Hartmann`s procedure 2014 - Homerton University Hospital
advertisement

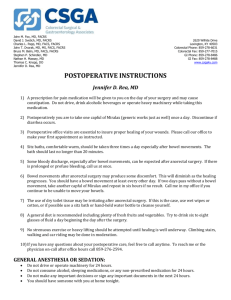
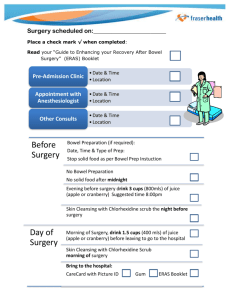
Hartmann’s Procedure Patient Information Colorectal Department Surgical Nurse Specialist Department Incorporating hospital and community health services, teaching and research Introduction This leaflet explains about the procedure known as a Hartmann’s Procedure. Before your operation Before your operation you may have scans and xrays to assess the extent of the cancer. While waiting for your operation it is important to prepare yourself physically. If you can, continue eating a normal diet and take gentle exercise. If you smoke, try and stop before your operation Before the operation you will be asked to sign a consent form to say that you understand what the operation involves. Pre-admission clinic You may have to attend the pre-admission clinic where routine pre-operative tests take place e.g. blood tests, chest x-ray, ECG (electrocardiograph – trace of your heart); listening to your chest and checking your blood pressure. This is to make sure your admission to hospital is as smooth as possible. During this appointment you may see the nurse specialist who will be able to answer any of your questions. Your admission to hospital Your bowel may need to be clear before your operation. You may be given some medicine to clear 2 your bowel and encouraged to drink clear fluids only for one day before your operation. This will help to clean your bowel and reduce the risk of dehydration before the surgery. You will be given: 2 x Bisacodyl tablets and 2 x Picolax sachets (powerful laxative drink) – to be taken the day before the operation. Please read the instruction leaflet you have been given carefully on how to take the bowel preparation. It is important to drink plenty of fluids while taking the laxatives to prevent dehydration. Fluids allowed include water, squash or tea/coffee (without milk) You may continue to drink plain water (not fizzy) for up to 2 hours before surgery. If you have been given Energy Drinks (Nutricia PreOp), drink them as soon as you wake up on the day of surgery before you come to the hospital. Do not eat any food for 6 hours before you come to the hospital for your surgery. Do not take your medications on the day of surgery. Bring all your medication with you to the hospital and the Doctors or nurses will advise you which medications to take. Your operation details 3 Anatomy of the bowel http://www.bowel-control.co.uk/anatomy/index.htm Hartmann’s Procedure This operation involves the removal of the lower part of the large bowel. The affected area will be removed including the sigmoid colon and part of the rectum. With this type of operation you will usually need a colostomy (stoma). This will mean that the faeces (stool) will collect into a colostomy bag attached to the abdominal wall. A cut will be made in your abdomen to create the opening. The waste matter from your body will now pass through this instead of your bottom. Depending on the reason for your operation the colostomy may be temporary to allow the bowel to rest and heal or permanent in certain cases. The sigmoid colon is mainly for the storage of waste matter, thus removing this part has little effect on your bowel function, although it may be a little softer and you may find that you open your bowels more frequently than before. 4 Your consultant surgeon and colorectal nurse will help you understand the procedure involved before your operation. The upper part is brought out through the abdomen wall normally on the right hand side to the surface this is called a Colostomy. The operation time may vary for this type of surgery but is usually around 3 hours. The piece of bowel that is removed is sent to the pathology department for examination. The results are usually available within two weeks of the operation. Diagram showing Hartmann’s Procedure myhealthyfeeling.com Having a stoma What is a stoma? Before your operation the stoma nurse or colorectal nurse will mark a place on your abdomen where the stoma will be placed. They will try to make sure that it is positioned in the best place for you so it does not 5 interfere with the clothes you wear and to make it as discreet as possible. The stoma care nurse will spend time with you before your operation discussing your concerns or questions. You will be given information booklets and shown appliances (Bags). A stoma is an artificial opening through the wall of the abdomen (tummy) to collect waste (stool) into a bag. A bag fits over this to collect your stool and is completely disposable. The bag will need to be changed on a daily basis. The stoma is part of the bowel and is very pink and moist, just like the inside of your mouth. At the beginning it will be quite swollen, but it will shrink down in a few weeks to about the size of a 50 pence piece (although this can vary depending on the type of surgery you have had). The design of stoma bags has improved in recent years and they are now completely disposable and very discrete. They come in various sizes to fit in with your lifestyle; your stoma nurse will show you a selection. Smaller bags can be worn under swimwear and are unnoticeable. You do not need to change the type of clothes you wear, although the stoma care nurse will be able to advise you on certain clothes that can even further disguise the fact you have a stoma bag. There is no reason to change your lifestyle because you have a stoma. You can still work, travel, eat out and enjoy a good social life. Laparoscopically assisted surgery 6 If possible your surgery may be performed using a laparoscopic assisted approach. Laparoscopic colorectal surgery also known as ‘keyhole surgery’ involves inserting laparoscopic (‘keyhole’) instruments through a number of small incisions in the abdomen (tummy).The instrument has a camera attached which projects images on a TV monitor to help with the dissection, removal of the diseased portion and thereby performing the entire surgery through a slightly larger incision. The main aim of having this type of surgery is to: - Reduce hospital stay, minimise hospital infection - Quicker recovery - Minimise scarring - Reduce discomfort following surgery Choosing not to have this operation will depend on your diagnosis following investigations but will include the continuation and worsening of the symptoms. The bowel is likely to become obstructed leading to emergency hospital admission and possible emergency surgery. Risks or complications of surgery Most operations are successful. However, every procedure has risks and potential complications. Those that are most relevant to the operation you are to have are listed below. If there is anything you are unsure about you can discuss this with your Doctor or Nurse. 7 If you are elderly or have a lot of other serious medical conditions, we have a specific complex preoperative assessment service. Where you will see a specialist doctor, cardiologist, Intensive care doctors and specialist allied health care professionals who work together to assess and plan your care if you have an operation. The risks and complications can be divided into three areas:1. Complications of the anaesthesia 2. General complications of any surgery 3. Specific complications of this operation 1. Complications of the anaesthesia Your anaesthetist will talk to you about the risks of an anaesthetic. 2. General complications of any operation Pain – this can occur with any operation. You will be visited regularly post operatively by the pain team who can regulate the pain relief to fit your personal needs. Bleeding – this can occur during or after the surgery. If this happens you may need a blood transfusion or very occasionally another operation may be required. If you have any religious or personal objection to having a blood transfusion there are alternatives which will be discussed with you. Infection in the surgical wound – this would usually be treated with antibiotics or occasionally further surgery (risk: 3-7 in 100). 8 Unsightly scarring - this is more likely if the wound has become infected. A hernia – this can occur in the incision scar when the deep muscles fail to heal or around the site of the stoma. If the hernia appears as a bulge around the incision line it is called an incisional hernia, if it occurs as a bulge around the stoma it is called a parastomal hernia. If this causes problems, you may need another operation. Blood clots – These can occur in the legs (thrombosis) and can move to the lungs to cause breathing problems. You will be asked to wear anti-thrombosis tights (long socks) and will be given injections to reduce the risk. This is the same thing that can occur during a long airplane flight (economy flight syndrome). Difficulty passing urine – You will have a catheter inserted at the time of the operation which will remain in place for approximately 7 days. Occasionally, when the catheter is removed, you may have difficulty passing urine. This is more common in men and/or if you have had difficulties passing urine prior to the operation. Chest infection – the physiotherapist will give you deep breathing exercises to help prevent a chest infection. 3. Specific complications of this operation (Hartmann’s Procedure) 9 Adhesions – this is where scars form inside the abdomen. This can occur following any operation on the abdomen and does not usually cause any problems. However, it can sometimes lead to bowel obstruction many years later. Sexual disturbance – the nerves that supply the sexual organs in both men and women run very close to the rectum. When the cancer is removed these nerves can be damaged which may lead to impotence in men and vaginal dryness in women. Impotence following rectal cancer surgery is one of the licensed indications for receiving Viagra (a drug used to overcome impotence). Before your operation the surgeon will visit you to discuss the operation and you will be asked to sign a consent form. It is important that you fully understand what operation is planned and what the likely benefits and possible side effects are. After your surgery Following surgery you will go back to the ward. The nurse on the ward will carry out regular observations on you. You will be allowed to drink fluids freely and to eat when you feel able. When you wake up you will find that you are attached to several tubes. These may be: A drip in your arm or neck, which gives you the extra fluids that you require. A PCA System (patient controlled analgesia), which is another tube in the 10 arm that gives you a painkiller; you will be able to control the amount of painkiller you have by pressing a button connected to a pump. Painkiller can also be given as an epidural infusion via a drip in the middle of your back. The anaesthetist will discuss these options with you. A catheter (tube), which goes into your bladder to drain urine away. This is so the amount of urine you pass can be accurately measured. You may have a drain which is a small tube which clears away any oozing fluid around the operation site. These tubes are put in while you are under anaesthetic, (except the epidural), and will be removed within the first 1-3 days after the operation. You will be in hospital for 4-6 days. After surgery, you can eat and drink as normal. To speed up your recovery, you will be given 3 supplements drinks each day. These will be given for 3 days after your surgery. Managing after surgery You can eat and drink soon after your surgery. If the bowel function is slow to start food and drink may be restricted for a few days. To speed up your recovery, you will be given 3 supplements drinks each day. These will be given for 3 days after your surgery. It is important to try and move around soon after the operation. Becoming mobile will help you to recover 11 quickly from the operation and also reduce the risk of complications. You will be helped to sit out of bed on the first day after your surgery and by the 3rd day, you will be helped to walk around the ward. The physiotherapist will help you to walk up and down stairs if you have them at home. The Stoma Nurse Specialist will start teaching you to look after this on the 1st day after surgery until you are able to manage this yourself. This usually takes 3-4 days. She will give you support during your recovery on the ward, and also once you are at home. After the operation, rest is very important as part of the recovery process, so it is advisable to restrict the number of visitors coming to see you so you don’t get overtired. Visiting time is between 11.00am – 12.30pm and 4.00 – 8.00pm. Only 2 visitors are allowed at a time. Going Home The medical staff will be able to advise you if some movements are restricted, like kneeling or bending down. This may last for a short period of time, as you get better you will be able to resume your daily activities. The stoma care CNS will arrange your supplies for home; they will visit you within the first week of discharge home. If you need any additional help the district nurse will be asked to visit. 12 For the first week or so you will feel tired and weak when you get home. It is therefore important that you rest although it is not good for you to stay in bed all the time. You should try gentle exercise first like walking around the house or to the end of the street. Your appetite may be reduced so try eating little and often to begin with. For most people it will take 6-8 weeks to recover from this type of operation. You may feel some pain and ‘twinges’ around your wound for several months. This is normal as it takes a while for full healing to take place. Taking a mild painkiller will help you feel better and help with recovery. For the first six weeks you are advised not to lift anything heavy such as shopping or wet washing, and not to do anything strenuous like digging the garden or mowing the lawn. You should not drive until you can do an emergency stop without hesitation that your wound will hurt. To test if you could do an emergency stop, lift both feet off the ground at the same time. If it does not cause you abdominal pain you would be able to do an emergency stop. It is advisable to check your car insurance for any clauses regarding driving after an operation. When you get home you may find that your bowel habit is still unpredictable. When you have had some of your large bowel removed you may find your stools are slightly loose, over time this will resolve itself. You may also find that you need to change or empty the stoma bag frequently. This could be anywhere between 1-4 times per day. If your bowel 13 habit does not settle, there are medications that can help . You may also get the feeling you need to open your bowels from your back passage, or you may pass some mucous, this is normal after the operation. If you are worried please discuss it with the stoma care nurse or your doctor. The length of time before you are fit to return to work will be individual and dependent on the type of work you do. Once you have recovered from your operation there is no reason why you can’t go back to your normal sex life. However, operations on the rectum can cause damage to the nerves that connect to the sexual organs. If there is damage men may find in difficult to get or maintain an erection, and may have problems with ejaculation. Women may experience pain when having sex or a lack of lubrication fluids (natural fluids in the vagina). If you do have problems talk to you doctor or specialist nurse. Dukes’ Staging Doctors use a system to describe the different stages of cancer of the large bowel – Dukes’ staging. The staging system is based on the depth the tumour has invaded through the bowel wall and whether any cancer has spread to the lymph nodes (lymph node metastasis). After your operation the histopathologist will examine the cancer under the microscope, we usually have 14 the results within 14 days and will then be able to tell you about the stage of your bowel cancer. Dukes’ Stage Dukes’ A Extent of cancer The cancer is confined to the bowel wall The cancer has spread through the full thickness of the bowel wall, but the lymph nodes are not affected. The cancer has spread to the lymph nodes. The lymph nodes are part of the lymphatic system, which is part of the body’s natural defence against infection. This is one of the first places the cancer can spread to. Dukes’ B Dukes’ C Medical Terms and Words These are some of the medical words and terms you may come across during your investigation and treatment. Abdomen Adjuvant therapy Anaemia Analgesia Anus Caecum Tummy or belly Chemotherapy and radiotherapy in addition to surgery A reduction in the number of red cells, haemoglobin (iron) or volume of packed red cells in the body Pain killers such as paracetamol and morphine The opening to the back passage The first part of the large intestine 15 forming a dilated pouch into which the ileum, the colon and the appendix opens. Chronic Symptoms occurring over a long period of time Chemotherapy Drug therapy used to attack cancer cells CNS (Clinical A qualified nurse that has Nurse specialist) specialised in a particular field of care. Colon The large intestine (bowel) extending from the caecum to rectum Colonoscopy Inspection of the colon by an illuminated telescope called a colonoscope. Colorectal Surgeon who specialises in the Surgeon treatment of conditions in the large bowel and rectum including bowel cancer. Colostomy Surgical creation of an opening between the colon and the surface of the body. Part of the colon is brought out of the abdomen creating a stoma. A bag is placed over this to collect waste material. Constipation Infrequent or difficulty in the passage of bowel motion stool (faeces). CT scan (CAT (computerised axial tomography) scan) A type of x-ray. A number of pictures are taken of the abdomen and fed into a computer to form a detailed picture of the inside of the body. 16 Defaecation Diagnosis Diarrhoea Electrolytes Enema Exacerbation Faeces Inoperable Laxative Lesion Malignant Mucus Oncologist Palliative care Pathology The act of passing faeces (having your bowels opened) Finding out what is wrong with you An increase in frequency and liquidity of bowel motions Salts in the blood e.g. Sodium, potassium and calcium A liquid introduced into the rectum to encourage the passing of motions An aggravation of symptoms The waste matter eliminated from the anus (other names – stools, motions, poo). A growth or tumour that can not be surgically removed Medicine or tablet that acts to cause emptying of the bowel. This may be by purging (irritating the lining) or increasing the volume of stool (bulking) A term used to describe any structural abnormality in the body Cancer A white, slimy lubricant produced by the large bowel A doctor who specialises in cancer care using drugs and radiotherapy Improving the quality of life by providing support and the control of pain and unpleasant symptoms. The study of the cause of the disease 17 Radiotherapy Rectum Sigmoid Sigmoidoscopy Stricture Suppository Tumour Ultrasound The use of high energy rays which attack cancer cells The large intestine, above the anus (the back passage) The portion of the colon shaped like a letter ‘S’ or ‘C’ extending from the descending colon to the rectum Inspection of the sigmoid colon with an illuminated telescope called a sigmoidoscope The narrowing of a portion of the bowel A bullet-shaped solid medication put into the rectum An abnormal growth which may be benign (non-cancerous) or malignant (cancer) Use of high-pitched sound waves to produce pictures of organs on a screen for diagnostic purposes Homerton Hospital Health and Cancer Information Centre Based at the front of the hospital Tel: 020 8510 5191 (Mon – Friday 9am – 5pm) Email: healthshop@homerton.nhs.uk Homerton Health Shop is a drop-in Health and Cancer Information Centre, based at the main entrance of the Trust. Macmillan Cancer Information and Support Manager provides cancer information, financial, practical and emotional support to anyone affected by cancer, their relatives, carers and friends. Homerton Hospital PALS (Patients Advice & Liaison Service) PALS is based in the main entrance of the hospital. Tel: 020 8510 7315 (9am – 5pm) 18 Email: pals@homerton.nhs.uk PALS provides confidential information and support, helping you to sort out any difficulties or concerns you have whilst in hospital, guiding you through the different services from the NHS. Useful Contacts Beating Bowel Cancer Harlequin House, 7 High Street, Teddington, TW11 8EE General Helpline: 08450 719 301 Nurse Advisory Service: 08450 719 301 (9.00am – 5.30pm) Email: nurse@beatingbowelcancer.org Website: www.beatingbowelcancer.org Provides expert knowledge support, raising awareness and information about bowel cancer so that individuals can make their own informed decisions of their treatment. Bowel Cancer UK 4 Rickett Street, London SW6 1RU Tel: 020 7381 9711 Advisory line: 0800 840 35 40 (10.00am – 4.00pm) Email: advisory@bowelcanceruk.org.uk Web page: www.bowelcanceruk.org.uk Advisory line staffed by specialist nurses providing advice and information service for all those affected or concerned about the disease. Bowel cancer information in other languages available. Cancer Research UK Cancer Research UK, P.O. Box 123, Lincoln's Inn Fields, London WC2A 3PX Cancer information nurses: 0808 800 4040, 9am - 5pm Email: cancerhelpuk@cancer.org.uk Website: http://www.cancerresearchuk.org/cancer-help/ 19 Cancer Research UK is dedicated to cancer research, provides information on site specific cancers and influences public policies. The Website provides information for bowel cancer patients. Hackney Citizens Advice Bureau Local Office: 300 Mare Street, London E8 1HE Tel: 0870 126 4013 Website: http://www.eastendcab.org.uk/ Mare Street office offers drop-in clinics Monday-Thursday from 8.30am. Friday doors open at 9.30am. Advice line operates Tuesday and Wednesday from 1pm – 3pm and 10am-12pm (for clients with mobility problems). Tel: 0844 499 1195. The Citizens Advice service helps people resolve their legal, money and other problems by providing free information and advice from over 3,000 locations, and by influencing policymakers. Colostomy Association 2 London Court, East Street, Reading, RG1 4QL Tel: 0118 939 1537 Helpline: 0800 328 4257 (24 hour) Email: cass@colostomyassociation.org.uk Website: www.colostomyassociation.org.uk Provides support and advice for colostomates, their families and their carers. Free literature and information is available about all aspects of living with a colostomy. Core – Fighting Gut and Liver Disease 3 St Andrews Place, London, NW1 4LB Telephone: 020 7486 0341 Email: info@corecharity.co.uk Web page: www.corecharity.org.uk Fund research in order to prevent, cure or treat digestive disorders and provide information for sufferers, their families and friends. Ileostomy and Internal pouch support group Peverill House,1 – 5 Mill Road, Ballyclare, Co. Antrim, 20 BT39 9DR. Tel: 0800 0184 724 (Office hours) Email: info@iasupport.org Website: www.iasupport.org/uni_contact.aspx Aims to help anyone who has had or is about to have their colon removed and has an ileostomy or internal pouch. Provides advice, information and leaflets. Institute for Complementary Medicine (ICM) 32-36 Loman Street, London SE1 0EH Tel: 0207 922 7980 Email: info@icnm.org.uk. Fax: 0207 922 7981 Website: http://icnm.org.uk/ Provides the public with information on Complementary Medicine Macmillan Cancer Support 89 Albert Embankment, London SE1 7UQ Macmillan cancer line: 0808 808 0000 (9am – 8pm) Website: www.macmillan.org.uk Provides specialist advice and support for cancer patients and financial advice and grants for people with cancer and their families. NHS Choices http://www.nhs.uk/Pages/HomePage.aspx The Polyposis Registry St. Mark’s Hospital, Northwick Park Hospital, Watford Road, Harrow, HA1 3UJ Tel: 020 8235 4270 Email: info@polyposisregistry.org.uk Website: www.polyposisregistry.org.uk Provides support and information to people who have, or may have, the familial adenomatous polyposis (FAP) gene, and so are at greater risk of developing bowel cancer. Other sources of information 21 - www.rcoa.ac.uk “You and your Anaesthetic” - www.rcseng.ac.uk Important information Please remember that this leaflet is intended as general information only. It is not definitive. We aim to make the information as up to date and accurate as possible, but please be warned that it is always subject to change. Please, therefore, always check specific advice on the procedure or any concerns you may have with your doctor. Hand Hygiene In the interests of our patients the trust is committed to maintaining a clean, safe environment. Hand hygiene is a very important factor in controlling infection. Alcohol gel is widely available throughout our hospitals at the patient bedside for staff to use and also at the entrance of each clinical area for visitors to clean their hands before and after entering. Other formats If you require this leaflet in any other format e please speak to your clinical nurse specialist (Keyworker). Reference The following team members have been consulted and agreed this patient information: Consultant, Clinical Nurse Specialist (Keyworker), Macmillan Cancer Information and Support Manager and Patient. Produced: Colorectal team Reviewed: May 2014 Next review date: May 2016 Homerton University Hospital NHS Foundation Trust Homerton Row, London, E9 6SR T 020 8510 5555 W www.homerton.nhs.uk E enquiries@homerton.nhs.uk 22