OSTEOPATHY AND CARDIOVASCULAR DISEASE
advertisement

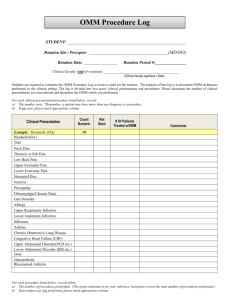
OMM #32 Wed., 10/22/03 1 pm Dr. Glenn Chapman Kirandeep Brar Page 1 of 11 OSTEOPATHY AND CARDIOVASCULAR DISEASE Dr. Chapman spoke directly from the ppts. Any additional comments I’ve put in italics. I. Objectives The role of O.M.M. in the management of the cardiac patient Describe the anatomy of the CV system, including the sympathetic and parasympathetic innervation to the heart Describe the viscerosomatic and somatovisceral reflexes of the cardiac system Compare the anginal and musculoskeletal presentations and mechanisms of chest pain Describe the presentation of myocardial infarction in terms of viscerosomatic reflexes Discuss the approach for osteopathic manipulative treatment of the cardiac patient II Management of Cardiac Patient Nonpharmacological: diet, increase exercise, stress reduction, smoking cessation, weight reduction, restrict sodium Pharmacological: Beta Blockers, Diuretics, ACE inhibitors, Calcium Channel Blockers Diet – HDL, LDL and Total Cholesterol – Unsaturated, Saturated and trans fatty acids. Source of trans fatty acids is margarine. So avoid cooking with margarine! – Increase intake of Omega-3 fatty acids – Antioxidants: Carotenoids, Vit. C, Vit. E, Selenium. Pneumonic: “ACES”. Another antioxidant is Coenzyme Q. – Minimize NaCl. Only 10% of pts are sensitive to salt. But ones that have HTN, salt will exacerbate their condition. – Diet rich in K+, Ca ++, Mg ++ Physical activity – Landmark Framingham Study: enhanced levels of fitness associated with lower risk of heart disease – Proven light to moderate activity associated with lower coronary heart disease rates – Proven: over one hour of walking per week predicts lower risk of heart disease. Person who is FIT reduces their risk of heart disease. Fitness is defined as 10, 000 steps taken/day. Stress Reduction – Sympathetic Stimulation: Goal to decrease it Activation of sympathetic outflow to skeletal muscle blood vessels: HTN; heart, OMM #30 Wed., 10/21/03 1 pm Dr. Glenn Chapman Kirandeep Brar Page 2 of 11 lung, kidney most likely to contribute to LVH. – Psychological Abnormalities: panic disorders, depression, stress – Yoga, meditation, tai-chi Smoking – Major risk factor for CV disease – Multiple mechanisms interact with atherosclerosis, vascular injury, thrombosis, vascular dysfunction – Quitting: Behavioral therapy, stepdown approach with patches and gums, acupuncture, pharmacologic. Pt must have desire to quit otherwise none of these methods will really work. Weight reduction – Increased activity – Decreased caloric intake – Pharmacologic: Sibutramine, Ephedra – Surgical: Gastric stapling, lap banding – Behavioral: Biofeedback, hypnotism Pharmacological – Beta Blockers: attenuates sympathetic input (decrease HR, BP, and contractility) st – Diuretics (1 line of treatment): Decrease intravascular volume (decreases filling pressure, ventricular volume and wall tension), increase sodium excretion – ACE inhibitors: Arteriolar dilatation (reduces afterload), venodilation (reduces preload), increase cardiac output, induces natriuresis – Calcium Channel Blockers: Smooth muscle relaxant (decrease SVR), antispasmotic, slow AV conduction (Verapamil only) – Other: Nitrates, Digoxin, Antiarrhythmics, III. Hypertension 90% Primary (Essential) Hypertension 2:1 for African Americans: Caucasians. Manyt African Americans are sensitive to salt. – No definable cause – Essentially don’t know what causes it 10% Secondary Hypertension – Renal Artery Stenosis, Pheochromocytoma, OCP, Cushing’s Disease Essential Hypertension – Hyper activity to sympathetic stimuli – Prolonged sympathetic stimuli to kidneys creates functional retention of water and salt plus elevated arterial pressure – Inappropriate increased systemic vascular resistance (SVR) Goal - Break the sympathicotonia cycle and delay stage of fixed HTN OMM Treatment OMM #30 Wed., 10/21/03 1 pm Dr. Glenn Chapman Kirandeep Brar Page 3 of 11 – – – – – – – OA Release: increase Vagal output Rib Raising: inhibitory (attenuate facilitation) Cervicals: carotid baroreceptors, cervical ganglions Thoracolumbar junction: renals and RAS Chapman’s Reflexes: myocardium, adrenals CV4: fluid homeostasis and decrease stress Myofascial Trigger Points: mobilize fluids IV. Arrhythmias Sinus tachycardia, sinus bradycardia, SVT, A Fib, VT, VF, AV blocks Goal: Reduction of segmental facilitation in the upper thoracics and modify vagal tonicity OMM Treatment – Vagal stimulation: OA release, globe pressure, carotid massage, valsalva maneuver (ask pt to bear down, easy way to do this is to ask pt to put hand to mouth and blow), Erben’s reflex (strong forward bending of head) – Thoracics: T1-6, T12-L2 – Myofascial Trigger Points: esp. Pectoralis and Sternalis V. CHF Definition: inability of heart to pump enough blood to meet oxygen requirements of body Causes: MI, valvular disease, HTN, cardiomyopathies Importance: 3 to 40 times resting amount of lymphatic return challenging the system. Extravasation of fluid causing pulmonary and peripheral edema In many cases, CHF is due to musculoskeletal abnormalities. Therefore Cardiac Rehab is recommended. It is shown to be twice as effective as ACE Inhibitors. OMM treatment – Lymphatic Pump: fluid mobilization – Diaphragmatic Techniques: abdominal and thoracic – Effluerage: mobilize peripheral fluid – Clavicular releases: promote thoracic duct drainage – CV4: fluid homeostasis and decrease stress – of course: OA, thoracics, lumbar, Chapman pts, fascia VI. Ischemic Heart Disease Atherosclerotic Coronary Artery Disease (ASCAD) - endothelial damage progressing to an obstructive lesion Two Basic Stages – Stable angina - coronary atherosclerosis – Unstable angina - non Q wave MI, Q wave MI, ischemic sudden cardiac death OMM #30 Wed., 10/21/03 1 pm Dr. Glenn Chapman Kirandeep Brar Page 4 of 11 Goal: calm the sympathetic hyperactivity to lower incidence of ectopic foci, arrhythmias, prevent MI, encourage collateral circulation, potentiate medical management OMM treatment – T2-5 Left: Indirect techniques to attenuate facilitation (esp. T2-3 Left in anterior wall MI) – OA: vagal normalization (esp. inferior wall MI) – Chapman points: myocardium, renals, lungs – Ribs and accessory muscles of respiration: decrease cardiac workload – Gait: abnormality can increase cardiac work up to 300%. EX: something as simple as a heal lift can decrease a patient’s work load. Myocardial Infarction and OMT- A decrease in mortality and morbidity after OMT OMM #30 Wed., 10/21/03 1 pm Dr. Glenn Chapman Kirandeep Brar Page 5 of 11 VII. Post Midline Sternectomy Secondary to CABG Presents as increased pain due to disruption of sternum, ribs Goal: Increase movement of ribs, respiratory dynamics, increase lymphatic drainage OMM Treatments: rib raising, balanced ligamentous tension, lymphatic Pump, clavicular releases, diaphragmatic release, OA release VIII. Anatomy of CV System Sympathetic Innervation to the Heart – T1-6 – Right and left sided distribution – Right side: Right deep cardiac plexus – Left side: Left deep cardiac plexus and SA node and AV node Sympathetics of the Heart OMM #30 Wed., 10/21/03 1 pm Dr. Glenn Chapman Kirandeep Brar Page 6 of 11 IX. Anatomy of CV System Hypersympathetic activity – Right = affects SA node = SVT – Left = affects AV node = ectopic foci, VF – Arrythmias, increase force of heart beat, shorten time of systole, increase ventricular output, increase rate of contraction – Coronary vasospasm and vasoconstriction – Inhibits development of collateral circulation, – Decreased lymphatic drainage Parasympathetic Innervation to the Heart – Cranial Nerve X (Vagus) – Right and Left sided distribution – Right side= SA node – Left side= AV node Parasympathetics of the Heart OMM #30 Wed., 10/21/03 1 pm Dr. Glenn Chapman Kirandeep Brar Page 7 of 11 Hyperparasympathetic activity – Right: SA node = sinus bradyarrythmias – Left: AV node = AV blocks Lymphatics – Right lymphatic duct: heart, lungs, liver, right upper limb, head and neck right brachiocephalic approximately 80% but much variation to this head and neck = right jugular trunk heart, lungs, liver = right bronchomediastinal trunk right limb = right subclavian trunk – Left lymphatic duct: rest of body left jugular, left subclavian, left bronchomediastinal, left thoracic duct X. Lymphatic Drainage Kirandeep Brar Page 8 of 11 XI. Viscerosomatic and Somatovicersal Reflexes Reflex - an involuntary nervous system response to a sensory input Viscerosomatic Reflex - localized visceral stimuli producing patterns of reflex response in segmentally related somatic structure Physical findings: – Areas of facilitation: a theory regarding the neurophysiological mechanisms underlying the neuronal activity associated with somatic dysfunction, ie T2-T5 left, tenderness, hyperirritability, tissue texture changes, increased muscle tension, or limitation of motion Referred pain via cardiac viscerosensory reflex from the coronary arteries: – Radiates to upper half of left chest – neck and jaw – down arm Chapman’s Reflex - a system of reflex points used by Frank Chapman Chapman’s Reflexes - Reflexes present as predictable anterior and posterior tissue abnormalities assumed to be reflective of visceral dysfunction or pathology OMM Treatment – Indirect techniques – CV4 – OA via ME MI Pain Referral Pattern OMM #30 Wed., 10/21/03 1 pm Dr. Glenn Chapman Kirandeep Brar Page 9 of 11 Somatovisceral Reflexes – Localized somatic stimulation producing patterns of reflex in segmentally related visceral structures Pectoralis Trigger Points: located in the right pectoralis major muscle, between the5th and 6th ribs, between the sternal margin and nipple line. Resulting in a supraventricular tachyarrythmia Treatment: Jones Strain-Counterstrain Arrhythmia Trigger Point Anginal vs Musculoskeletal CP OMM #30 Wed., 10/21/03 1 pm Dr. Glenn Chapman Kirandeep Brar Page 10 of 11 XII. Anginal vs Musculoskeletal CP Stable angina – Presentation: heaviness, pressure, burning, squeezing, smothering, choking – Typically caused by exertion, or emotion, and relieved by rest or sublingual Nitroglycerin Unstable angina – Basically any change, new onset angina, angina at rest for first time, increasing severity or duration or frequency Variant (Prinzmetal’s) angina – Due to transient coronary vasospasm – Hallmark is transient ST segment elevation Linked angina – Esophageal acid stimulation significantly reduces coronary blood flow in patients with CAD via a viscero-visceral reflex Musculoskeletal Chest Pain – Costochondral and costosternal articulations are the most common sites. – Direct pressure at articulations will reproduce pain and is essential part of CP workup – Pain may be darting, last a few seconds, or a dull ache lasting hours or days – Tietzes Syndrome: redness and swelling with pain at the costosternal junction Myocardial infarction – WHO diagnostic criteria for acute MI requires at least 2 of the following criteria a clinical history of ischemic type chest discomfort changes on serial ECG elevation of cardiac enzymes Viscerosomatic Reflex physical findings – VS Reflex pain from coronary arteries classically described as Radiating upper half of left chest referral out and down the inner surface of arm and hand to the tips of fingers refer up the neck and into the jaw – Palpatory findings Areas of acute facilitation = acute, warm, boggy, edematous, T1-T5 Left Viscerosomatic Reflex physical findings – Chapman reflex points anterior second intercostal space tender point in myofascial tissue with hyperirritability, increased sweat gland activity, spasm and vasoconstriction – Trigger Point right pectoralis muscle between the 5th and 6th ribs midway between the sternal margin and the nipple line