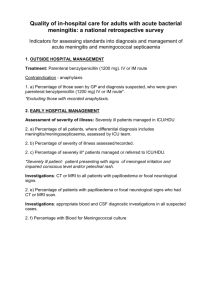
Guideline Bacterial Meningitis and
Bacterial Meningitis and Meningococcal Septicaemia
Summary statement: How does the document support patient care?
The purpose of this policy is to provide evidence based guidance for staff for Bacterial Meningitis and
Meningococcal Septicaemia
Staff/stakeholders involved in development:
Job titles only
Chief of Service
Division:
Department:
Responsible Person:
Author:
For use by:
Purpose:
Women & Child Health
Paediatrics
Chief of Service
Dr M Linney from NICE CG102
Medical staff
To provide guidance to medical staff on how best to approach the management of a child presenting with
Bacterial Meningitis and Meningococcal Septicaemia
NICE CG102 This document supports:
Standards and legislation
Key related documents:
Approved by:
Divisional Governance/Management Group
Approval date:
Ratified by Board of Directors/ Committee of the Board of Directors
Ratification Date:
Expiry Date:
Management of petechial rash 2012 guideline.
W & C Divisional Governance
February 2013
No Applicable – Divisional ratification only required
No Applicable
– Divisional ratification only required.
November 2015
Review date: August 2015
If you require this document in another format such as Braille, large print, audio or another language please contact the Trusts Communications Team
Reference Number: To be added by the Library
Bacterial Meningitis and Meningococcal Septicaemia
Version Page 1 of 7 Jan 2013
Version date
1.0 February 2013
2.0
3.0
Author
Mike Linney
4.0
1.0
2.0
3.0
4.0
5.0
6.0
Index
Introduction
Symptoms and signs
Management in pre hospital setting
Management in secondary care
Organisms and antibiotics
Pictures
Bacterial Meningitis and Meningococcal Septicaemia
Version Page 2 of 7
Status Comment
4
5
7
8
Page No
4
4
Jan 2013
1.0 Introduction
Bacterial meningitis is an infection of the surface of the brain (meninges) by bacteria that have usually travelled there from mucosal surfaces via the bloodstream. In children and young people aged 3 months or older, the most frequent causes of bacterial meningitis include
Neisseria meningitidis (meningococcus), Streptococcus pneumoniae (pneumococcus) and
Haemophilus influenzae type b (Hib). These organisms occur normally in the upper respiratory tract and can cause invasive disease when acquired by a susceptible person. In neonates (children younger than 28 days), the most common causative organisms are
Streptococcus agalactiae (Group B streptococcus), Escherichia coli , S pneumoniae and
Listeria monocytogenes .
Most N meningitidis colonisations are asymptomatic, but occasionally the organism invades the bloodstream to cause disease. Meningococcal disease most commonly presents as bacterial meningitis (15% of cases) or septicaemia (25% of cases), or as a combination of the two syndromes (60% of cases). Meningococcal disease is the leading infectious cause of death in early childhood, making its control a priority for clinical management (as well as public health surveillance and control).
The epidemiology of bacterial meningitis in the UK has changed dramatically in the past two decades following the introduction of vaccines to control Hib , serogroup C meningococcus and some types of pneumococcus. As no vaccine is currently licensed against serogroup B meningococcus, this pathogen is now the most common cause of bacterial meningitis (and septicaemia) in children and young people aged 3 months or older. This guideline does not consider meningitis associated with tuberculosis (TB), because tuberculous meningitis (or meningeal TB) is covered in ‘Tuberculosis: clinical diagnosis and management of tuberculosis, and measures for its prevention and contr ol’ (NICE clinical guideline 33).
However, some features of the presentation of tuberculous meningitis are indistinguishable from bacterial meningitis.
Key priorities for implementation
2.0 Symptoms and signs of bacterial meningitis and meningococcal septicaemia
Consider bacterial meningitis and meningococcal septicaemia in children and young people who present with the symptoms and signs of bacterial meningitis or meningococcal shock. Particularly if they have a fever. Treat as per Table 1
Presentation may be non-specific (see table 2) and mimic viral infections particularly in early stages.
Recognise shock (see table 3) and manage urgently in secondary care.
Under the Health Protection (Notification) Regulations 2010, registered medical practitioners in England have a legal requirement to notify the proper officer of the local authority urgently when they have reasonable grounds for suspecting that a patient has meningitis or meningococcal septicaemia.
Bacterial Meningitis and Meningococcal Septicaemia
Version Page 3 of 7 Jan 2013
Be aware of need for and contraindications to lumbar puncture (table 4)
3.0 Management in the pre-hospital setting
Primary care healthcare professionals should transfer children and young people with suspected bacterial meningitis or suspected meningococcal septicaemia to secondary care as an emergency by telephoning 999.
4.0 Management in secondary care of bacterial meningitis or sepsis.
Table 1 Immediate management of bacterial meningitis
A) Give intravenous ceftriaxone/ cefotaxime immediately to children and young people with a petechial rash if any of the following occur at any point during the assessment : o Signs of bacterial meningitis or
(see table 2) o Signs of shock (table 3), o The child or young person o Petechiae start to spread o Rash becomes purpuric o meningococcal septicaemia appears ill to a healthcare professional
Abnormal CRP or WBC
B ) Give intravenous ceftriaxone/ cefotaxime immediately to children and young people without a petechial rash if suspected of having bacterial meningitis or septicaemia
(Table 2)
Meningococcal Sepsis (early management),
South Thames retrieval service (STRS).
STRS http://www.strs.nhs.uk
Investigations
PCR to meninngoccocal as soon as possible (EDTA bottle). But may be useful upto 96 hours
Perform a lumbar puncture as soon as possible if suspected meningitis unless contraindicated (table 3)
Blood cultures, FBC, Clotting, electrolytes, CRP, Blood glucose, Blood gas as per treating sepsis guideline
All patients with non-traumatic petechial rash must have FBC and film, CRP.
Initial investigations may be normal, treat if suspicious.
Inform senior and refer to PICU management guidelines available on staff intranet. Treat any signs of shock
(table 3) aggressively referring to relevant guidelines
Guidelines for the retrieval and management of severe sepsis and septic shock in infants and children. Southampton and Oxford retrieval team SORT http://www.sort.nhs.uk/home .
Bacterial Meningitis and Meningococcal Septicaemia
Version Page 4 of 7 Jan 2013
Table 2 Signs of Bacterial meningitis or meningococcal meningitis with or without sepsis
Specific symptoms/signs
Non-blanching Rash ( be
aware to check soles feet or palms in darker skin tones)
Altered mental status
Photophobia
Kernigs sign
Brudzinski’s sign
Stiff neck
Unconciousness
Toxic/moribund state
Paresis
Focal neurological deficit
including cranial nerve and abnormal pupils
Seizures
Bulging Fontanelle
Common Nonspecific symptoms/signs
Less common Nonspecific symptoms
Fever
Vomiting/nausea
Lethargy
Irritability/unsettled
Ill appearance
Chills/ shivering
Diarrhoea
Abdominal pain/ distension
Sore throat
Refusing food/drink
Headache
Muscle pain/joint pain
Respiratory symptoms/signs
Blanching macular rash
(early)
Coryza or other ear nose and throat symptoms
Table 3 Signs of shock
Capillary refill time more than 2 seconds
Unusual skin colour
Tachycardia and/or hypotension
Respiratory symptoms or breathing difficulty
Leg pain
Cold hands/feet
Any sign of shock is a clinical emergency inform seniors and refer to sepsis guidelines (See Table 1)
Table 4 Contraindications to immediate lumbar puncture
Signs suggesting raised intracranial pressure o reduced or fluctuating level of consciousness o (Glasgow Coma Scale score less than 9
Shock
Extensive or spreading purpura
After convulsions until stabilised
coagulation abnormalities or a drop of 3 or more) o coagulation results (if obtained) outside o relative bradycardia and hypertension the normal range o focal neurological signs o platelet count below 100 x 10
9
/litre o abnormal posture or posturing o unequal, dilated or poorly responsive o receiving anticoagulant therapy
Local superficial infection at the lumbar pupils o papilloedema
If LP contraindicated consider delayed LP puncture site
Respiratory insufficiency (lumbar puncture is considered high risk of precipitating
Bacterial Meningitis and Meningococcal Septicaemia
Version Page 5 of 7 Jan 2013
5.0 Organisms and Antibiotics
Table 5 Choice of antibiotics and duration
Organism responsible for meningitis
Antibiotic* (*But always be directed by sensitivities any doubt take microbiological
advice)
Duration of Treatment for age group.
AGE
<3 months Infant or child
H.Influenza tybe b ceftriaxone
10 days
S.Pneumoniae
Meningococcus ceftriaxone cefotaxime/
ceftriaxone**
7 days
14 days
7 days
Group B
Streptococcus cefotaxime/
ceftriaxone
minimum 14 days
Listeria
Monocytogenes
IV amoxicillin and gentamicin
21 days amoxicillin and 7 days
gentamicin***
Gram negative
bacilli
Suspected bacterial meningitis (no culture but raised
WBC in CSF)
cefotaxime/ ceftriaxone
IV ceftriaxone/ cefotaxime (+ amoxicillin if less
than 3 months) ceftriaxone
At least 21 days
14 days
10 days
Unconfirmed but likely meningococcus
7 days
disease
Herpes Simplex
meningoencephalitis
IV aviclovir
Take further advice Take further advice
** Ceftriaxone can be used in all age groups but is recognised to increase levels of
jaundice and is therefore contraindicated in those with elevated bilirubins.
***Local agreement to add amoxicillin to cefotaxime if suspicious discuss with microbiology
Bacterial Meningitis and Meningococcal Septicaemia
Version Page 6 of 7 Jan 2013
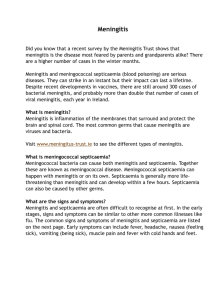
6.0 Pictures
Isolated pin-prick spots may appear where the rash is mainly maculopapular 24 , so it is important to search the whole body for small petechiae, especially in a febrile child with no focal cause
The rash can be more difficult to see on dark skin,but may be visible in paler areas, especially the soles of the feet, palms of the hands, abdomen, or on the conjunctivae or palate.
Bacterial Meningitis and Meningococcal Septicaemia
Version Page 7 of 7
Maculopapular rash in meningococcal septicaemia
Jan 2013