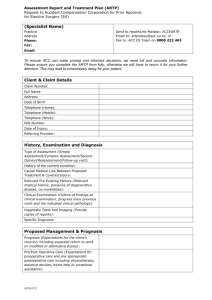
Pain Management Service Agreement
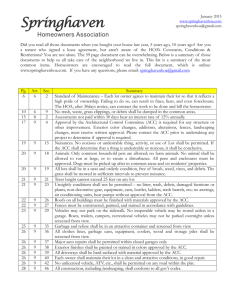
advertisement

Pain Management Services Agreement Operational Guidelines April 2008 This is an evolving document and will be updated as required. We will welcome feedback, particularly from providers. Please use the Feedback Form at the back to suggest improvements. Pain Management Services – Operational Guidelines Contents Introduction ............................................................................................... 1 Pain Services Framework ........................................................................ 1 Services ........................................................................................... 1 Service Principles .............................................................................. 1 Service Philosophy ............................................................................ 2 History and Current Strategy ................................................................... 2 The Pain Management Strategy: Five components ................................. 2 General Guidelines ...................................................................................... 4 Client Entitlements ................................................................................. 4 Vendor Responsibilities and Travel ........................................................... 4 Functional Goal Setting ........................................................................... 5 Working with ACC: Teams and Assistance ................................................. 5 Progressive Goal Attainment Programme (PGAP) – Operational Guideline ........... 8 Introduction .......................................................................................... 8 Eligibility and Services ............................................................................ 9 PGAP Reporting Templates .................................................................... 10 Pain Disability Prevention (PDP) Programme – Operational Guideline ............... 11 Introduction ........................................................................................ 11 Eligibility and Services .......................................................................... 12 PDP Reporting Templates ...................................................................... 13 Functional Reactivation Programme (FRP) – Operational Guideline .................. 14 Introduction ........................................................................................ 14 Other Treatment Limited During the FRP ................................................. 15 Eligibility Criteria .................................................................................. 16 Programme Content ............................................................................. 17 Delivering the Exercise Programme ........................................................ 17 Education Component ........................................................................... 19 FRP Reporting Templates ...................................................................... 19 Pain Management Psychological (PMP) Service – Operational Guideline ............ 23 Introduction ........................................................................................ 23 Eligibility Criteria .................................................................................. 24 Service Delivery and Education .............................................................. 24 PMP Reporting Templates ...................................................................... 25 Pain Management Services – Operational Guidelines Comprehensive Pain Assessment (CPA) Services – Operational Guideline ......... 29 Introduction ........................................................................................ 29 Eligibility Criteria ............................................................................. 29 Programme Content ........................................................................ 29 Pain Management Medical Follow-Up.................................................. 30 Prescribing Pain Medications during the CPA ....................................... 30 Service Delivery and Team ............................................................... 30 The Medial Assessment ......................................................................... 31 The Functional Assessment .................................................................... 32 The Psychological Assessment ............................................................... 32 CPA Reporting Templates ...................................................................... 33 Activity Focus Programme (AFP) – Operational Guideline ................................ 34 Introduction ........................................................................................ 34 Other Treatment Limited During the AFP ................................................. 35 Service Components ............................................................................. 35 Eligibility Criteria .................................................................................. 37 Programme Content ............................................................................. 37 Delivering the Programme ..................................................................... 37 AFP Reporting Templates ...................................................................... 39 Multi-disciplinary Persistent Pain (MDPP) Programme ..................................... 43 Note: This is under development and will be added to the Guidelines when ready. Interventional Pain Management (IPM) Service – Operational Guideline ........... 44 Introduction ........................................................................................ 44 Service Description ............................................................................... 44 Client Referral and Eligibility Criteria ....................................................... 44 Service Delivery ................................................................................... 45 IPM Reporting Templates ...................................................................... 46 Appendix: Frequently Asked Questions (FAQs) .............................................. 47 Pain Management Services: Operational Guidelines - Introduction Introduction Pain Management services are a suite of specialised services, which provide detailed information and recommendation to the case owner on the most appropriate and cost-effective options for treating and managing a client’s pain. The following information is designed to help providers interpret the different Pain Management Services and their contracts. This is a living document and updated versions will be made available as queries arise. These services have been planned and implemented to provide specific treatment for clients who require specialised pain management assessments, treatment and rehabilitation. Note: This information is a guideline only and if there is any conflict between this information and your contract with ACC, the contract takes precedence. Pain Services Framework The framework consists of the specific services, principles, and philosophies. Services Pain management services consist of the following services: 1. Progressive Goal Attainment Programme (PGAP) 2. Pain Disability Prevention (PDP) Programme 3. Functional Reactivation Programme (FRP) 4. Pain Management Psychological Service (PMP) 5. Comprehensive Pain Assessment Services (CPA) 6. Activity Focus Programme (AFP) 7. Multi-disciplinary Persistent Pain Programme (MDPP) (Under Development) 8. Interventional Pain Management Service (IPM) Service Principles The service principles will adhere to the three defining and interconnected principles of the ACC Rehabilitation Framework. These are: 1. Listen to and understand the person in their context. 2. Work with the person to plan and deliver an agreed rehabilitation pathway. 3. Mobilise support and services to help the person to achieve an everyday life. April 2008 Page 1 of 51 Pain Management Services: Operational Guidelines - Introduction Services Philosophy Pain is a unique experience that varies within the same person in terms of frequency, intensity, and impact. Because of its subjective nature the quality of pain can be defined only by the person suffering from it. Pain definition - International Association for the Study of Pain (IASP): “Pain is an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage.” For clients reporting undue pain, assessment using the appropriate tools is the cornerstone of addressing their pain-related factors. Early recognition, acknowledgement, accurate assessment, and timely intervention can reduce the risk of pain-related disability, and significantly enhance the person’s quality of life. A holistic approach addressing physical, emotional, vocational, and social needs and an active client participation in their own rehabilitation plan are essential to effective rehabilitation. In order to optimize rehabilitation outcomes for clients reporting undue pain, it is essential that we provide appropriate multimodal services for the purpose of maintaining and restoring the client’s functionality. It is also vital that treatment and rehabilitation efforts are monitored for effectiveness in returning clients to work or independence. History and Current Strategy The first pain management contracts were set up in January 2000 and most of them have since had a number of variations. All the services now come under the ACC Master Agreement. A service evaluation was completed in August/September 2005 and identified a number of gaps in service delivery. These have been addressed with the implementation of the Pain Management Strategy. Key goals of the strategy were to improve: Access Quality of service The referral process Service monitoring, and Early identification of ‘at risk’ clients, with early access to appropriate services and early interventions. The Pain Management Strategy: Five components A project was set up to implement the strategy which included the following five components: April 2008 Page 2 of 51 Pain Management Services: Operational Guidelines - Introduction The ACC Pain Working Group This is an internal working group set up to manage the pain services project. The group provides support and assistance to the project leader, bringing the skill and expertise necessary for the success of the project. It ensures that the project is on track, monitors progress, ensures output quality, and addresses the implementation of all the work-streams in the project plan. The Pain Focus Group This group consists of representatives from ACC and clinical leaders in pain management who currently provide contracted pain services to ACC. Nominations for the group were sought in consultation with the relevant professional bodies. The aim of the group is to: Promote and maintain an overview of service expectations, and Discuss strategies for matters of shared interest between the pain management service providers and ACC with the intention of promoting best possible outcomes for all stakeholders. Pain Management Psychological Services The Pain Management Psychological Service was introduced and provides appropriate psychological assessment and interventions for pain management. The service is delivered by suitably qualified psychologists to help clients achieve the expected outcome(s) in the most effective and long-lasting manner. The ACC Pain Champions ACC is committed to ensuring that staff are well informed and well supported in referring clients for whom pain is an issue. The Pain Champions are a resource for colleagues at each Branch, Contact Centre, and Long-Term Claims Unit. They have attended a number of workshops and training sessions specially developed for Pain Champions. Progressive Goal Attainment Programme (PGAP) and Pain Disability Prevention Programme (PDP) Services These two new services are early intervention tools designed for implementation at 6 weeks post-injury. These services are marketed as “the first disability prevention programme specifically to target psychosocial risk factors for pain and disability.” PGAP and PDP are 10-week activity mobilization programmes that are tailored to meet the rehabilitation needs of clients who struggle to overcome the challenges of a wide range of persistent pain conditions. April 2008 Page 3 of 51 Pain Management Services: Operational Guidelines – General Guidelines General Guidelines Client Entitlements No Co-payment The client may not be charged a co-payment for pain management services. All treatment-related expenses are covered by the payment made by ACC. Client’s Choice of Provider If there is more than one provider in an area it should be clearly documented in the client’s notes that they were offered the choice of service provider. The client’s rehabilitation plan would be a suitable place to note that this choice has been given. For a list of providers see, www.acc.co.nz > For providers > How to work with ACC > Search for contracted providers. Clients are entitled to access pain management services five days a week between the hours of 8am and 5pm, Monday to Friday. Vendor Responsibilities and Travel Reason to Decline or Delay Referral Vendors have an obligation to decline or delay any referrals they deem to be inappropriate, based on the information provided to them and/or following their assessment of the client. Rationale for the decline or delay will be given to the case owner and subsequently reviewed by ACC. A decision to decline a referral should be advised to the case owner at the earliest possible time. Clinical Records Clinical records are to be maintained to mirror the standards set out in the ACC Treatment Provider Handbook 2007. Each session is to have a clinical record. ACC may request clinical notes to audit and monitor the service. Provider Travel ACC may pay for service providers to travel to and from the provider’s base. The individual service agreement will specify if travel is covered, and the travel distance that can be invoiced for. Vendors may invoice for both travel time and travel distance. If more than one client is seen at the facility, travel may only be invoiced once per return trip and will be pro-rated across the number of clients. Equipment No equipment is supplied by ACC for any of the services under this contract. April 2008 Page 4 of 51 Pain Management Services: Operational Guidelines – General Guidelines Functional Goal-setting Background The International Classification of Functioning, disability and health (ICF) model is useful for rehabilitation providers and ACC staff to refer to when considering a client’s functional aspects of health. This model helps to move all stakeholders away from impairment-focused or deficit-focused frameworks to a participative one. Considering activity limitations, ie restrictions in daily living and life roles, is central to rehabilitation efforts. Functional Goals The provider uses appropriate assessment tools to determine the client’s activity limitations, ie restrictions to their usual activities of daily living and life roles. In consultation with the client, the key areas of restriction are identified and goals are set for the purpose of planning eventual return to these activities. Functional goals are meaningful to the client because they relate to their participation priorities and life roles. The provider and client work collaboratively to set sequential and achievable goals. Progress with the goals can easily be measured and progressed until the long-term goal of return to usual activities of daily living is achieved. Working with ACC: Teams and Assistance The Teams Case Owners Case owners deal with queries relating to the specific claim of a specific client. Relationship Managers ACC has a team of 20 Relationship Managers who advise and help providers to work with ACC as effectively as possible. Relationship Managers also work with Programme Managers and the ACC branches to monitor compliance with the service’s monitoring plans, contract specifications, and ACC’s legislation. The team is responsible for: Providing updates on ACC policies, processes, and services to providers Organising continuing medical education (CME) sessions Helping to train providers who are new to New Zealand Managing provider issues and facilitating communication Ensuring providers reflect best-practice in their treatment of clients Monitoring activity using the Health Purchasing Provider Performance Monitoring Framework Helping with development, negotiation, and implementation of provider performance improvement plans. Your local Relationship Manager can be contacted via the Provider Helpline on 0800 222 070. April 2008 Page 5 of 51 Pain Management Services: Operational Guidelines – General Guidelines Health Procurement Facilitators The Health Procurement Facilitator advises on and applies best practice procurement for all contracts, and manages tenders, renewals and variations. During the term of the contract, they facilitate named provider requests, new entrant applications and evaluations, and contract terminations. They also deal with vendor and provider contractual issues. Contracts Administrators The Contract Administrators: Manage the application of vendors to the contract Generate vendor specific contracts Maintain a register of vendors and providers, and Load vendor and provider information on MFP and Informe sites of the ACC intranet. Note: This is also the group to contact with any change of address details. Programme Managers The Programme Manager’s responsibilities for their given service are: Scoping, developing, and implementing the service purchasing strategies Developing policies and processes Arranging relevant training for the services Liaising and working with ACC Branch and other staff Consulting with providers, provider groups, other government agencies Managing the service, and Monitoring and evaluating service delivery. Assistance Provider Helpline For help with any enquiries please phone the Provider Helpline on 0800 222 070. Client Non-compliance or Did-not-attend (DNA) Measures must be taken to address non-compliance issues including attempts to contact the client via telephone calls and letters. The provider must notify the case owner of any instances of non-compliance, such as missed appointments, within one working day. Report Templates Report templates are listed in, and can be linked to from, this document under each service. They can also be found on ACC’s website (www.acc.co.nz) under For Providers > Resources, and scroll down to the Pain Management section. April 2008 Page 6 of 51 Pain Management Services: Operational Guidelines – General Guidelines Payment To invoice ACC, please send us: An ACC40 or ACC47, or Your normal business invoice. If sending a normal business invoice, remember to include the claim number, purchase order number, and service item code(s). Please send the invoice to your regional Processing Centre: ACC, PO Box 90341, Auckland, OR ACC, PO Box 408, Dunedin. April 2008 Page 7 of 51 Operational Guidelines: Pain Management Services – PGAP Progressive Goal Attainment Programme (PGAP) – Operational Guideline Introduction The Progressive Goal Attainment Programme (PGAP) is a disability prevention programme designed to target psychosocial risk factors for pain and disability. PGAP is a 10-week activity mobilisation programme which is tailored to meet the rehabilitation needs of clients who are struggling with the challenges of a wide range of persistent pain conditions. The psychological risk factors targeted by PGAP include catastrophic thinking, fear of movement and re-injury, and perceived disability. PGAP services are not intended to replace or alter current medical approaches to treating persistent pain conditions, but focus specifically on managing the disability associated with the injury to improve the client’s quality of life and help them return to work. Further information and support available ACC will supply contracted providers with DVDs, manuals, information technology support, and advice on any queries about programme delivery. Providers will be advised from time to time on how this support will be made available. No extension of service Under no circumstances will PGAP services extend beyond the structured 10 sessions. Staffing requirements PGAP services may only be provided by a Physiotherapist, Occuational Therapist, Registered Nurse, Osteopath, or Chiropractor. Each service provider must: Be registered with ACC as a Treatment Provider Have completed the ACC–approved PGAP training, and hold a completion certificate from the Centre for Research on Pain and Disability, McGill University, Montreal Have relevant experience and/or skills and interest in providing pain management services. April 2008 Page 8 of 51 Operational Guidelines: Pain Management Services – PGAP Eligibility and Services Eligibility Criteria PGAP was purchased specifically as an early intervention tool. Initially only clients who have a vocational rehabilitation entitlement and are in the early stages of rehabilitation (ie less than six months post-injury) are eligible for the programme. This will be reviewed when ACC is able to measure the volumes of referrals and the effectiveness of the treatment. Clients can be referred for PGAP when all of the following criteria are met: Significant psychosocial risk factors have been identified, and There are no medical contraindications, and The client’s GP has been consulted about the referral. Service Assessment and Programme Content The PGAP service is delivered in accordance with the contract and consists of the following components. Assessment The clients are asked to complete a set of self-report instruments at three stages during their treatment. These stages are at initial contact, mid-way through treatment (session 4) and at treatment termination (session 9). Clients complete measures of catastrophizing, fear of pain, perceived disability, and pain severity. The purpose of the assessment is to: Carry out risk screening assessment measures and confirm the client’s suitability for the programme Explain the purpose of the service to the client and obtain their agreement to participate Form a basis for introducing clients to the role of psychosocial factors in pain and disability Describe the treatment process Guide decisions about any need for additional treatment, as well as the nature of treatment, and Highlight potential obstacles to progress. Programme Content PGAP is a 10-week activity mobilisation programme which is tailored to meet the rehabilitation needs of the client. Each weekly session targets specific objectives. In the first four weeks of treatment, activity scheduling is the primary focus and takes into account the client’s life situation, physical abilities, and stated goals. April 2008 Page 9 of 51 Operational Guidelines: Pain Management Services – PGAP Note: The client must be advised that it is essential to keep their workbook up to date and bring it to each session. In the event that a client arrives at treatment without the client workbook the session must not proceed. The session is rescheduled for later that week and the case owner is notified immediately. PGAP has a modular approach to managing the client’s high-risk factors. The PGAP provider will choose the most appropriate module for the client’s current needs. These modules consist of: The Pain Catastrophizing Module The Fear of Pain Module The Perceived Disability Module, and The Transition to the Workplace Module. This module can be invoked at any time that the service provider, client, and case owner agree that returning to the workplace should be considered. PGAP service providers make use of the following material: The PGAP information DVD PGAP treatment manual PGAP client workbook PGAP assessment instruments The PDP-PGAP.com website PGAP Reporting Templates PGAP service providers do not provide an Assessment Report. Progress and Termination Reports are provided mid-way through the programme and at its completion. The templates for the Reports used for the PGAP service are located on ACC’s website under For Providers > Publications and forms > ACC Publications > Pain Management. The Reports used are the: ACC4220 Progress Report, and ACC4221 Termination Report. April 2008 Page 10 of 51 Operational Guidelines: Pain Management Services – PDP Pain Disability Prevention (PDP) Programme – Operational Guideline Introduction The Pain Disability Prevention Programme (PDP) is a disability prevention programme designed to target psychosocial risk factors for pain and disability. PDP is a 10-week activity mobilisation programme which is tailored to meet the rehabilitation needs of clients who are struggling with the challenges of a wide range of persistent pain conditions. PDP services are suitable for clients who have mental health conditions, particularly depression, and for whom pain symptoms and psychological factors are significant barriers to rehabilitation progress. The psychological risk factors targeted by PDP include depression, catastrophic thinking, fear of movement and re-injury, and perceived disability. PDP services are not intended to replace or alter current medical approaches to treating persistent pain conditions, but focus specifically on managing the disability associated with the injury. Further information and support available ACC will supply contracted providers with DVDs, manuals, information technology support, and advice on any queries about programme delivery. Providers will be advised from time to time on how this support will be made available. No extension of service Under no circumstances will PDP Services extend beyond the structured ten sessions. Staffing requirements PDP services may only be provided by a Medical Practitioner, Psychiatrist, Clinical Psychologist or Health Psychologist. Each service provider must: Be registered with ACC as a Treatment Provider Have completed the ACC–approved PDP training, and hold a completion certificate from the Centre for Research on Pain and Disability, McGill University, Montreal. Have relevant experience and/or skills and interest in providing pain management services. April 2008 Page 11 of 51 Operational Guidelines: Pain Management Services – PDP Eligibility and Services Eligibility Criteria PDP was purchased specifically as an early intervention tool. Initially only clients who have a vocational rehabilitation entitlement and are in the early stages of rehabilitation (ie less than six months post-injury) are eligible for the programme. This will be reviewed when ACC is able to measure the volumes of referrals and the effectiveness of the treatment. Clients can be referred for PDP when all of the following criteria are met: Significant psychosocial risk factors have been identified and it is likely that the client has mental health concerns, and There are no medical contraindications, and The client’s GP has been consulted about the referral. Service Assessment and Programme Content The PDP service is delivered in accordance with the contract and consists of the following components. Assessment The clients are asked to complete a set of self-report instruments at three stages during their treatment. These stages are at initial contact, mid-way through treatment (session 4) and at treatment termination (session 9). Clients complete measures of depression, catastrophizing, fear of pain, perceived disability, and pain severity. The purpose of the assessment is to: Carry out risk screening assessment measures and confirm the client’s suitability for a programme Explain the purpose of the service to the client and obtain their agreement to participate Form a basis for introducing clients to the role of psychosocial factors in pain and disability Describe the treatment process Guide decisions about any need for additional treatment, as well as the nature of treatment, and Highlight potential obstacles to progress. Programme Content PDP is a 10-week activity mobilisation programme which is tailored to meet the rehabilitation needs of the client. Each weekly session targets specific objectives. In the first four weeks of treatment, activity scheduling is the primary focus and takes into account the client’s life situation, physical abilities, and stated goals. April 2008 Page 12 of 51 Operational Guidelines: Pain Management Services – PDP Note: The client must be advised that it is essential to keep their workbook up to date and bring it to each session. In the event that a client arrives at treatment without the client workbook the session must not proceed. The session is rescheduled for later that week and the case owner is notified immediately. PDP has a modular approach to managing the client’s high-risk factors. The PDP provider will choose the most appropriate module for the client’s current needs. These modules consist of: The Pain Catastrophizing Module The Fear of Pain Module The Perceived Disability Module, and The Transition to the Workplace Module. This module can be invoked at any time that the service provider, client, and case owner agree that returning to the workplace should be considered. PDP service providers make use of the following material: The PDP information DVD PDP treatment manual PDP client workbook PDP assessment instruments The PDP-PGAP.com website PDP Reporting Templates PDP service providers do not provide an Assessment Report. Progress and Termination Reports are provided mid-way through the programme and at its completion. The templates for the Reports used for the PDP service are located on ACC’s website under For Providers > Publications and forms > ACC Publications > Pain Management. The Reports used are the: ACC4222 Progress Report, and ACC4223 Termination Report. April 2008 Page 13 of 51 Operational Guidelines: Pain Management Services – FRP Functional Reactivation Programme (FRP) – Operational Guideline Introduction The following information is designed to help you interpret the Functional Reactivation Programme (FRP) contract. FRP services are for ACC-referred clients who have injury-related pain that has persisted for over six weeks. The rehabilitation programme consists of: An individual exercise programme. See, Delivering the Exercise programme on page 17. Education in pain management and the practical applications of selfmanagement principles including skills training in Cognitive Behavioural Therapy. See, Education Component on page 18. The exercise programme targets key pain-related disability factors using a physical reactivation approach to help clients return to the maximum possible level of functional independence and to participate in their usual activities at work and at home. The programme is aimed at clients who have not returned to work and/or independence due to injury for more than six weeks. Each individualised programme is designed to be relevant to the client’s social, work/home surroundings, and within their economic means. The service is to be provided in a facility where the client can have an individualised prescribed exercise programme. This may be, but is not limited to, the treatment clinic, an exercise facility, gymnasium or swimming pool. Client Access to Programmes In order for clients to return to full-time workforce duties as well as participating in the rehabilitation programme, it is expected that there will be flexibility to access the programme at exercise facilities beyond normal working hours with some supervision. Worksite or Home Visit A worksite or home visit may be undertaken, if appropriate. Please see the referral information, and/or discuss with the case owner, as to whether a worksite assessment has already been done or home visit is required. If a worksite visit is required this will take place at the client’s usual work premises. April 2008 Page 14 of 51 Operational Guidelines: Pain Management Services – FRP No Client Co-payment The programme is fully funded and no co-payment may be charged to the client. Client entrance fees to gymnasiums, swimming pools or exercise facilities are included in the contract price, as is the cost of all exercise equipment such as therabands, swiss balls, and other similar equipment. Clinical Records Clinical records are to be maintained to mirror the standards set out in the ACC Treatment Provider Handbook 2007. Each exercise session is to have a clinical record, which may include an activity log demonstrating the type, frequency, repetition and grade of exercise performed, and any adjustment to the programme. The records must also include the education given to the client. ACC may request clinical notes to audit and monitor the service. Other Treatment Limited During the FRP Concurrent Treatment Concurrent treatment during the FRP is limited to psychological services and vocational rehabilitation in most circumstances. Finish Manual Treatment First or Suspend FRP Manual or “hands-on” treatment (manual therapy, ultrasound, acupuncture, etc) should be completed before starting the FRP because: An FRP aims to facilitate self-management, and it is therefore important that a consistent approach is taken. By continuing with “hands-on” treatment there is the risk of confusing the client as to which is the best approach to take and thereby reducing their compliance with self-management and thus the FRP. Education given in the FRP regarding the pathophysiology of persistent pain may be undermined by continuing to treat the local area. In rare circumstances where a provider believes that hands-on treatment is justified, an ACC32 should be completed, showing why hands-on treatment and an FRP are appropriate concurrently. Once approved, additional manual treatment may then be given and the FRP suspended until the issues needing treatment are resolved. The FRP may then recommence and the exercise activity adjusted accordingly. Payment for the manual treatment is invoiced to ACC separately in the usual manner for that service provider, eg Endorsed Provider Network Physiotherapy Services Agreement, Cost of Treatment Regulations. Exception If the client has a separate injury accepted claim at a different body site which requires manual treatment, this may be treated concurrently with the FRP, as long as the injury does not interfere with the rehabilitation. Discuss individual cases with the case owner before starting manual treatment. April 2008 Page 15 of 51 Operational Guidelines: Pain Management Services – FRP Eligibility Criteria ACC will identify appropriate clients and make the referral to the vendor for an FRP when all of the following criteria are met: Clients have functional difficulties due to pain-related disability factors arising from their personal injury The client has not returned to work and/or full independence (they are receiving ACC funded Home and Community Support Services) due to injury for more than 6 weeks. Clients who display catastrophising and/or fear avoidance behaviours, ie believing that something terrible will happen to them or their injury will get much worse with increased activity. Who is not eligible for this programme? Clients who only require strengthening/fitness activities, which can be provided under physiotherapy regulations. Clients for whom their pain-related disability factors is not a significant barrier to rehabilitation Clients who are currently receiving hands on manual therapy, ie: physiotherapy or further investigation or medical treatment for the covered injury. Clients who are already attending: o Work Hardening Programme (WH) o Progressive Goal Attainment Programme (PGAP) o Pain Disability Prevention Programme (PDP) o Activity Focused Programme (AFP) o Multidisciplinary Pain Programme (MDPP) o Comprehensive Pain Assessment Service (CPA) Clients who do not qualify for Weekly Compensation or ACC-funded Home and Community Support services (these people may receive strengthening and fitness services under Physiotherapy Regulations, the EPN contract or community activities). When recommending that ACC refers a client for a functional reactivation programme, providers need to remember: This programme is for clients with pain related disability factors. The focus of this programme is for clients to achieve the closest possible preinjury level of independence and participation in their usual work and home activities. The exercise programme is aimed at addressing the key activity limitations of the client at home and work as identified by a Work Site Assessment or Home Assessment to help clients regain their ability to perform tasks essential to their job and/or ability to live independently. The programme is within the clients’ economic means so they will continue with exercises following completion of the programme. If the service provider identifies a client who would benefit from an FRP, they should contact the case owner with supporting reasons for a referral to be made. April 2008 Page 16 of 51 Operational Guidelines: Pain Management Services – FRP Sharing clinical information via discussion with the client’s GP and case owner helps to determine whether the FRP is the most appropriate service to meet the client’s needs, and allows for the provision of integrated and co-ordinated rehabilitation. Programme Content The programme consists of: An initial subjective and objective assessment to determine the current level of functioning and to identify any “yellow flags” or “red flags”. Refer to the ACC Pain Compendium for evidence-based assessment tools to include in your assessment. A worksite/home visit, if appropriate, to determine the current level of function, the involvement of the employer, and to design the individualised programme which will help the client return to full participation in work/home activities. Developing the Plan of Action which: o Identifies the programme duration and frequency o Identifies activities to target including the type of exercise to be undertaken in the exercise facility and the continuation of this as a home exercise programme o Details the education and skills training (which follow the principles of Cognitive Behavioural Therapy) to be delivered to the client to improve their knowledge and understanding of pain management, and o Shows evidence of setting functional goals with the client. Programmes are more successful when: Good explanations are provided at the beginning Clients take responsibility for their rehabilitation, and The client’s motivation, interests, and agreed goals drive the programme. Extending the Programme The duration of the FRP is 3-12 weeks. An extension to the programme will be granted in exceptional circumstance and will require clear rationale and specific outcomes to be achieved. A case conference is recommended. Delivering the Exercise Programme The focus of the programme is that clients achieve the closest possible pre-injury level of independence and participation in their usual work and home activities. This requires them to achieve self-management by the end of the programme. The programme is to be a minimum of three weeks and a maximum of 12 weeks duration. The number of sessions needed to achieve the identified goals and outcomes is at the discretion of the service provider. ACC requires a minimum of two supervised one-hour sessions per week. April 2008 Page 17 of 51 Operational Guidelines: Pain Management Services – FRP The programme will be tailored to meet the client’s individual needs. It will combine the strengthening and general cardiovascular and aerobic exercises, with the range of motion, stretching, flexibility and relaxation necessary to improve function. These exercises and activities will be graded, increasing in difficulty as the client’s fitness/endurance improves, with a focus on application to their tasks in the home and/or work environment. The service provider is to teach, supervise, and adjust the programme as required. Once the client has reached a point of self-management, the one-onone direct contact may decrease. Evidence demonstrating self management will be documented in the treatment notes and Progress Report. In most instances the decrease in one-on-one supervision would not occur until the half way point of the programme and will be documented in the six week Progress Report. This enables the Service Provider to ensure the safe gradual progression of exercise. The programme is delivered by physiotherapists and occupational therapists. Other exercise professionals may supervise sessions, however they may not alter the programme in any way. In exceptional cases where it is not practical for the service provider to attend each session (eg due to rural location), it is expected that one-on-one supervision will occur at least once a week until the client is independent. This is to be approved by the case owner before the programme starts. Regular contact is to be maintained with the client, eg telephone follow up conversations. During and on completion of the programme, the client’s improved capacity for performance and enhanced skills and problem-solving abilities will be transferred to their normal family, social and work environments. This ensures the service functions as a bridge to independence and productive activity. The exercise programme must be aimed at the key activity limitations of the client, and be within their economic means so that they will continue with the exercise following the completion of the programme. Home Exercise Programme Each client is to be provided with an individualised home exercise programme that will ensure that they take ownership of their rehabilitation. The home exercises are to be completed in between exercise sessions while undergoing the FRP and to continue after discharge from the FRP. This homework could include walking routines, swiss ball exercises, theraband and mat exercises. The provision of these home-based activities or exercise routines should be documented within the client’s records and should include diagrams alongside the type, frequency, repetition, and grade of exercise. April 2008 Page 18 of 51 Operational Guidelines: Pain Management Services – FRP Education Component Education on the practical application of pain management practices (following the principles of Cognitive Behavioural Therapy) is to be delivered throughout the programme. The education sessions can be given to clients either individually or as part of a group. Clients must also be given educational material that will reinforce what has been discussed in treatment sessions. The education programme will teach: The basic physiology and neurophysiology of pain About pain beliefs, misunderstandings about injury and health status, hurt does not equal harm How to understand pain responses, the persistent pain problem and the role of the psychological factors, including barriers to rehabilitation, eg fear and avoidance behaviour The evidence that shows activity is beneficial for pain conditions, activity pacing skills, and how to manage flare-ups Skills training including goal setting, problem-solving, muscle relaxation, cognitive management strategies for managing low mood and/or anxiety, and About other community resources the client may access and utilise to promote self-management and preparation for independence. If the client is having separate sessions with a Psychologist, the service provider should contact the Psychologist to discuss co-ordinating treatment and applying the principles into the practical education sessions. FRP Reporting Templates The templates for the Reports used for the FRP service are located on ACC’s website under For Providers > Publications and forms > ACC Publications > Pain Management. Reporting requirements are detailed in the guidelines below. Reports used are: ACC4224 Assessment Report *Worksite/Home Visit Report ACC4225 Progress Report ACC4226 Completion Report ACC4227 Non-Completion Report. Note: Worksite/Home Visit Report *The Worksite/Home Visit Report does not have a template. Please report on the information requirements listed under Worksite/Home Visit Report below. Reports are required during the programme. They may be submitted to the case owner electronically, by fax, or by post. Payment will be made for each service item on the receipt of a suitable report. April 2008 Page 19 of 51 Operational Guidelines: Pain Management Services – FRP Assessment Report After the Initial Assessment the service provider is to document an Assessment Report which will include a Plan of Action. The Report provides a crucial start to the programme as it details the client’s goals, functional difficulties, current abilities, and pain-related issues. Assessments are both subjective and objective and include discussions with clients about their goals, problems, and education needs. The Initial Assessment The Initial Assessment will: Confirm the client’s suitability for a programme Explain the purpose of the service to the client Assess the client’s knowledge and understanding of their injury Carry out subjective and objective assessments, including using evidencebased assessment tools, to determine the client’s current level of functioning Recommend further assessment if required, eg by a psychologist and/or a psychiatrist. Further assessment must be pre-approved by ACC Identify “yellow flags” or “red flags” with the appropriate recommendations Determine client functional goals to be achieved Confirm the expected outcome(s) with the client, which are outlined in the referral, and develop a Plan of Action to achieve these goals and outcomes Specify how the outcome(s) will be achieved. If the outcome(s) varies from that specified in the referral, the service provider must discuss this and obtain agreement from the case owner, and Identify any need for specific services to be given to the client concurrently (limited to psychological services and vocational rehabilitation). A key component of the Assessment Report is the Plan of Action, which is to be developed with the client. The Plan of Action The Plan of Action will include: Functional goal-setting aiming to restore full participation in the client’s usual activities at work and at home Defining the duration of the programme, specifying the number of sessions per week and the start and end dates for the programme Details of the activities the client will be participating in and identifying the goals the activities are targeting Details of homework activities the client is expected to complete between sessions, including an activity diary Details of regular recording and monitoring of the client’s progress, including progression of exercise activity April 2008 Page 20 of 51 Operational Guidelines: Pain Management Services – FRP Details of the education and skills training (following the principles of Cognitive Behavioural Therapy) which will be delivered and applied to improve the client’s knowledge and understanding of pain management, and Obtaining the client’s written informed consent to the programme. Worksite/Home Visit Report If a work or home assessment is required, the work report will identify which work/home activities the client is not able to perform, and detail functional exercises to help restore the client’s independence and/or work readiness for those activities. The service provider, in collaboration with the client, will target the goal-setting towards those activities. Progress Reports For programmes that run longer than a six week duration, a Progress Report is to be sent to ACC at the mid-point of the programme. For programmes that are between three to six weeks, the Progress Report is only completed at the end of the programme and fulfils the function of the Completion Report. Each written Progress Report must include but need not be limited to: Information on the progress made towards each of the agreed outcomes and goals, and any obstacles encountered including evidence of reassessment using the evidence-based assessment tools Identifying any further significant psychosocial or vocational issues that may have arisen since assessment Any recommendation that the case owner refer the client for concurrent vocational rehabilitation or psychological services Details of the activities implemented and services provided and completed The rationale for any change of treatment or direction Details of homework activities completed between sessions Details of the self-management plan for the client to continue with postprogramme activities Any activities specified in the Plan of Action that were not implemented or completed, and the reasons for this including an opinion as to whether this was due to any client non-compliance, and Answers to any specific questions asked by the case owner in the referral. Completion Report The Completion Report is to be provided at the end of the programme. Each written Completion Report must include but need not be limited to: The client’s engagement in, and satisfaction with, the treatment/intervention provided April 2008 Page 21 of 51 Operational Guidelines: Pain Management Services – FRP Details of the activities implemented and the services provided and completed Details of homework activities completed between sessions Details of the self-management plan for the client to continue with postprogramme activities The client’s functional abilities and improvements made Any activities specified in the Plan of Action that were not implemented or completed, and the reasons for this including an opinion as to whether this was due to any client non-compliance Reasons as to why any of the agreed outcomes were not met at completion of the programme, and Answers to any specific questions asked by the case owner in the referral. Non-Completion Report If the client cannot or will not participate or co-operate with the programme, the provider is to contact the case owner and together make a decision to withdraw the client from the programme. Following this decision the provider is to do a Non-Completion Report which must include, but is not limited to: Details of all unsuccessful attempts to contact the client, eg messages left, letters written and, where applicable, the client’s responses The initial non-compliance occurred The dates and circumstances of subsequent non-compliance Any areas where the client co-operated The areas where the client refused, or was unable, to co-operate Details of the client’s non-compliant behaviour(s) and verbal responses to the service provider’s approaches/requests/instructions Details of steps taken by the service provider to address the non-compliance of the client, including: o Negotiation efforts undertaken to seek compliance o Contact with the client’s case owner and Health Professionals contacted to discuss and address the non-compliance o Details of any agreed new strategies raised by the case owner or Health Professionals, and o Alternatives offered. Details of client’s response to the alternatives proposed Confirmation that the client was advised that continued non–compliance may result in the programme being discontinued and a Non-Compliance Report forwarded to the case owner Details of the client’s response to the advice of the possible consequences of continuing non-compliant behaviour, and Confirmation of any discussions held involving the case owner, client and/or service provider regarding the decision to terminate the service. If the client is withdrawn from the programme within the first three weeks of it starting, the service provider may invoice ACC using the Service Item Code FRNC for each week that the client attended the programme, up to the three weeks. In this situation the Service Item Code FR03 is not invoiced. April 2008 Page 22 of 51 Operational Guidelines: Pain Management Services – PMP Pain Management Psychological Service (PMP) – Operational Guideline Introduction The following information is designed to help you interpret the Pain Management Psychological Service (PMP) contract. The Pain Management Psychological Service (PMP) is for referred clients who have a persistent pain problem due to their covered personal injury which has resulted in significant behavioural, cognitive, social, or psychological dysfunction. The PMP service includes a psychological assessment and provides evidencebased and best practice psychological therapies/interventions to help the client adapt to their injuries. Initial Assessment The Initial Assessment confirms the client’s suitability for the service. See the ACC Pain compendium for validated psychometric instruments you may include in your assessment. Initial Simple Assessment If a Comprehensive Pain Assessment or another full psychosocial assessment has been included in the referral information, then the first assessment will be an Initial Simple Assessment (PMP1). Initial Extensive Assessment In the absence of a previous psychosocial assessment, then the first assessment will be an Initial Extensive Assessment (PMP2). Plan of Action The Plan of Action: Identifies the programme duration and frequency, type of interventions to be provided, goals, and outcomes to be achieved Outlines the education and skills training (following the principles of Cognitive Behavioural Therapy) that will be delivered to improve the client’s knowledge and understanding of pain management, and Includes functional goal-settingwith the client. Programmes are more successful when: Good explanations are provided at the beginning Client’s take responsibility for their rehabilitation, and The client’s motivation, interests, and agreed goals drive the programme. April 2008 Page 23 of 51 Operational Guidelines: Pain Management Services – PMP Eligibility Criteria ACC will identify appropriate clients and make the referral to the vendor for PMP services when all of the following criteria are met: The client has a persistent pain problem due to their covered personal injury The client’s personal injury has resulted in significant behavioural, cognitive, social, or psychological dysfunction The case owner has consulted with the client’s GP about the suitability of PMP services for the client, and The case owner has informed the service provider about the referral for PMP services. Discussion with the service provider and GP helps in sharing clinical information to determine whether PMP services is the most appropriate way to meet the client’s needs and allows for the provision of integrated and co-ordinated rehabilitation. If a treatment provider identifies a client who would benefit from PMP services, they should contact the case owner with supporting reasons for a referral to be made. Service Delivery and Education The treatment/intervention is individualised to meet each client’s needs in order to achieve their treatment goals and outcomes. Evidence-based and best practice psychological therapies/interventions (including Cognitive Behavioural Therapy (CBT) and/or Acceptance and Commitment Therapy (ACT)) are to be provided to help the client adapt to their injury. The programme is to be a maximum of 10 sessions delivered within 16 weeks. The service provider is to teach, monitor, and adjust the programme as required, continually reassessing the progress made towards achieving the goals. Education is to be extended to the client’s support network (family/whanau). Evidence demonstrating progress and self-management will be documented in the clinical notes and Progress Report. Educational material will be given to the client to reinforce what has been discussed in treatment sessions. Clients may be given material to read and work on in between sessions as preparation for self-management and independence. Information on community resources that the client may access and use postdischarge will also be provided. April 2008 Page 24 of 51 Operational Guidelines: Pain Management Services – PMP PMP Reporting Templates The templates for the Reports used for the PMP service are located on ACC’s website under For Providers > Publications and forms > ACC Publications > Pain Management. Reporting requirements are detailed in the guidelines below. The Reports used are the: ACC4228 Assessment Report (simple or extensive) ACC4229 Progress Report ACC4230 Completion Report *Non-Completion Report. Note: Non-Completion Report *The Non-Completion Report does not have a template. Please report on the information requirements listed under Non-Completion Report below. Reports are required during the programme. They may be submitted to the case owner electronically, by fax, or by post. Payment will be made for each service item on the receipt of a suitable report. Assessment Report After the Initial Assessment the service provider is to document an Assessment Report which will include a Plan of Action. The Simple and Extensive Initial Assessment Both the Simple and the Extensive Initial Assessment will: Introduce the client to the purpose of the service including an explanation of the limits of confidentiality and obtaining informed consent Identify and where possible address any other concerns about this service the client may have Confirm the client’s suitability for a programme Assess the client’s knowledge and understanding of their injury Confirm the recommendations of the Comprehensive Pain Assessment with the client if appropriate, and specify the actions required to achieve these recommendations Recommend further assessment if required, eg by a neuro-psychologist and/or a psychiatrist. Further assessment must be pre-approved by ACC Identify “yellow flags” with the appropriate recommendations Determine client functional goals to be achieved Clinical formulation April 2008 Page 25 of 51 Operational Guidelines: Pain Management Services – PMP Confirm the expected outcome(s) outlined with the client, which are outlines in the referral, and develop a Plan of Action to achieve these goals and outcomes Specify how the outcome(s) will be achieved, including the number of sessions and details of what interventions are recommended in order to meet the goals negotiated with the client. If the outcome(s) varies from that specified in the referral, the service provider must discuss this and obtain agreement from the case owner, and Identify any need for specific services to be given to the client concurrently, Concurrent treatment is limited to vocational rehabilitation and other relevant pain management services. Extensive Initial Assessment – additional information The Extensive Initial Assessment and Report will also include: Carrying out subjective and objective assessments, including using standard psychometric evaluation questionnaires to determine the client’s current level of functioning Obtaining the history of the presenting psychological problem, and ascertaining its causal link to the original physical injury A functional enquiry about the client’s present coping skills and support systems, and Assessing pre-injury psychosocial functioning and coping skills by obtaining relevant personal, educational, social, occupational, and psychological/psychiatric history. A key component of the Assessment Report is the Plan of Action, which is to be developed with the client. The Plan of Action The Plan of Action will include: Functional goal-setting aiming to restore full participation in the client’s usual activities at work and at home Defining the duration of the programme, specifying the number of sessions per week and start and end dates for the programme Details of any activities the client will be participating in and identifying the goals the activities are targeting Details of homework activities the client is expected to complete between sessions Detail of regular recording and monitoring of the client’s progress Details of the education and application of skills-training (following the principles of Cognitive Behavioural Therapy) which will be delivered to improve the client’s knowledge and understanding of pain management, and Obtaining the client’s written informed consent to the programme. April 2008 Page 26 of 51 Operational Guidelines: Pain Management Services – PMP Progress Report A Progress Report is to be completed at the mid point of the programme if the total number of sessions to be provided is more than eight. Each written Progress Report must include but need not be limited to: Information on the progress made towards each of the agreed outcomes and goals, and any obstacles encountered including evidence of reassessment using the evidence-based assessment tools Identifying any further significant psychosocial or vocational issues that may have arisen since assessment Any recommendation that the case owner refer the client for concurrent vocational rehabilitation services Details of the activities implemented and services provided and completed The rationale for any change of treatment or direction Details of homework activities completed between sessions Details of the self-management plan for the client to continue with postprogramme activities Any activities specified in the Plan of Action that were not implemented or completed, and the reasons for this including an opinion as to whether this was due to any client non-compliance, and Answers to any specific questions asked by the case owner in the referral. Completion Report The Completion Report is to be provided at the end of the programme. Each written Completion Report must include but need not be limited to: The client’s engagement in, and satisfaction with, the treatment/intervention provided Details of the activities implemented and the services provided and completed Details of homework activities completed between sessions Details of the self-management plan for the client to continue with postprogramme activities The client’s functional abilities and improvements made Any activities specified in the Plan of Action that were not implemented or completed, and the reasons for this including an opinion as to whether this was due to any client non-compliance Reasons as to why any of the agreed outcomes were not met at completion of the programme The discharge formulation Onward recommendations including the need for follow up sessions, and Answers to any specific questions asked by the case owner in the referral. April 2008 Page 27 of 51 Operational Guidelines: Pain Management Services – PMP Non-Completion Report If the client is unable or unwilling to participate or co-operate with the programme, the service provider is to contact the case owner and together make a decision to withdraw the client from the programme. Following the decision the service provider is to do a Non-Completion Report which must include, but is not limited to: Details of all unsuccessful attempts to contact the client, eg messages left, letters written and, where applicable, the client’s responses The date the initial non-compliance occurred The dates and circumstances of subsequent non-compliance Any areas where the client co-operated The areas where the client refused or was unable to co-operate Details of the client’s non-compliant behaviour(s) and verbal responses to the service provider’s approaches/requests/instructions Details of steps taken by the service provider to address the non-compliance of the client, including: o Negotiation efforts undertaken to seek compliance o Contact with the client’s case owner, and Health Professionals contacted to discuss and address the non-compliance o Details of any agreed new strategies raised by the case owner or Health Professionals, and o Alternatives offered. Details of client responses to the alternatives proposed Confirmation that the client was advised that continued non–compliance may result in the programme being discontinued and a Non-Compliance Report forwarded to the case owner Details of the client’s response to the advice of the possible consequences of continuing non-compliant behaviour, and Confirmation of any discussions held involving case owner, client, and/or service provider regarding the decision to terminate the service. April 2008 Page 28 of 51 Operational Guidelines: Pain Management Services – CPA Comprehensive Pain Assessment (CPA) Services – Operational Guideline Introduction The following information is designed to help you interpret the Comprehensive Pain Assessment (CPA) contract. The CPA is a delivered by a multidisciplinary team (MDT – see Service Team, below) which ensures that clients with persistent pain-related disability receive a comprehensive, fully integrated, and independent clinical assessment. The emphasis is on determining functional goals for the client’s rehabilitation. The CPA consists of three separate clinical assessments followed by a team discussion (see Programme Content, below). The team produces a combined ‘formulation’ with recommendations. The advantage of this approach is that the medical, functional and psychological perspectives are substantially enhanced from a team discussion about these modalities. The functional goals and recommendations produced in the report will guide future therapies. Eligibility Criteria ACC will identify appropriate clients and make a referral to the vendor for CPA services when all of the following criteria apply: The client’s GP and/or specialist has requested a referral (or the referral has been discussed with and agreed to by the GP) The client’s injury diagnosis is not in doubt Pain has persisted for at least 12 weeks from the date of injury ACC information has identified that the client has significant pain issues The client’s injury is stable, there is no surgery scheduled, and The client has no other medical problems that either: o Contribute to the pain, or o Would be incompatible with pain management services. Programme Content The CPA consists of: A comprehensive assessment involving a: o Medical Assessment o Functional Assessment, and o Psychological Assessment. An MDT meeting to determine common clinical formulation, goals, and recommendations Feedback to the client of the CPA findings and recommendations April 2008 Page 29 of 51 Operational Guidelines: Pain Management Services – CPA A combined multidisciplinary summary CPA Report with individual discipline reports attached to it Communication with the case owner following their receipt of the CPA Report An option of communicating with Treatment Providers who are currently working with the client, and Pain management medical follow-up, if required. Pain Management Medical Follow-Up A medical follow up should be completed by the Medical Practitioner if medications are being trialled by the client. The follow-up consists of clinical reassessment focusing on the treatment response and guiding future medication. The Medical Practitioner may do up to three medical follow-ups with ACC approval. The follow-ups are to be completed in a timeframe that is appropriate to the medication that the client is trialling. Prescribing Pain Medications during the CPA The Medical Practitioner may recommend a trial of different pain medications during the CPA. Before prescribing any medications the Medical Practitioner must have taken a full medical history to ensure that there are no contraindications to existing medications and medical conditions that the client may have. Service Delivery and Team The multidisciplinary team (MDT) will combine their services to provide an integrated approach to the client’s rehabilitation. In order to broaden the perspective of the client’s assessment the same service provider may not do more than one of the assessments. The service is to be provided in an MDT setting, eg hospital, pain clinic, etc. The MDT service team The MDT consists of a: Medical Practitioner, who holds Vocational Registration in a Medical Speciality Physiotherapist and/or Occupational Therapist, and Psychologist. April 2008 Page 30 of 51 Operational Guidelines: Pain Management Services – CPA The Medical Assessment The Medical Assessment is done by the Medical Practitioner and covers: The pain history which includes the: o Site of pain o Characteristics of pain o Circumstances of onset o Intensity and frequency of pain o Associated symptoms, if any, and o Effects that the pain has on daily activities and sleep. The treatment history which includes: o Medication details including doses and the response/side effects o A history of non-prescriptive medication, complementary therapies, alcohol and substance abuse o Allergies o Other treatment modalities the client has had, including medical, surgical, psychiatric and psychological treatment, and o The client’s response, including attitudes and beliefs of treatment. A physical examination which includes: o Assessment of the affected and non-affected regions for comparison o Examining for red flag signs, and signs of neuropathic features o Baseline cardiovascular, respiratory, neurological, and musculoskeletal function, and o Basic cognitive function. The client’s beliefs, knowledge, and expectations regarding pain prognosis and management Discussing reports, tests, and other relevant documents with the client Identifying whether further investigations are required Rehabilitation recommendations including: o Client-focused functional goals o The medical view of the required multidisciplinary approach o Medical interventions: discuss clinical indication, relationship to other treatment modalities, side-effects, and likely benefits in relation to functional goals o Recommended pain medications: specify dose/frequency and follow-up o Ensuring medications are understood by the client and family/support person o Detailing medical parameters if there are specific medical restrictions on activities in relation to participating in ADLs, work or school, and social activity, and o Any further treatment, investigation, or opinion required. April 2008 Page 31 of 51 Operational Guidelines: Pain Management Services – CPA A diagnosis summary, and Advising the client about the diagnosis, coping strategies, and the assessment process including likely recommendations, if appropriate. The Functional Assessment The Functional Assessment is done by the Physiotherapist or Occupational Therapist. Evidence-based assessment tools may be useful to include in your assessment. The assessment covers: A functional examination which details the client’s current levels of participation in meaningful activity including potential identified rehabilitation goals in the areas of: o Self care o Productive activity (ie work, childcare, housework, home maintenance, voluntary work, driving, etc), and o Leisure (social and recreational activity). Assessing specific functional limitations in any area of activity including strength, endurance, balance, flexibility, activity avoidance, etc Identifying factors that contribute to reduced function including pacing, activity management, and lifestyle balance, and Providing a basic explanation of the assessment process, pain experience, and coping strategies, if appropriate. The Psychological Assessment The Psychological Assessment is done by a Psychologist and covers: Clinical presentation and behavioural observations The client’s current perception and experience of pain, including attitudes and beliefs about pain The impact of pain on current psychological and psychosocial functioning, ie emotional functioning, mood, sleep, and daily activities including work, leisure, family, friends, and relationships Current methods of coping – include both adaptive and maladaptive Pre-injury psychological and psychosocial functioning, including predisposing risk factors for the development of long-term disability Previous psychological conditions and treatment Identifying any barriers to change and rehabilitation/treatment, eg emotional, financial, social, cognitive, beliefs and attitudes, concurrent antagonistic treatment Psychometric assessments and evaluation Clinical formulation and opinion, including a description of maintaining factors Recommendations, including whether further psychological treatment is required, and Providing basic advice about the pain assessment process, pain experience, and coping strategies, if appropriate. April 2008 Page 32 of 51 Operational Guidelines: Pain Management Services – CPA CPA Reporting Template The template for the ACC4232 Comprehensive Pain Assessment Report used in the CPA service is located on ACC’s website under For Providers > Publications and forms > ACC Publications > Pain Management. Reporting requirements are detailed in the guidelines below. The Assessment Report may be submitted to the case owner electronically, by fax, or by post. Payment will be made for each service item on the receipt of a suitable report. The Assessment Report Following the individual assessments an MDT meeting will be held to discuss the findings for the combined multidisciplinary summary Assessment Report. The Report may be written by either one or more of the MDT members collating the assessment findings, diagnostic formulation, goals, and recommendations by the team. The Assessment Report will include: A brief edited summary of the client’s history and assessment findings with highlighted significant features affecting the pain experience The final shared formulation that includes the results of all three assessments The integrated recommendations following the result of the MDT discussion outlining: o Specific functional goals o Priority of intervention o Intervention readiness, and o Timeframes. Evidence of communication/feedback with the client regarding the goals of rehabilitation, the MDT’s recommendations, and the client’s response. The purpose of this communication/feedback is to ensure the client understands and agrees with their rehabilitation plan. Communication may take place by phone or face-to-face. Communication with the case owner following receipt of the CPA report to ensure that recommendations are understood and clear, and The three individual discipline reports attached. April 2008 Page 33 of 51 Operational Guidelines: Pain Management Services – AFP Activity Focus Programme (AFP) – Operational Guideline Introduction The following information is designed to help you interpret the Activity Focus Programme (AFP) contract. The AFP service is a multidisciplinary programme provided to ACC-referred clients who have a persistent pain-related disability with significant functional problems which are due to an injury and have lasted for more than 12 weeks. The purpose of this programme is to help clients adopt a self-management approach to independent functioning both at work and home, despite pain. The Service Team The service is to be provided by a multidisciplinary team (MDT) which is a combination of the following professions: Registered Psychologist (essential) Medical Practitioner (essential) Physiotherapist (essential) Occupational Therapist (optional), and Registered Nurse (optional). The MDT will combine their services to provide an integrated approach to the client’s rehabilitation. The rehabilitation programme has a strong psychological focus to address key pain-related disability factors and consists of an individualised programme and the application of a range of pain management strategies, including skills training in Cognitive Behavioural Therapy to help the client return to independent functioning at work and home. Clinical Records Clinical records are to be maintained to mirror the standards set out in the ACC Treatment Provider Handbook 2007. Each session is to have a clinical record, which may include an activity log demonstrating the type, frequency, repetition, and grade of exercise performed, and any adjustment to the programme. The records must also include the education given to the client. ACC may request clinical notes to audit and monitor the service. Worksite/Home Visit A worksite or home visit may be undertaken, if appropriate. Please refer to the referral information and/or discuss with the case owner as to whether a worksite assessment has already been done or a home visit is needed. If a worksite visit is needed this will take place at the client’s usual work premises. April 2008 Page 34 of 51 Operational Guidelines: Pain Management Services – AFP Other Treatment Limited During the AFP Concurrent Treatment Concurrent treatment during the AFP is limited to vocational rehabilitation. Finish Manual Treatment First or Suspend AFP Manual or “hands-on” treatment (manual therapy, ultrasound, acupuncture, injections, etc) should be completed before starting the AFP because: An AFP aims to facilitate self-management, and it is therefore important that a consistent approach is taken. By continuing with “hands-on” treatment there is the risk of confusing the client as to which is the best approach to take and thereby reducing their compliance with self-management and thus the AFP. Education given in the AFP regarding the pathophysiology of persistent pain may be undermined by continuing to treat the local area. In rare circumstances where a provider believes that hands-on treatment is justified, an ACC32 should be completed, showing why hands-on treatment and an AFP are appropriate concurrently. Once approved, additional manual treatment may then be given and the AFP suspended until the issues needing treatment are resolved. The AFP may then recommence and the activity adjusted accordingly. Payment for the manual treatment is invoiced to ACC separately in the usual manner for that service provider. Exception If the client has a separate injury accepted claim at a different body site which needs manual treatment, this may be treated concurrently with the AFP, as long as the injury does not interfere with the rehabilitation. Discuss individual cases with the case owner before starting manual treatment. Service Components Service providers must include the following components in the programme: Goal-related activities Behavioural intervention and education, and Client progress toward self-management. These components will address education, activity and skills training that adhere to Cognitive Behavioural Therapy principles, and focus on improving the client’s self-efficacy and self-directed pain management. The components can be delivered either individually or in a group as appropriate to the client’s needs. The minimum group size is four participants and the recommended maximum group size is eight to ten participants. Appropriate members of the MDT will provide the components. The Psychologist must provide the education and psychological component. April 2008 Page 35 of 51 Operational Guidelines: Pain Management Services – AFP The Physiotherapist or Occupational therapist will provide the activity programme. The Medical Practitioner will provide a supervisory role monitoring the response to medications, and providing pain education as required. Clinicians will meet and discuss progress and work together ensuring the Plan of Action is tailored to meet the client’s individualised functional goals. Activities Component The Activity component includes supervising a prescribed routine with the client in the most appropriate environment for the identified functional goals. The activities must include graded and monitored exposure to physical activity that the client can practice at home. Education Component Education on pain management practices (which follow the principles of Cognitive Behavioural Therapy) is to be delivered throughout the programme. The education sessions can be given to clients either individually or as part of a group. Clients must also be given educational material that will reinforce what has been discussed in treatment sessions. The education component will address the pain-related disability factors, as identified in the assessment and may include: Providing information about the basic physiology and neurophysiology of pain. This should also address basic principles of analgesia in relation to physiology Addressing pain beliefs, misunderstandings about injury, and health status Addressing flare-ups and using it as a teaching opportunity to raise client awareness of these and develop a flare-up management plan Addressing behaviours such as client fear of movement, and catastrophizing Providing information about persistent pain-related disability, and contributing factors including psychosocial factors, and how they impact on the client’s functioning Providing information about other community resources that the client may use to complement their pain management rehabilitation. Self-management Component Self-management training will be tailored to the individual’s needs to ensure the client has knowledge and ability which may include: Goal-setting Activity-pacing skills, including successive approximations to desired activity Problem-solving Communication skills, ie being able to communicate queries, concerns, and confirmation of understanding of pain management rehabilitation, eg assertiveness training, etc April 2008 Page 36 of 51 Operational Guidelines: Pain Management Services – AFP Cognitive management strategies for unhelpful thinking Muscle-relaxation skills and combining client self-talk and visualisations to reduce autonomic arousal Cognitive Behavioural Therapy and Acceptance Commitment Therapy skills for managing low mood and/or anxiety, and Flare-ups and relapse management. Eligibility Criteria ACC will identify appropriate clients and make the referral to the vendor for an AFP when all of the following criteria are met: The client has functional difficulties due to their personal injury The client has more than 12 weeks pain-related disability with reduced function and loss of independence The client has had a Comprehensive Pain Assessment (CPA), and The CPA recommends that the client needs an Activity Focus Programme to help their rehabilitation. Discussion with the vendor and GP helps in sharing clinical information to determine whether the AFP is the most appropriate service to meet the client’s needs and allows for the provision of integrated and co-ordinated rehabilitation. If a treatment provider identifies a client who would benefit from an AFP, they should contact the case owner with supporting reasons for a referral to be made. Programme Content The programme consists of: An assessment to confirm the client’s suitability for the service A work site or home visit, if indicated A Plan of Action which identifies the number of sessions, type of interventions to be provided, goals, and outcomes to be achieved Delivery of the programme A Progress Report at the midpoint of the programme A Completion Report Liaison with relevant stakeholders, when required, and Follow-up sessions, if indicated. Delivering the Programme The focus of the programme is to achieve the greatest possible level of independence and participation in the client’s usual activities at work and at home. This requires the early achievement of self-management by the client at the completion of the programme. April 2008 Page 37 of 51 Operational Guidelines: Pain Management Services – AFP The programme is to be a minimum of three weeks and a maximum of 12 weeks duration. The number of sessions is at the discretion of the service provider in order to achieve the identified goals and outcomes. However, as a guideline ACC would expect a minimum of two supervised one-hour sessions per week. The service provider is to teach, supervise, and adjust the programme as required. In exceptional cases where it is not practical for the service provider to attend each session (eg due to rural location), it is expected that one-to-one supervision will occur at least once a week until the client is independent. This is to be approved by the case owner before the programme starts. Regular contact is to be maintained with the client, eg telephone follow-up conversations. By completion of the programme the client’s improved capacity for performance, and their enhanced skills and problem-solving abilities will be transferred to their normal family, social, and work environments. This ensures the service functions as a bridge to independence and productive activity. The programme must be aimed at the key activity limitations of the client, and be within their economic means so that they will continue with it following the completion of the programme. Home Programme Each client is to be provided with an individualised home programme that will ensure they take ownership of their rehabilitation. The home activities are to be completed in between the programme sessions and should continue after discharge from the AFP. The provision of these home-based activities should be documented within the client’s records. Monitoring and Supervising the Client during the Programme Monitoring and supervising the client is the responsibility of the service provider who must clearly document the client’s outcomes for the programme. Throughout the sessions the service provider needs to re-assess the client’s goals and discuss the progress made, regularly adjusting the programme based on that progress. Initially one-to-one contact needs to be delivered regularly so that the client is closely monitored and the programme can be adapted as required. Clients will have one-to-one contact with the appropriate service provider, for a minimum of one hour twice a week. Phone contact may be considered one-to-one contact where access to services is restricted (eg rural locations). However, every attempt must be made by the provider to have one-to-one contact. The one-to-one contact may be gradually reduced over the course of the programme as the client’s self-management techniques improve. April 2008 Page 38 of 51 Operational Guidelines: Pain Management Services – AFP AFP Reporting Templates The templates for the Reports used for the AFP service are located on ACC’s website under For Providers > Publications and forms > ACC Publications > Pain Management. Reporting requirements are detailed in the guidelines below. The Reports used are the: ACC4233 Assessment Report *Worksite/Home Visit Report ACC4234 Progress Report ACC4235 Completion Report ACC4236 Non-Completion Report. Note: Worksite/Home Visit Report *The Worksite/Home Visit Report does not have a template. Please report on the information requirements listed under Worksite/Home Visit Report below. Reports are required during the programme. It is expected that all clinicians managing the client’s rehabilitation will contribute to the findings in the reports. They may be submitted to the case owner electronically, by fax, or by post. Payment will be made for each service item on the receipt of a suitable report. Assessment Report The Initial Assessment may be done by any one, or a combination, of the clinicians in the multidisciplinary team (MDT). After the Initial Assessment the team will meet to discuss the subjective and objective findings and will document an Assessment Report which will include the Plan of Action. The Assessment Report may be written by one or more of the team members, collating the team’s assessment findings and recommendations for the programme. The Initial Assessment The Initial Assessment will: Confirm agreement or disagreement, with supporting reasons, on the Comprehensive Pain Assessment (CPA) Confirm the client’s suitability for a programme Explain the purpose of the service to the client April 2008 Page 39 of 51 Operational Guidelines: Pain Management Services – AFP Assess the client’s knowledge and understanding of their injury Confirm the recommendations of the CPA with the client and specify the actions required to achieve these recommendations Carry out subjective and objective assessments, including the use of evidence-based assessment tools, to determine the client’s current level of functioning Recommend further assessment if required, eg by a neuro-psychologist and/or a psychiatrist. Further assessment must be pre-approved by ACC Identify “yellow flags” and/ or “red flags” with the appropriate management recommendations Determine client functional goals to be achieved Confirm the expected outcome(s) with the client, which are outlined in the referral, and develop a Plan of Action to achieve these goals and outcomes Specify how the outcome(s) will be achieved. If the outcome(s) varies from that specified in the referral, the service provider must discuss and obtain agreement from the case owner, and Identify any need for specific services to be given to the client concurrently (limited to psychological services and vocational rehabilitation). The Plan of Action The Plan of Action is developed in collaboration with the client and will identify functional goals which need to address areas of: Self-care Productive activity (eg work, childcare, housework, driving) Leisure (recreational and creative activity), and Psychological, social, and emotional function. The programme should not exceed 12 weeks and is at the discretion of the service provider in order to achieve the client goals and outcomes the activities are targeting. The Plan of Action will: Identify the detail the activities of the programme, and number of sessions the client will attend per week, and the start and end dates for the programme, and Detail the homework requirements the client is expected to complete between sessions, which may include an activity diary. Worksite/Home Visit Report If a work or home assessment is required, the work report will identify which work/home activities the client is not able to perform, and detail functional exercises to help restore the client’s independence and/or work readiness for those activities. The service provider, in collaboration with the client, will target the goal-setting towards those activities. April 2008 Page 40 of 51 Operational Guidelines: Pain Management Services – AFP Progress Report A Progress Report is to be completed at six weeks for all programmes that run for longer than a six week duration. Each written Progress Report must include but need not be limited to: Information on the progress made towards each of the agreed outcomes and goals, and any obstacles encountered including evidence of reassessment using the evidence-based assessment tools Identifying any further significant psychosocial or vocational issues that may have arisen since assessment Any recommendation that the case owner refer the client for concurrent vocational rehabilitation services Details of the activities implemented The rationale for any change of treatment or direction Details of homework activities completed between sessions Details of the self-management plan Any activities specified in the Plan of Action that were not implemented or completed, and reasons for this including an opinion as to whether this was due to any client non-compliance. Completion Report The Completion Report is to be provided at the end of the programme and must include: The client’s engagement in, and satisfaction with, the treatment/intervention provided Details of the activities implemented and the services provided and completed Details of homework activities completed between sessions Details of the self-management plan for the client to continue with postprogramme activities The client’s functional abilities and improvements made Any activities specified in the Plan of Action that were not implemented or completed, and reasons for this including an opinion as to whether this was due to any client non-compliance Non-Completion Report If the client is unable or unwilling to participate in or co-operate with the programme, the service provider is to contact the case owner and together make a decision to withdraw the client from the programme. Following the decision the service provider is to provide a Non-Completion Report which must include: Details of all unsuccessful attempts to contact the client, eg messages left, letters written and, where applicable, the client’s responses The date the initial non-compliance occurred The dates and circumstances of subsequent non-compliance April 2008 Page 41 of 51 Operational Guidelines: Pain Management Services – AFP Any areas where the client co-operated The areas where the client refused or was unable to co-operate Details of client non-compliant behaviour(s) and verbal responses to the service provider’s approaches/requests/instructions Details of steps taken by the service provider to address the non-compliance of the client, including: o Negotiation efforts undertaken to seek compliance o Contact with the client’s case owner, and the Health Professionals contacted to discuss and address the non-compliance o Details of any agreed new strategies raised by the case owner or Health Professionals, and o Alternatives offered. Details of the client’s responses to the alternatives proposed. Confirmation that the client was advised that continued non–compliance may result in the programme being discontinued and a Non-Compliance Report forwarded to the case owner Details of client response to the advice of the possible consequences of continuing non-compliant behaviour, and Confirmation of any discussions held involving the case owner, client, and/or service provider about the decision to terminate the service. April 2008 Page 42 of 51 Operational Guidelines: Pain Management Services – MDPP Under Development Multi-disciplinary Persistent Pain (MDPP) Programme Note: This service is under development and will be added to the document when the details have been reviewed and completed. April 2008 Page 43 of 51 Operational Guidelines: Pain Management Services – IPM Interventional Pain Management (IPM) Service – Operational Guideline Introduction Interventional Pain Management (IPM) services help clients with persistent pain that results from a personal injury covered by ACC. The services focus on interventions, such as injections to diagnose and treat pain and discomfort. The IPM service facilitates a clients access to specific medical interventions designed to diagnose and/or treat pain. The service is provided by vocationally registered medical practitioners from a range of medical disciplines including anaesthetics, musculoskeletal physicians, and pain specialists. ACC acknowledges that pain is a complex phenomenon and supports an integrated approach. IPM procedures should be undertaken within the wider context of the client’s rehabilitation. Service description IPM services consist of: Assessment services which determine whether a client’s personal injury can be treated by IPM techniques. This usually requires only one clinician’s involvement Treatment services which can begin once ACC has approved the ACC4246 Interventional Pain Management Assessment Report and Treatment Plan (ARTP) and funding for the treatment. Client Referral and Eligibility Criteria The service is only available for clients whose condition is caused by personal injury for which they have cover. This must be clarified before doing an ARTP. The referral to the service provider must be initiated by: A Comprehensive Pain Assessment (CPA), or A vocationally registered Medical Practitioner, or The client’s treating GP. Once the provider is satisfied that all assessment sessions have been carried out, they complete an ACC4246 ARTP and send it to the case owner. April 2008 Page 44 of 51 Operational Guidelines: Pain Management Services – IPM Service Delivery IPM Assessment Services The IPM Assessment Services include: Interviewing the client and detailing their clinical history, including a review of relevant investigations and tests performed to date Arranging access to necessary pathology services and diagnostic imaging services including radiology, MRI and CT scanning, and incorporating the results of those tests in the ACC4246 ARTP Discussing suitable treatment options with the client, including other treatment options where appropriate Completing the ACC4246 ARTP. IPM Treatment Services Treatment begins once the case owner has approved the ACC4246 Interventional Pain Management Assessment Report and Treatment Plan (ARTP) and funding for the treatment. Treatment session(s) involve injection therapies. Injections may be: Diagnostic to determine the source of the pain, or Therapeutic to minimise the pain and improve function. Only one session and procedure is usually involved, although the provider may recommend multiple procedures and sessions. No prior approval in the following circumstances No prior approval is required for the first five treatments for: Peripheral and plexus nerve injections – codes IN10, IN12 Join injections - code IN30 Enthesis injections – codes IN70, IN71, IN72. After five treatments, prior approval will need to be obtained. Practice guidelines for IPM procedures/treatment Recommended guidelines are: ACC IPM Guidelines The Interventional Spine Intervention Society (ISIS) Practice Guidelines Spinal Diagnostic and Treatment Procedures Faculty of Pain Medicine Clinical Guidelines for lumbar, caudal, epidural, and intrathecal injections. The provider also includes information and instructions for the client in each session. April 2008 Page 45 of 51 Operational Guidelines: Pain Management Services – IPM IPM Reporting Templates The template for the Report used in the IPM service are located on ACC’s website under For Providers > Publications and forms > ACC Publications > Pain Management. Reports required for the IPM service are the: ACC4246 Interventional Pain Management Assessment Report and Treatment Plan (ARTP) End of Care Report (there is no template for this report). Payment will be made for each service item on the receipt of a suitable report. The ACC4246 Assessment Report and Treatment Plan (ARTP) Once the provider is satisfied that all assessment sessions have been carried out, they complete an ACC4246 ARTP and send it to the Elective Service Centre by: Email, to ARTPS4ESU@acc.co.nz or Fax, to 0800 222 463. The ACC4246 ARTP will recommend that the client is either: Suitable for IPM treatment, or Not suitable for IPM treatment and outline the reasons why. The report will include: Details of diagnostic tests undertaken The impact of the personal injury on the client’s ability to work Any pre-existing conditions unrelated to, but having an impact on, the personal injury The recommended treatment, and Expected outcomes. End of Care Report Once the treatment session(s) and follow-up visit have been carried out, the provider completes an End of Care Report and sends it to the: Client’s case owner, and Client’s GP, unless the client requests otherwise. April 2008 Page 46 of 51 Operational Guidelines: Pain Management Services – FAQs APPENDIX Frequently Asked Questions (FAQs) for all Pain Management services The following are FAQs which were compiled after the March 2008 Pain Seminars showed that similar questions were being raised at the different venues. This section holds answers on: Pain Disability Prevention (PDP) Programme, and Progressive Goal Attainment Programme (PGAP) Functional Reactivation Programme (FRP) Activity Focus Programme (AFP) Comprehensive Pain Assessment (CPA) Services Provider Listings Pain Management Psychologists Reporting Templates The Pain Compendium Pain Management Training General Questions on the Services Pain Disability Prevention (PDP) Programme, and Progressive Goal Attainment Programme (PGAP) Q: Is there any further training planned for PDP and PGAP? 1 2 3 A: There are, as yet, no confirmed arrangements. However, discussions are under way for further training courses. Providers and ACC staff will be kept up to date and advised of any future arrangements. Q: In the Operational Guidelines is states "Under no circumstances will PGAP services extend beyond the structured 10 sessions". Does that mean that the programme must be delivered within 10 weeks? A: Yes, except for unavoidable situations which necessitate a short break being taken. The programme is designed to be run on consecutive weeks for a maximum of 10 sessions. However, if there is an unavoidable break then longer than 10 weeks is acceptable. Q: What should providers do if they have a holiday break in the middle of running a programme? A: A short holiday break in the middle of the programme is acceptable but any longer breaks should be discussed with the case manager prior to accepting the referral and starting the programme. Q: Is it appropriate to be doing concurrent treatment with the PDP and PGAP? 4 A: Yes. With these programmes treatment as usual can continue, but providers should not be doing a Work Hardening programme and FRP concurrently with PDP or PGAP. Q: Can PDP and PGAP run concurrently? 5 A: No. The case manager and the provider will determine which programme is the most appropriate for the client. April 2008 Page 47 of 51 Operational Guidelines: Pain Management Services – FAQs Functional Reactivation Programme (FRP) Q: Can we (physiotherapists) have clarification about how to integrate pain management in to this programme. 1 A: For information on these requirements please read the service schedule or the details above in these Operational Guidelines. Each contracted vendor has a copy of the service schedule. As agreed to in the contract it is expected that providers undertaking this service have expertise in this area. Q: Why is the funding of the two-hour client contact time with the provider for FRP not in line with the EPN rates? 2 A: This programme has a different contract from EPN and ACC has determined that the remuneration for this is appropriate. There may be a revision of the prices occurring with the budget as a result of the physiotherapy review. This matter will be reviewed at that time. Q: In a group setting, is one-to-one treatment considered to be in line with contract requirements? 3 A: No. The minimum requirement of two hours of one-to-one contact time with the client has been specified in the contract. Group settings/sessions can be included if the clinician deems specifically that a group situation adds value to the client’s programme, over and above one-to-one contact. Q: With the requirement for two one-hourly sessions per week, can this be subdivided into four half-hourly sessions per week? 4 A: Yes. ACC is not determining how the programme should be delivered, merely giving clear guidelines about the minimum amount of time needed to be spent with the client. The feedback from providers and ACC staff following the Activity-based Programme review that there was a huge variation of both time spent with the client, and information that was covered in the programme. ACC needed to clarify this. Manual therapy and FRP 5 Q: Why can’t providers give manual therapy when doing an FRP programme with a client? A: This is in line with the philosophy and purpose of the FRP. Please refer to the section on FRP concurrent treatment on pg 15 in these guidelines. Activity Focus Programme (AFP) Q: What is the role of the medical practitioner in the AFP? 1 A: The role of the medical practitioner is to provide a supervisory role monitoring the response to medications and providing pain education as required. Please see pg 36 in these guidelines under AFP Service Components, or click on the link provided. Q: Why is there no funding available for external gym membership, etc? The funding is for personnel only. 2 A: Each provider has different facilities available for their clients and it is therefore difficult to cover all situations. ACC has designed the new services to help the providers focus on the client’s functioning, and wants to encourage providers to look at reactivating in a broad range of settings, rather than having a gym as the only option. April 2008 Page 48 of 51 Operational Guidelines: Pain Management Services – FAQs Comprehensive Pain Assessment (CPA) Services Q: Why is the CPA not undertaken earlier than 12 weeks? 1 A: CPAs provide an in-depth and comprehensive assessment of a client and therefore should be reserved for only the more complex cases. Clients with complex pain issues are generally identified at this stage. There are other more appropriate pain management options for less complex cases that are utilised in the early stages of rehabilitation. If you have concerns about a particular client then contact the case manager to discuss them. Q: Why was the Initial Assessment dropped from the CPA when it did add value to this assessment (provider query)? 2 3 A: This service was reviewed thoroughly with ACC staff and providers, including the Pain Focus Group and there was no evidence that the Initial Assessment added value to the CPA. It often meant there were unnecessary delays to providing the assessment. There is flexibility in the current system to allow providers to have sufficient contact with clients. Q: Is a psychiatrist as suitable as a medical specialist with a vocational specialty for the CPA? A: Yes. Please refer to the CPA service schedule Part 9.1.2 for the list of Medical Practitioners with vocational registration. Provider Listings 1 Q: Can we have a list of the Pain Management service providers in our area and which services they are providing? A: Please contact your local ACC branch for this information, or go to the Health Service Search (http://healthwise.hosting.co.nz/cgi-bin/search-contracts/). Pain Management Psychologists 1 Q: Can you please clarify which psychologists ACC has contracted with to provide psychological input for any of the Pain Management services they are involved in? A: ACC has contracted with Registered Clinical and Health Psychologists to provide psychological services. These psychologists must have demonstrated to ACC that they have competency to deliver pain management services. Q: With referrals for psychology, can you please clarify which contract clients fit under, ie Pain Management Psychological Services, Psychological Services, or Social Services? 2 A: Those clients with pain related psychological issues should be referred to psychologists who hold contracts for the Pain Management Psychological Service or Pain Disability Prevention (PDP) Programme. Both providers and ACC staff will need to ensure that they clarify which service is required. April 2008 Page 49 of 51 Operational Guidelines: Pain Management Services – FAQs Reporting Templates Q: Can the font size on the template be enlarged and can spell-check be allowed? 1 2 A: Yes. In response to feedback from providers on the difficulty with using these templates on their patient management computer systems the templates have been unprotected. Providers are now able to use spell-check and alter the font size on their own computer systems. ACC will be monitoring the use of these templates and may review this decision at a six-month post-implementation review of the services. Q: Is a signature necessary for auditing purposes? A: Yes. ACC will accept electronic signatures on these documents. Q: Why is the client’s signature required? As there is a time-lag between completing the assessment and having it typed up, it can be difficult to get the client’s signature on the report, especially in rural areas where travelling distances are large. 3 A: The purpose of this requirement is to encourage the client to understand the programme that has been designed for them and therefore increase their motivation to own the programme rather than feel that it is the treatment provider’s programme for them. The Pain Compendium Q: Can psychologists have copies of the Pain Compendium? 1 A: Yes. If they hold a pain contract, ACC will have sent a copy of the Compendium. CD copies of the Compendium (ACC4606) can be ordered via the ACC website at www.acc.co.nz > For Providers>Resources > Pain Management Services. Click here for the Provider resources order form and scroll down to Pain management. Pain Management Training 1 Q: Physiotherapist asked: What opportunities are there for providers to participate in continuing professional development in the field of pain management? A: ACC is not currently involved in this type of training for providers. This training usually contributes to CPD requirements and providers should contact their professional bodies and relevant tertiary institutions for information on post-graduate papers, pain management courses, and training programmes that are available. 2 Q: Are there going to be opportunities for GPs and other provider groups to have education sessions on these services? A: GPs and other provider groups will be given information about these services by the Relationship Managers (RMs) during their usual visits. In many areas RMs are organising educational sessions about pain management and related topics. Please contact your local RM for details of any sessions that might be held in your area. April 2008 Page 50 of 51 Operational Guidelines: Pain Management Services – FAQs General Questions on the Services 1 Q: How do we provide feedback on these services as they go live? A: ACC welcomes your feedback and recommends that you provide this to your Relationship Managers via the Provider Helpline if you do not have their direct phone contact details. 2 Q: Can we have more information on when to use which service? A: A range of services are available based on clients’ needs. Please refer to the ACC4467 Pain Management Quick Reference Guide. This guide details the pain management services available and is available on ACC’s website (www.acc.co.nz) under For Providers > Resources > Pain Management Services. April 2008 Page 51 of 51