Super Cereal Recipes
advertisement
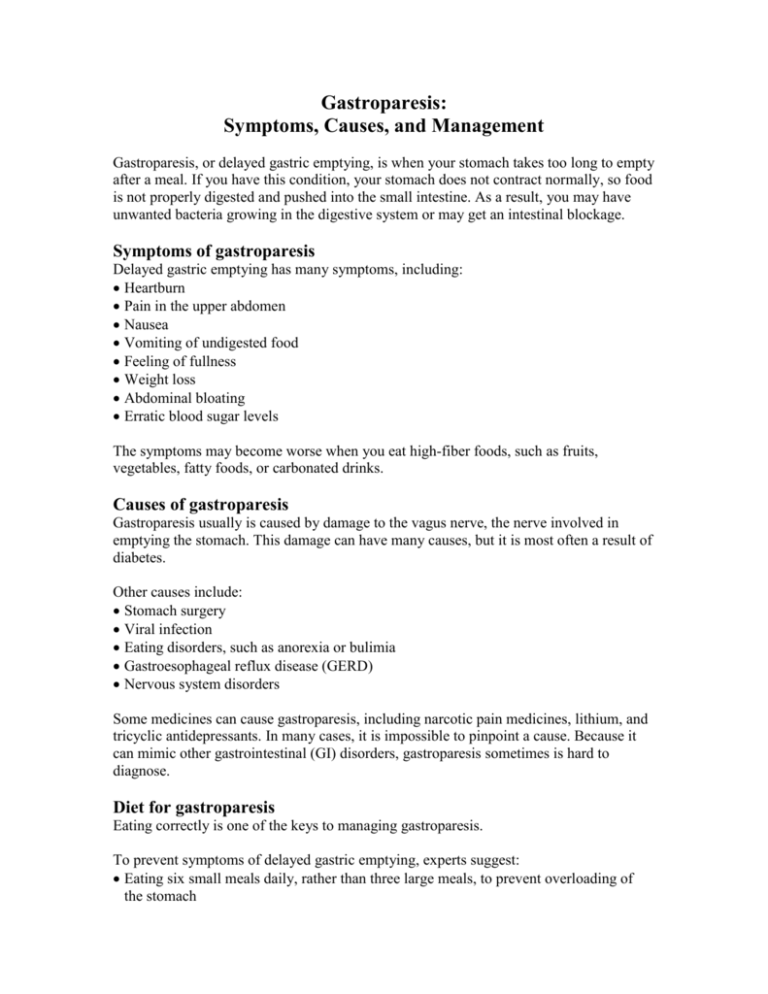
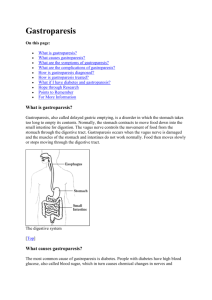
Gastroparesis: Symptoms, Causes, and Management Gastroparesis, or delayed gastric emptying, is when your stomach takes too long to empty after a meal. If you have this condition, your stomach does not contract normally, so food is not properly digested and pushed into the small intestine. As a result, you may have unwanted bacteria growing in the digestive system or may get an intestinal blockage. Symptoms of gastroparesis Delayed gastric emptying has many symptoms, including: Heartburn Pain in the upper abdomen Nausea Vomiting of undigested food Feeling of fullness Weight loss Abdominal bloating Erratic blood sugar levels The symptoms may become worse when you eat high-fiber foods, such as fruits, vegetables, fatty foods, or carbonated drinks. Causes of gastroparesis Gastroparesis usually is caused by damage to the vagus nerve, the nerve involved in emptying the stomach. This damage can have many causes, but it is most often a result of diabetes. Other causes include: Stomach surgery Viral infection Eating disorders, such as anorexia or bulimia Gastroesophageal reflux disease (GERD) Nervous system disorders Some medicines can cause gastroparesis, including narcotic pain medicines, lithium, and tricyclic antidepressants. In many cases, it is impossible to pinpoint a cause. Because it can mimic other gastrointestinal (GI) disorders, gastroparesis sometimes is hard to diagnose. Diet for gastroparesis Eating correctly is one of the keys to managing gastroparesis. To prevent symptoms of delayed gastric emptying, experts suggest: Eating six small meals daily, rather than three large meals, to prevent overloading of the stomach Avoiding high-fiber foods, such as many fruits and vegetables, dried beans and peas, and whole-grain breads, because diets high in fiber are associated with bezoars, which are a mixture of food fibers that get caught in the stomach and can cause a blockage Eliminating high-fat foods from your diet Avoiding adding fat, such as butter, margarine, mayonnaise, and oils, to other foods Chewing foods well—you may need to grind or puree foods, such as meats, before eating them to make them easier to digest Choosing pudding, such as Ensure® Pudding, and liquids, such as Ensure® or Glucerna®, to help prevent weight loss—these often are easier for your stomach to digest Medications to treat gastroparesis Your doctor can prescribe medicines that can help improve gastric emptying, including Reglan® or erythromycin. Other medicines are available to help you manage nausea or diarrhea. Gastroparesis and diabetes If you have diabetes, gastroparesis can affect your blood sugar levels. In fact, gastroparesis can make diabetes worse. Your blood sugar may rise and fall because of delayed digestion. Make sure you monitor your blood sugar regularly. It may help to talk with a registered dietitian or registered dietitian nutritionist who is skilled in diabetes to help you plan meals. This will help you manage your gastroparesis and keep your blood sugar as normal as possible. References and recommended readings Fox J, Foxx-Orenstein A. Gastroparesis. American College of Gastroenterology Web site. http://www.acg.gi.org/patients/gihealth/gastroparesis.asp. Published August 2004. Updated December 2012. Accessed February 10, 2014. National Digestive Diseases Information Clearinghouse (NDDIC). Gastroparesis. National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), National Institutes of Health Web site. http://digestive.niddk.nih.gov/ddiseases/pubs/gastroparesis. Updated June 15, 2012. Accessed February 10, 2014. Parrish CR, Yoshida CM. Nutrition interventions for the patient with gastroparesis: an update. Practical Gastroenterology. August 2005:29-66. http://www.medicine.virginia.edu/clinical/departments/medicine/divisions/digestivehealth/nutrition-support-team/nutrition-articles/ParrishArticle.pdf. Accessed February 10, 2014. Review Date 2/14 G-0812