ONCOLOGY/PALLIATIVE CARE UNIT
advertisement
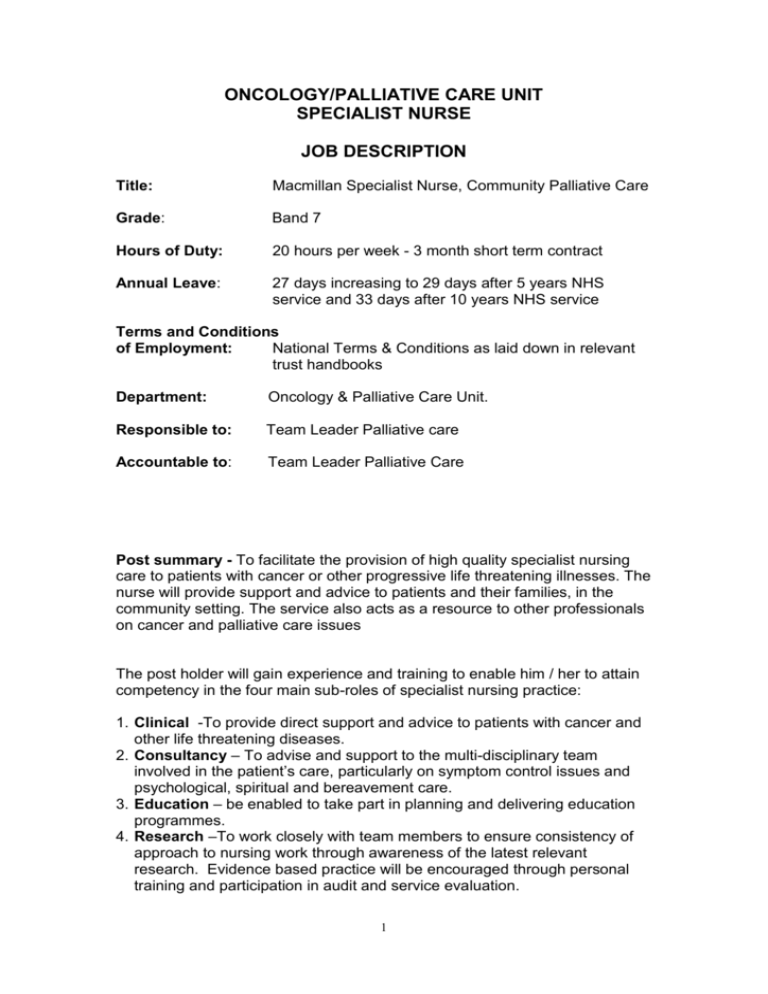
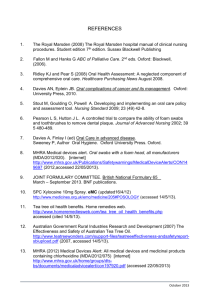
ONCOLOGY/PALLIATIVE CARE UNIT SPECIALIST NURSE JOB DESCRIPTION Title: Macmillan Specialist Nurse, Community Palliative Care Grade: Band 7 Hours of Duty: 20 hours per week - 3 month short term contract Annual Leave: 27 days increasing to 29 days after 5 years NHS service and 33 days after 10 years NHS service Terms and Conditions of Employment: National Terms & Conditions as laid down in relevant trust handbooks Department: Oncology & Palliative Care Unit. Responsible to: Team Leader Palliative care Accountable to: Team Leader Palliative Care Post summary - To facilitate the provision of high quality specialist nursing care to patients with cancer or other progressive life threatening illnesses. The nurse will provide support and advice to patients and their families, in the community setting. The service also acts as a resource to other professionals on cancer and palliative care issues The post holder will gain experience and training to enable him / her to attain competency in the four main sub-roles of specialist nursing practice: 1. Clinical -To provide direct support and advice to patients with cancer and other life threatening diseases. 2. Consultancy – To advise and support to the multi-disciplinary team involved in the patient’s care, particularly on symptom control issues and psychological, spiritual and bereavement care. 3. Education – be enabled to take part in planning and delivering education programmes. 4. Research –To work closely with team members to ensure consistency of approach to nursing work through awareness of the latest relevant research. Evidence based practice will be encouraged through personal training and participation in audit and service evaluation. 1 Key Areas of Responsibility Clinical The post Holder will: 1. In collaboration with other members of the multi-disciplinary team, assess the needs of patients, families and other carers and provide specific advice or support as appropriate. 2. Advise and support the multi-disciplinary team to provide high quality care. This might include advice on pain and symptom control, care planning, spiritual, social and psychological care, communication and resources. 3. Collaborate with other health care professionals and relevant agencies to promote planned co-ordinated care. 4. Maintain adequate records of all patients and ensure all relevant information is documented in the patient’s medical/nursing notes. 5. Evaluate the effectiveness of nursing interventions and treatment protocols. 6. Facilitate the provision of bereavement support to families and other carers. 7. To participate in the provision of information to patients and their carers regarding their illness treatment and services available 8. The post holder will ensure that all clinical practice is directed by the NMC. advisory documentation, e.g. Code of Professional Conduct, Scope of professional Practice, P.R.E.P. etc. Consultancy Under Supervision of the Team Leader the post holder will: 1. Accept requests for specialist palliative care consultation from whoever refers a patient. This could include patients, carers, GP’s, district nurses, colleagues within the Oncology & Palliative Care Unit and others. 2. Consider requests for consultation and direct to appropriate agencies if outside the scope of specialist palliative care. 3. Maintain clarity with regard to the consultation relationship, responsibilities of the consultee and consultant, and lines of accountability. The CNS will only assume primary responsibility for specialist palliative care. 4. If the consultation process is deemed the appropriate response to the request for consultation the CNS will complete a thorough assessment of the situation drawing on his/her skills, knowledge and experience. 5. Identify overt and covert patient problems through assessment. 6. Communicate the findings of the consultation to the primary carer(s) and the patient. 7. Plan action based on the assessment. This might include: education of the patient and primary carers, recommendations for change(s) in therapeutic regime(s), requests for more data from patient and/or primary carer(s), initiation of specialist palliative care techniques if care needs are beyond the competence of the primary carer(s). 2 8. Evaluate, with the patient and primary carers, the effectiveness of recommended interventions. Management The post holder will: 1. Efficiently utilise the resources required to meet service objectives. 2. Participate in business planning and objective setting for the Unit. 3. Participate in the continuing work of the Unit for service improvement to meet the NICE guidance for supportive and palliative care for adults with cancer. 4. To take part in the preparation for Peer review. 5. Manage time in such a way as to fulfil all four sub-roles. 6. Establish and maintain good communication links with medical staff, nursing colleagues, patients and carers, and others, in both hospital and community settings. 7. Take part in appraisal of self and others, including 360-degree appraisals. 8. Take part in reviewing processes of care to enhance efficiency. 9. Foster a multi-disciplinary approach to care through communication and collaboration, and valuing the contribution of others to care. Education The post holder will: 1. Identify the specific education needs of individual patients and carers and facilitate meeting those needs. 2. Identify the training and education needs of the multi-disciplinary team together with senior staff to promote specific skills related to cancer and palliative care. Work collaboratively with relevant educational staff to provide teaching programmes to meet those needs. 3. Prepare and provide learning materials for use within the clinical areas. 4. Act as a role model and mentor to staff. Provide informal education and support to staff in their provision of cancer and palliative care 5. Participate in clinical supervision 6. Keep self up to date through informal and formal learning 3 Audit and Research The post holder will: 1. In consultation with the Unit Manager and collaboration with other specialist nurses, identify and encourage research-based practice in relation to palliative care within the Trust. 2. In conjunction with the Unit manager and Lead Clinicians participate in multi-disciplinary audit. 3. Participate in nursing and collaborative research in palliative care. 4. Submit statistics and activity data as required. 5. Assist in the development of policies, procedures and clinical protocols related to cancer and palliative care. 6. Develop standards of practice against which quality of care may be measured. 7. Contribute to clinical audit as required. 4 Health and Safety Policy Employees must be aware of the responsibilities placed on them under the Health and Safety at Work Act (1974) to ensure that the agreed safety procedures are carried out to maintain a safe environment for employees and visitors. Security It is the responsibility of all employees to work within the security policies and procedures of the Whittington Hospital NHS Trust to protect patients, staff and visitors and the property of the Trust. This duty applies both to the specific work area of the individual and to the Hospital in general. Data Protection This post has a confidential aspect. If you are required to obtain, process and/or use information held on a computer or word processor you should do it in a fair and lawful way. You should hold data only for the specific registered purpose and not use or disclose it in any way incompatible with such a purpose. To disclose data only to authorised persons or organisations as instructed. Breaches of confidence in relation to data will result in disciplinary action that may involve dismissal. No Smoking We have promoted a No Smoking Policy as part of our responsibility for the provision of health. You will be required to work within the framework of this policy. Equal Opportunities This Trust operates an equal opportunities policy. It is the aim of the Trust to ensure that no job applicant or employee receives less than favourable treatment on the grounds of sex, race, colour, nationality or national origins or is placed at a disadvantage by conditions or requirements that cannot be shown to be justifiable. To this end the Trust has an equal opportunities policy and it is for each employee to contribute to its success. Confidentiality You are required to maintain confidentiality of any information concerning patients which you have access to or may be given in the course of your work, 5 in accordance with current policy on confidentiality of the Whittington Hospital NHS Trust. Method of Payment Payment of salary is made into bank account/building society account by direct bank system. Details of a bank account or building society account will be required on the first day of work. There is no facility for any other form of payment. Personal Conduct All staff are expected to treat other members of staff with courtesy and respect. The trusts’ rules & policies, including the disciplinary procedure apply to all staff without exception. NMC Registration The maintenance of registration with the NMC. is a requirement of this post. Post holders are expected to comply with the NMC. regulations and guidance. This Job Description is not exhaustive. It is a general guide to the role and responsibilities expected of the post holder. As such, it will be subject to periodic review and change to meet the emerging needs of the service. DF September 2004 6 ONCOLOGY/PALLIATIVE CARE UNIT SPECIALIST NURSE - PALLIATIVE CARE PERSON SPECIFICATION Educational Requirements First level Registered Nurse; ENB 285 or equivalent palliative care experience, or; ENB 237 or significant oncology experience, plus; ENB 998 (or equivalent). Evidence of ability to undertake study at degree level and to gain one or More of the above mentioned courses. Essential Essential Essential Desirable Essential Experience Two years post registration experience in a oncology/palliative care nursing setting. Teaching experience. Competent knowledge in symptom management and psychological care. Ability to work independently with a caseload. Experience of utilising nursing research and audit. Experience of supporting colleagues. Community experience. Essential Essential Desirable Desirable Desirable Desirable Desirable Skills and Abilities Able to demonstrate knowledge of management. Able to demonstrate good communication skills, written and oral. Able to act as a positive role model. Able to reflect on own performance. Able to take part in own appraisal. Able to take part in clinical supervision. Desirable Essential Essential Essential Essential Essential Knowledge Good understanding of changes facing nursing and the Health Service. Sound clinical knowledge base. Essential Desirable Personal Qualities Good listening skills. Assertive qualities. Ability to negotiate. Clear vision for nursing. Able to work well within a team. Essential Essential Essential Essential Essential Other Requirements Good health record. Able to work flexibly. Willing to develop & extend own practice. Well written application form. Driving licence. Essential Essential Essential Essential Desirable The essential elements of this person specification are minimal. They have been chosen in order to define a person with the right kind of orientation to practice for this post. The desirable elements are those competencies that will be developed through the training offered. 7