policy_sage10157
advertisement

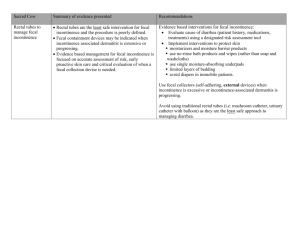
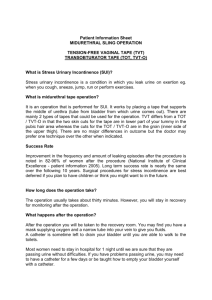
Skyline Medical Center POLICY AND PROCEDURE TITLE: Incontinence Management Guidelines DEPARTMENT/SCOPE: Interdisciplinary PAGE: 1 of 9 ORIGINATION DATE: 10/28/05 REFERENCE NUMBER: REVISED DATE: REVIEWED DATE: Approved By: _______________________ Administrative Officer ___________________________ Medical Director (if applicable) PURPOSE: Incontinence management is a complex problem that requires a comprehensive approach for effective management. An estimated 33% of all hospitalized adults suffer from fecal incontinence.1 Incontinent patients are at 22% higher risk for pressure ulcer development and when immobile the risk increases to 30%.2 Components of successful incontinence management include: (a) consistent protection of intact skin,3,5 (b) treatment of compromised skin with active ingredients4,17, (c) containment of intractable fecal incontinence,6,10 and (d) non-traumatic cleansing of skin.7,8,9 Comprehensive management of incontinence reduces the incidence of perineal dermatitis (PD) and reduces the risk for incontinence related pressure ulcers.18 POLICY: Assessment of the integument is an essential component of the nursing patient assessment. A skin assessment will be performed for each patient on admission, q shift and with a significant change in condition that could lead to skin breakdown. Patients experiencing incontinent episodes will be assessed for management per SLMC Incontinence Management Guidelines.19 Key care interventions include: (a) assessment of the integument; (b) cleansing of affected, at risk tissue with gentle cloths and non-traumatic techniques;15 (c) consistent application of barrier products; and (e) use of external or internal waste containment products. Patients with incontinence are managed through interventions outlined in SLMC Incontinence Management Guidelines (IMG). IMG goals include prevention of perineal dermatitis (PD), prevention of incontinence related skin breakdown and early treatment of incontinence compromised skin.19 IMG may be initiated by physicians, WOCN, RN or LPN with the exception of the Flexi-Seal® Fecal Containment Device. The Flexi-Seal® Fecal Containment Device (FMS) requires a physician’s or WOCN protocol order for use. Perineal Dermatitis (PD): Clinical indicators for perineal dermatis (PD) include: 1. Location: Peri-anal, perineal, gluteals, upper thighs, labia, scrotal areas where excrement, moisture and urine collect. 2. Maceration (excessive moisture): Tissue presents clinically as over-hydrated tissue with superficial peeling of epidermis. 3. Erythema: Present at areas of excrement contact. Affected tissue is usually painful and indurated (swollen). a. Note: Assess patient for presence of canidiasis (yeast) rash, which presents clinically as a solid red area with characteristic “satellite” lesions. Patients may complain of “itching.” Canidiasis is a common occurrence for incontinent patients and barrier products without antifungal ingredients are not effective for canidiasis treatment. Skyline Medical Center POLICY AND PROCEDURE TITLE: Incontinence Management Guidelines REFERENCE NUMBER: PAGE: 2 of 9 4. Denuded tissue: Loss of epidermal tissue; painful, reddened tissue with weeping serous drainage. Note: Superficial or deep tissue loss may occur with persistent exposure to urine and or feces. PROCEDURE: Skin Cleansing/Protection of Intact Skin 1. Cleansing: Remove stool and or urine from skin contact as soon as possible to prevent maceration and contact damage to skin.13 2. Clean heavy soiling from skin using standard moist washcloths and perineal cleanser. 3. Protection: Perineal Care Washcloths with 3% dimethicone (Comfort Shield® Perineal Care Washcloths) should be used for final cleansing/rinsing of the skin or for general cleansing in the presence of light soiling. a. Rationale: Perineal Care Washcloths with 3% dimethicone provide nontraumatic cleaning of the skin and application of a protective barrier product in one-step, establishing consistency in preventative care.13,14,16 4. Repeat steps 1-3 with each episode of incontinence. Protection and Treatment of Non-Intact Skin 1. Cleansing: Remove stool and or urine from skin contact as soon as possible to prevent maceration and contact damage to skin.13 2. Clean heavy soiling from skin using standard moist washcloths and perineal cleanser. 3. Protection: Perineal Care Washcloths with 3% dimethicone should be used for final cleansing of skin after heavy soiling or for general cleansing in the presence of light soiling. a. Rationale: Perineal Care Washcloths with 3% dimethicone provide nontraumatic cleaning of the skin and application of a protective barrier product in one-step, establishing consistency in preventative care.13,14,16 4. Treatment: Apply Xenaderm® ointment (Castor Oil, Balsam Peru and Trypsin) to affected tissue 2 times daily and PRN with each incontinent episode. Ointment should be applied in a thin layer to cover macerated, denuded tissue and areas of perineal dermatitis (PD). Xenaderm® ointment leaves an added layer of visible protection, promotes healing and soothes irritated, inflamed skin. Skyline Medical Center POLICY AND PROCEDURE TITLE: Incontinence Management Guidelines REFERENCE NUMBER: PAGE: 3 of 9 Containment Urine Patients with urinary incontinence are at risk for development of perineal dermatitis and use of the IMG for prevention and treatment of at risk tissue. Containment of urinary incontinence may be achieved through use of incontinent absorption products or use of an indwelling urinary catheter in conjunction with skin protection guidelines. Cleansing, protection and treatment: (See cleansing, protection and treatment pg. 2). Containment/absorption Incontinent pads and briefs: Used for absorption of urine and feces in small to moderate amounts. Change when damp or wet to prevent maceration of tissue.13 *Incontinent Pads: Reusable pads for standard support surface. Air-flow disposable pads for low-air-loss and air-fluidized specialty beds. *Incontinent Briefs/Diapers: For ambulatory or chair-bound patients only. Remove diapers/briefs when in bed to prevent trapping urine and feces on skin. Indwelling urinary catheter: Containment of urine with an indwelling urinary catheter requires a physician order for placement. See Facility Policy for insertion. Management/Care: - Daily catheter care with soap and water. - Stat-Lock® securing devices if catheter is in place for 48 hours or longer. - Drainage bag placed below level of bladder. - Maintain a closed drainage system. - Use smallest size catheter required. *Consider alternatives to indwelling catheters and incontinence briefs: - Scheduled or timed voiding. - Bladder retraining. - Elimination of bladder irritants. Fecal Containment of fecal material may be necessary to protect at risk tissue when fecal incontinence is persistent or when output volumes are 350-500cc or more in a 24 hour period. Protection of intact skin and treatment of compromised skin may be compromised by persistent, high volume output. Containment systems are an effective supplemental treatment option that is available as part of the IMG treatment plan. Patients with liquid or semi-liquid stools who have the following conditions should be evaluated for use of a fecal pouch to prevent perineal dermatitis: Skyline Medical Center POLICY AND PROCEDURE TITLE: Incontinence Management Guidelines REFERENCE NUMBER: PAGE: 4 of 9 Unconscious patients on enteric feedings. Patients with significantly diminished or decreased LOC that prohibits social continence. Spinal cord injury patients who are not on a bowel routine. External Pouching: Fecal pouching systems are appropriate for containment of small to moderate amounts of semi-liquid or liquid stool (less than 500cc in 24 hrs.). Fecal pouching systems require adhesives for application and are only appropriate for application to intact peri-anal tissue. Fecal pouches are changed every 24-72 hours and as needed for leaking. Note: External pouching systems must be applied during the first episodes of fecal incontinence, when the skin is intact. When skin becomes macerated or denuded, external pouching systems are mostly ineffective. Pouch application takes 2 people. Fecal pouches are only appropriate for bed-bound patients. Application of Fecal Pouch with Integrated Skin Barrier12 1. Wash the perianal area with mild soap and water. Trim the perianal hair. Rinse and dry thoroughly. Close the attached drain cap on the collector. 2. Do not use skin gels or other skin sealants as these products can decrease wear time (i.e. Hollister skin barrier wipe, 3-M™ Carilon™ No Sting barrier film, etc.). 3. If necessary, enlarge the skin barrier to fit the perineal area. Do not cut beyond the printed line on the release paper. 4. Remove the release paper and fold the barrier in half. a. Note: A bead of barrier paste to encircle the barrier opening may assist in obtaining a seal. Hollister Medical Adhesive Spray may also be applied to the barrier to increase adhesive properties of the barrier. Apply only to the barrier (not to the skin) and allow 30-45 seconds to dry before application. 5. Position the patient in the side lying position, top leg flexed at hip knee brought toward chest if possible. Separate the patient’s buttocks and position the skin barrier opening over the patient’s anal opening. Apply barrier to perianal bridge first, then press down the entire barrier firmly. 6. Hold the barrier in place for 30 seconds to 1 minute to achieve good adhesion. The skin must be absolutely dry for the pouch to adhere. 7. The pouch may be connected to a bedside bag for continuous drainage collection if indicated. Skyline Medical Center POLICY AND PROCEDURE TITLE: Incontinence Management Guidelines REFERENCE NUMBER: PAGE: 5 of 9 Fecal Containment System (FMS)11 Patient who experience liquid stool in volumes of 500cc or greater for at least 24 hours may require an internal containment system for management. A physician’s order or WOCN Protocol order is required for use. Criteria for use of the FMS incontinence device include: Liquid/semi-liquid stool volumes of 500cc or greater, for at least 24 hours. Patients must be confined to bed; unconscious, semi-conscious or cognitively impaired with little or no bowel control. Consulted WOCN for evaluation of FMS placement and incontinence management Patient will have been checked for o C. Difficile o Medications with side-effects contributing or causing diarrhea (i.e., antibiotics, Reglan, etc.) As appropriate o Dietary consult to evaluate nutritional interventions for liquid stools Formula at room temperature when administered Formula rate adjusted to tolerance Evaluated for changing to fiber formula Evaluated for changing to peptide based or elemental formulas o Consideration of anti-diarrhea medications o Failed management per IMG for protection and or treatment during the previous for the 24 hours. Contraindications11 Beyond 29 consecutive days of consecutive use. Pediatric patients Patients who are sensitive to or who have an allergic reaction to any components of the kit (i.e., silicone, etc.) Have had lower bowel surgery or rectal surgery within the past year. Have rectal or anal injury. Have a severe rectal or anal stricture or stenosis (distal rectum cannot accommodate the retention balloon when inflated). Have suspected or confirmed rectal mucosa impairment (i.e., severe proctitis, ischemic proctitis, mucosal ulcerations, etc.). Have a confirmed or suspected rectal tumor. Have severe hemorrhoids. Have a fecal impaction. Assessment11 Review patient chart and history for contraindications. Position the patient in the left side-lying position, if able to tolerate, to access the anal opening. With gloves and lubricant, perform a digital examination of the rectum prior to insertion, to rule out presence of impactions obstructions and assess adequate rectal tone for retention of the device balloon.11 Skyline Medical Center POLICY AND PROCEDURE TITLE: Incontinence Management Guidelines REFERENCE NUMBER: PAGE: 6 of 9 Insertion of FMS containment device11 1. Assemble equipment (FMS kit, gloves, lubricant and tap water/saline). Open kit. 2. Fill the syringe with 45cc of tap water or saline. Attach the syringe to the inflation port. Fill the bulb to check for patency then aspirate contents. Leave filled syringe attached to the inflation port. 3. Snap the collection bag to the connector at the end of the catheter. 4. Unfold the length of the catheter to lay flat on the bed, extending the collection bag towards the foot of the bed. Insert a gloved index finger into the retention balloon cuff finger pocket for digital guidance during insertion. Lubricate deflated balloon. 5. Grasp the catheter and gently insert the balloon end through the anal sphincter until the balloon is beyond the external orifice and well inside the rectal vault. 6. While holding the balloon in position, slowly inflate the balloon with 45cc of water or saline. Remove finger and gently pull on catheter to check position and assure seating of the balloon. 7. For positioning checks, note the proximity of the catheter insertion line to the anal opening. Document position of the catheter for reference. 8. Remove the catheter tip syringe by twisting the tip to loosen before removing from the inflation port. 9. Position the length of the flexible silicone catheter tubing along the patient’s legs being careful to avoiding kinks and obstructions. 10. Hang the drainage bag by the strap at the lower end of the bed. Maintenance of Device11 1. Check position of the retention bulb, kinking of tubing, solid particles and external pressure with turning and repositioning of patient. 2. Change the collection bag as needed. Snap the cap onto each used bag and discard according to institutional protocol of disposal of medical waste. 3. Empty drainable pouches every shift and as needed. 4. If sampling is required, attach a new bag, collect the desired amount and replace sampling bag with a new collection pouch. a. Note: If the retention bulb is expelled, it should be reinserted after deflating the balloon and cleaning the catheter with soap and water. See device insertion. Irrigation of Device11 If the silicone catheter becomes blocked with solid particles or the stool is of a semiliquid consistency, the catheter can be irrigated to insure patency of the device. 1. Using the port labeled “irrigation” instill 45-60cc of tap water to flush the silicone catheter. Repeat the procedure as often as necessary to maintain proper function of the device. 2. If repeated flushing with water does not return the flow of stool through the catheter, the device should be inspected to ascertain that there is no external obstruction (i.e., Skyline Medical Center POLICY AND PROCEDURE TITLE: Incontinence Management Guidelines REFERENCE NUMBER: PAGE: 7 of 9 pressure from a body part or piece of equipment). If no source of obstruction is detected, use of the device should be discontinued. Discontinuation of device11 Removal of the rectal catheter is indicated when: There is an increase in the LOC that supports social continence. Patients c/o discomfort with the device. The patient is no longer confined to bed. The consistency of drainage is too thick to pass through the catheter. 1. To remove the catheter from the rectum, the retention balloon must be deflated. Attach the syringe to the inflation port and slowly withdraw all the water from the retention balloon. Disconnect the syringe and discard. 3. Grasp the catheter as close to the patient as possible and slowly remove the device. 4. Dispose of the device in accordance with facility guidelines for disposal of medical waste. Contributors Deborah P. Gray BSN, RN, CWOCN Wound and Skin Care Coordinator Flexi-Seal® is a registered trademark of ConvaTec; Comfort Shield® is a registered trademark of Sage Products Inc.; Xenaderm® is a registered trademark of Healthpoint, Ltd.; 3M™ Carilon™ are registered trademarks of 3M Corp.; StatLock® is a registered trademark of Medical Components, Inc. References 1. Nix, D. (2004). A Review of Perineal Skin Care Protocols and the Skin Barrier Product Use. Ostomy Wound Management. 50(12). HMP Communications, PA. 2. Vollman, K. M. (2005). The Cycle of Process Improvements: A Workshop on Process Improvement Strategies for Optimizing Skin Care Outcomes in the ICU. 3. Emory University (1997, May). Management of the Patient with Urinary Incontinence. In Continence Module. Sec. 4, pp. 52-83. Emory Unversity W.O.C.N Nursing Program, Atlanta, GA. 4. Gray, M., Jones, D. P. (2003, March). The Effect of Different Formulations of Equivalent Active Ingredients on the Performance of Two Topical Wound Treatment Products. Ostomy and Wound Management. 50 (3), pp. 34 (8). HMP Communications. Skyline Medical Center POLICY AND PROCEDURE TITLE: Incontinence Management Guidelines REFERENCE NUMBER: PAGE: 8 of 9 5. Howe, K., Padmanabhan, A., Stern, M. A., Williams, J. (2005, May/June). Managing Diarrhea and Fecal Incontinence: Results of a Prospective Clinical Study in the ICU. Journal of WOCN, 32(38).Supplement 2, Abstract Program, p. 514. Lippincott, Williams & Wilkins. 6. Bliss, D. A., Zehrer, C., Savik, K., Ding, L., Hedblom, E. (2005, May/June). An Economic Evaluation of Skin Damage Prevention Regimes among Nursing Home Residents with Incontinence: Labor Costs. Journal of WOCN. 32 (38). Supplement 2, Abstract Program, p. S1. Lippincott, Williams & Wilkins. 7. Nix, D. (2000). Wound Care: Factors to Consider When Selecting Cleaning Products. Journal of WOCN. 27, pp. 260-268. Mosby. Retrieved 10/27/05 www.wocn.org/education/articles1.html 8. Cleaver, K., Smith, G., Browser, C, Monroe, K. (2005). Evidence-based prevention: a Study evaluating the efficacy of a uniquely delivered skin protectant on Incontinent patients and the formulation of sacral/buttock pressure ulcers. WOCN 2005 Poster Presentation. Las Vegas, NV. 9. Bates-Jenson, B. & Sussman, C. (2001). Pressure Ulcers: Pathophysiology and Prevention. In Wound Care, 2nd Ed. Ch. 325-360. Lippincott, Williams & Wilkins. Philadelphia, PA. 10. ConvaTec (2004). Clinical Evaluation of Flexi-Seal® Fecal Incontinence Management System. Clinical Trial: CC 198-03-A695. 11. ConvaTec (2004). Flexi-Seal®: Directions for Use. E.R. Squibb & Sons, L.L.C. Princeton, N.J Skyline Medical Center POLICY AND PROCEDURE TITLE: Incontinence Management Guidelines REFERENCE NUMBER: PAGE: 9 of 9 12. Hollister (2004). Hollister Drainable Fecal Collector. Hollister Inc., Libertyville, Ill. 13. Doughty, D. B. (1991). Management of Urinary Incontinence. In Urinary and Fecal Incontinence: Nursing Management. Ch.4, pp. 95-150. Mosby, St. Louis, MI. 14. Hunter, S., Anderson, J., Hanson, D., Thompson, P., Langemo, D., Klug, M. G. (2003, Sept.). Clinical Trial of a Prevention and Treatment Protocol for Skin Breakdown in Two Nursing Homes. Journal of Wound, Ostomy and Continence Nursing. 30 (5), pp. 250 (8). Mosby. 15. Newman, D. K. (1999). Incontinence Products. In The Urinary Incontinence Sourcebook. Ch.17, pp.230 (18). Lowell House, Los Angles, CA. 16. Nix, D. (2005). An Analysis of 66 Perineal Skin Care Protocols from 32 States: Use of Skin Protectants is Lacking in Protocols and Application. WOCN 2005 Poster Presentation. Las. Vegas, NV. 17. Bohacek, L., Farley, K. (2004). Improved Healthcare Outcomes in Partial Thickness Wounds. Case Studies. 18. Doughty, D. (2005, May-June). Comparison of Pressure Ulcer Treatments in Long-term Care Facilities. 32(3), pp. 163 (7). Journal of W.O.C.N. Lippincott, Williams & Wilkins. 19. WOCN (1996). Role of the Wound, Ostomy and Continence Nurses in Continence Management. WOCN Position Statement. www.wocn.org/publications/posstate/role/html Retrieved 10/27/05.