remove the affected part of the lung, but only if the disease is localised and very troublesome.
7. Nasal drops and sprays can help if you have a nose or sinus infection.
Alexandra Hough, Respiratory Physiotherapist, www.alexhough.com
, 01323 638615