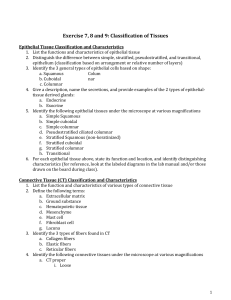
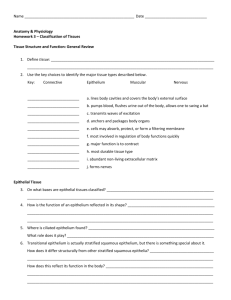
Epithelial Tissue
advertisement

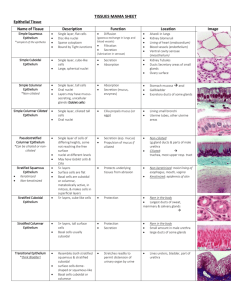
Epithelial Tissue Epithelial tissues cover all body surfaces, line most internal surfaces of passageways or tubes, and are the major tissues of glands. Because epithelium covers organs, forms the inner lining of body cavities, and lines hollow organs, it always has a free surface-one that is exposed to the outside or to an open space internally. The underside of this tissue is always anchored to connective tissue by a thin, noncellular layer called the basement membrane. As a rule, epithelial tissues lack blood vessels; however, substances diffuse from underlying capillaries in connective tissues to nourish epithelial cells. Connective tissue is usually well supplied with blood vessels. Epithelial tissue is classified by the number of cell layers and cell shape. There are three major types of epithelium based on the number of cell layers in each type: 1. 2. 3. Simple epithelium consists of a single layer of cells, with each cell extending from the basement membrane to the free surface. Stratified epithelium consists of more than one layer of cells, only one of which is adjacent to the basement membrane. Pseudostratified epithelium consists of epithelial cells that are all attached to the basement membrane, but only some of the cells reach the free surface. This epithelium is called pseudostratified because, although it consists of a single cell layer, it appears multilayered. The arrangement of the nuclei gives a stratified appearance. There are three types of epithelium based on the epithelial cell shapes: 1. 2. 3. Squamous (flat) cells are flat or scalelike, and frequently look like floor tiles. Cuboidal (cubelike) cells are cube-shaped, and are about as wide as they are tall. Columnar (tall and thin, similar to a column) cells are taller than they are wide. In most cases, an epithelium is given two names, such as simple squamous, stratified squamous, simple columnar, or pseudostratified columnar. The first name indicates the number of layers, and the second indicates the shape of the cell at the free surface. Simple squamous epithelium is composed of a single layer of flattened cells each with a somewhat flattened nucleus Locations: alveoli of the lungs; walls of blood capillaries; mesothelium Function: diffusion; some secretion Key Features: single layer of flat cells with flat nucleus; little matrix, free surface Simple cuboidal epithelium consists of a single layer of cells squarish in profile. The nucleus of each cell is round and centrally located. Locations: bronchioles; kidney tubules; thyroid and other glands Simple columnar epithelium is composed of a single layer of tall, thin cells. The nuclei are usually elongated and located in the basal one-third of the cell. Simple columnar epithelium frequently contain mucus-secreting goblet cells. Locations: the stomach, intestines, and the uterus Functions: secretion and absorption Key Features: single layer of columnar cells; nuclei in a somewhat linear arrangement; may have goblet cells; little matrix Pseudostratified columnar epithelium appears stratified because the nuclei are staggered and appear at many levels. However, it is categorized as simple because every cell contacts the basement membrane. Pseudostratified columnar epithelium frequently contains goblet cells and cilia. Location: the lining of the respiratory passages Function: secretion Key Features: staggered nuclei; may have goblet cells and cilia; little matrix Stratified squamous epithelium consists of multiple layers of cells with the surface cells flattened (squamous) and the deeper cells cuboidal. Some stratified squamous epithelium are keratinized, meaning that the surface cells have died and are anucleated after secreting the protein keratin. Locations: the epidermis, the oral cavity, and the anal canal Function: protection against abrasion Key Features: flattened, anucleated cells near free surface; little matrix Stratified cuboidal epithelium consists of two or more layers of cuboidal cells. Locations: limited, but can be found lining ovarian follicles and the lining of some ducts and glands Functions: lining of ducts Key Features: cuboidal cells near free surface; usually two layers of cells Stratified columnar epithelium consists of two or more layers of cells, typically with columnar surface cells resting upon cuboidal basal cells. Location: limited, and includes small portions of the pharynx and larynx Functions: a transitional zone between stratified squamous epithelium and simple columnar epithelium or pseudostratified epithelium Transitional epithelium consists of two or more layers of cells with the basal cells being mostly cuboidal and surface cells varying from flattened to dome-shaped depending on the distension of the organ. Occasionally binucleated cells are observed near the surface. Locations: limited to structures of the urinary system - ureters, urinary bladder and the urethra Functions: allows for distension as an organ fills with fluid Key Features: domed cells near free surface, binucleated cells Connective Tissue Connective tissues bind structures together, provide support and protection, serve as frameworks, fill spaces, store fat, produce blood cells, protect against infections, and help repair tissue damage. Connective tissue cells are usually spaced farther apart than epithelial cells, and they have an abundance of intercellular material, or matrix, between them. This matrix consists of fibers and a ground substance whose consistency varies from fluid (blood) to semisolid (cartilage) to solid (bone). Connective tissue cells are usually able to divide and replace themselves. In most cases, they have good blood supplies and are well nourished. Some connective tissues, such as bone and cartilage, are quite rigid. Loose fibrous connective tissue, adipose tissue, and dense fibrous connective tissue are more flexible. Fibroconnective tissue, or fibrous connect tissue, is a tissue type that consists of cells and a matrix that is predominately protein fibers. Cell types include: Fibroblasts: most common cell; cell that produces the matrix. Histiocytes: macrophage of fibroconnective tissue. Leukocytes: white blood cells. Plasma cells: cells that produce antibodies. Mast cells: cells that produce the anticoagulant heparin and histamine, a substance that promotes inflammation. Adipocytes: fat cells; cells that store triglycerides. Fiber types include: Collagenous fibers: strong and flexible fibers that appear as wavy bundles in tissue sections. Reticular fibers: thin collagen fibers coated with a glycoprotein. They tend to branch extensively forming delicate networks. Elastic fibers: consist of the protein elastin, which allows for stretching and recoiling. Ground substance: the tissue fluid, minerals, and proteoglycans located between the cells and fibers of connective tissue. Areolar connective tissue consists of a loose arrangement of fibers. It contains all of the cell types mentioned, as well as all three fiber types. Areolar also has an abundance of ground substance, which appears white in tissue preparations. Locations: multiple locations including beneath epithelium and mesenteries Functions: provides nutrients and support to other tissue types; immune functions Key Features: loose appearance, multiple fiber and cell types Adipose tissue consists of adipocytes, which store fat droplets. The nucleus of the adipocyte is located adjacent to the plasma membrane. Locations: subcutaneous region, bone marrow, and mesenteries Functions: lipid storage; thermoregulation; protection Key Features: cells with nuclei "pushed to the side"; minimal matrix; capillaries may be present Reticular connective tissue consists of branching fibers and fibroblasts. Locations: stroma of spleen, liver, lymph nodes and thymus Function: support Key Features: "network" appearance; fibroblasts and branching reticular fibers Dense (fibrous) regular connective tissue consists of closely packed parallel collagen fibers and fibroblasts interspersed between the fibers. Locations: tendons; ligaments Function: strong support Key Features: one fiber type in parallel arrangement; thin fibroblasts; minimal ground substance Dense (fibrous) irregular connective tissue is similar to the dense regular connective tissue except that the collagen fibers do not exhibit a consistent pattern. Locations: dermis; sheaths around bones, nerves and cartilages Function: strong support Key Features: thick bundles of fibers with no pattern, minimal ground substance There are three types of cartilage: (a) hyaline cartilage, (b) fibrocartilage, and (c) elastic cartilage. Cartilage is a connective tissue that consists of chondrocytes trapped in cavities called lacunae and surrounded by extracellular matrix consisting of collagen fibers. The different types of cartilages are classified based on differences in the fibers. Cartilage is avascular; it is frequently surrounded by a layer of dense connective tissue called a perichondrium. Hyaline cartilage contains chondrocytes in lacunae and a matrix of fine collagen fibers that are not visible. Frequently, two or more chondrocytes are nested in one lacunae. Locations: fetal skeleton; covering of bones at joints; ends of ribs Function: flexible support Key Features: glassy appearance; nested chondrocytes in lacunae Elastic cartilage contains chondrocytes in lacunae and a matrix of collagen fibers with elastic fibers randomly oriented. Locations: outer ear; epiglottis; and eustachian tube Function: flexible support Key Features: single chondrocytes Fibrocartilage consists of parallel fibers of collagen fibers with chondrocytes in lacunae interspersed. Locations: intervertebral discs; pubic symphysis Function: firm support Key Features: parallel Compact bone tissue is dense calcified tissue with no spaces visible to the naked eye. The structural unit of compact bone is an osteon. An osteon consists of osteocytes within lacunae embedded within a matrix arranged in concentric cylinders. At the center of each osteon is a central or Haversian canal. Locations: outer surface and shaft of bone Function: support Key Features: