2. Synthetic Ligaments: Past - Present - Future
advertisement
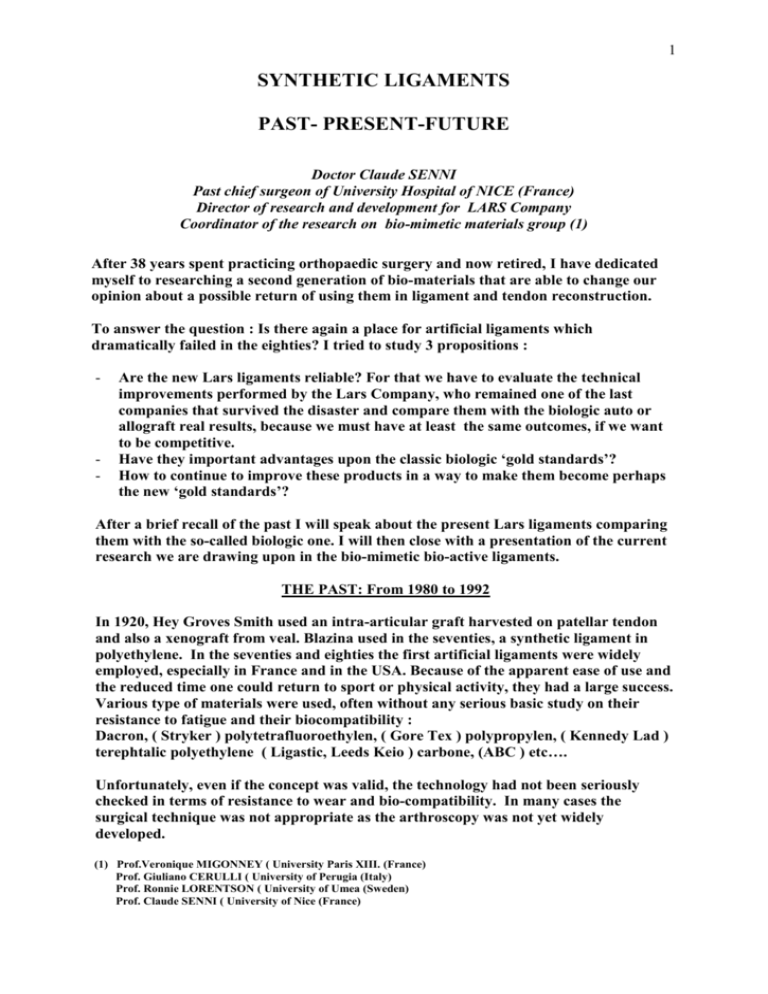
1 SYNTHETIC LIGAMENTS PAST- PRESENT-FUTURE Doctor Claude SENNI Past chief surgeon of University Hospital of NICE (France) Director of research and development for LARS Company Coordinator of the research on bio-mimetic materials group (1) After 38 years spent practicing orthopaedic surgery and now retired, I have dedicated myself to researching a second generation of bio-materials that are able to change our opinion about a possible return of using them in ligament and tendon reconstruction. To answer the question : Is there again a place for artificial ligaments which dramatically failed in the eighties? I tried to study 3 propositions : - - Are the new Lars ligaments reliable? For that we have to evaluate the technical improvements performed by the Lars Company, who remained one of the last companies that survived the disaster and compare them with the biologic auto or allograft real results, because we must have at least the same outcomes, if we want to be competitive. Have they important advantages upon the classic biologic ‘gold standards’? How to continue to improve these products in a way to make them become perhaps the new ‘gold standards’? After a brief recall of the past I will speak about the present Lars ligaments comparing them with the so-called biologic one. I will then close with a presentation of the current research we are drawing upon in the bio-mimetic bio-active ligaments. THE PAST: From 1980 to 1992 In 1920, Hey Groves Smith used an intra-articular graft harvested on patellar tendon and also a xenograft from veal. Blazina used in the seventies, a synthetic ligament in polyethylene. In the seventies and eighties the first artificial ligaments were widely employed, especially in France and in the USA. Because of the apparent ease of use and the reduced time one could return to sport or physical activity, they had a large success. Various type of materials were used, often without any serious basic study on their resistance to fatigue and their biocompatibility : Dacron, ( Stryker ) polytetrafluoroethylen, ( Gore Tex ) polypropylen, ( Kennedy Lad ) terephtalic polyethylene ( Ligastic, Leeds Keio ) carbone, (ABC ) etc…. Unfortunately, even if the concept was valid, the technology had not been seriously checked in terms of resistance to wear and bio-compatibility. In many cases the surgical technique was not appropriate as the arthroscopy was not yet widely developed. (1) Prof.Veronique MIGONNEY ( University Paris XIII. (France) Prof. Giuliano CERULLI ( University of Perugia (Italy) Prof. Ronnie LORENTSON ( University of Umea (Sweden) Prof. Claude SENNI ( University of Nice (France) 2 After 4 to 5 years of general satisfaction the failures became evident : acute aseptic synovitis ( 16% of cases ), early rupture in the first 4 months, and high rate failure within 4/5 years ( rupture and lengthening ). Making it not only to abandon them but also reject them as if they were diabolic objects. And this without, after more serious study confirm, give them a second chance. After the way to operate with synthetic ligaments was abandoned the autografts, harvested on the patient, for some years the patellar tendon, first leaving its tibial insertion hoping a better vascular ingrowth, then free ( Dejour), were defined as the ‘gold standard’. THE PRESENT: From 1993 to the present day To estimate the opportunity to return to synthetic ligaments we have to answer this question : Are the biologic grafts 100% satisfactory? If so, we do not need to do anything else. However, it doesn’t seems so. According to the results of many objective analysis, also confirmed by the important increase in the use of allografts, demonstrate that the autografts are not fully satisfactory in all indications. So I tried to assess the real results, being as objective as possible, the advantages and disadvantages of the autografts and allografts. Generally, today we use: -Autografts : bone to bone patellar tendon, -Hamstrings ST.G, which are mostly used. -Allografts -Rarely xenografts. BIOLOGIC GRAFTS : A) AUTOGRAFTS : These grafts pretend to be ‘gold standard’ because they give the illusion to be made of biologic human tissues and therefore have more opportunities to be completely integrated by the patient’s organism. However, if we analyse with a critical eye, we can recognise some disadvantages. AUTOGRAFTS INCONVENIENTS : - - - The necessity to harvest tissue from the patient adds further damage to an already damaged knee with destruction of the proprioceptivity neuroreceptors. Regarding hamstrings, several studies show that their removal can create a diminution of the rotational control and consequently decrease the protection of the new ligament during rotational stresses. To have a good graft resistance it is necessary to make large tunnels, 8, 9, 10mm and sometimes more. In the first few weeks following the implantation, the graft resistance decreases (Amiel, Shino) reaching only 30% of the initial one and after 9 years the final resistance is only 50%. This explains why the return to physical activities (sport) must be reported within 7 to 8 months. A great number of rehabilitation sessions are necessary due to the harvesting of tissues. In the following months lengthening of the graft is frequent, especially for hamstrings. 3 - - In case of failure or iterative rupture after a new incident it is necessary to harvest a new tissue on the wounded knee adding another lesion to the precedent one and in some cases it is harvested on the opposite healthy knee. Patients are generally young and return to sport practice, so new incidents are frequent. The large tunnels may create difficulties to change the position of the new tunnels in case of a wrong position of the previous one. Beyond these disadvantages the autografts have possible : COMPLICATIONS CONNECTED TO THE HARVESTING rarely, graft ruptures when it is too thin - fracture of the patella - retraction of the PT with patella baja - permanent extension defect - cyclops syndrome - anterior lasting pain: this prohibits the return to sport and professions which requires a kneeling position. - deficit of the quadriceps - large haematomas - scars - U.S. studies include also the inconvenience when the graft falls to the ground. It is true that these complications become less frequent with the improvement of the technique. Their frequency is very variable. In Europe it is valued from 1,5 % ( Prof. BRANCA Italy) to 82 % on BTB (Prof. Paessler. Germany). They probably don’t include the same complication parameters. But nevertheless with synthetic ligaments we have 0% of these complications because we do not have to harvest anything. AUTOGRAFTS ADVANTAGES : The main advantages could be considered : a) the durability of the graft b) the high rate of good results; it is generally estimated between 80 to 90% of cases. While trying to control these statistical judgments, I made a summary of some hundred of worldwide results. It was very difficult to make a serious valuation on the basis of percentage calculations on a significant number of cases. 1) Most of the results are retrospective and non-randomised. The patients had been checked by the surgeon himself and often that surgeon had to deal with less than 100 cases with 5 years follow up. 2) The results have poor value because they are bias : in many cases the number of patients, which aren’t found again, can distort the results because these patients, perhaps, are those who had a failure. In many studies the percent average rises to more than 10 % of not found again patients, and often increases even more with a follow-up over 10 years. In the past, in my practice, it was mandatory to consider a patient not seen again as a case of failure. 4 3) The variables are very high making it difficult to compare statistics. - - Populations of men and women in different percentages, practising or not practising sport, in a professional or amateur way, young or over 35/40 years old, with a high motivation or necessity to return to sport or quicker active work. The lesions are also various, fresh or chronic, ACL isolated or with other peripheral lesions, with or without meniscus lesion or cartilage defects etc… There are also an infinity of variations in the techniques used : position of the tunnels (9, 10, 11 hours), notch plasty or not, means of fixation, choice of the tendon harvested etc… 4) What can we call a good outcome? - Patient satisfaction, his possibility to return to former activity ? - Surgeon satisfaction ? - or clinic objective and instrumental examination ? A very serious study performed by Nicolas DUVAL ( Montreal Canada ) shows that there is no correlation at all between the patient’s satisfaction and the objective examination. The multiplication of the scores used for the valuation shows also a difficulty to gain reliable statistics for compare technologies : IKDC , KOOS, SF-36, LYSHOLMTEGNER, ARPEGE etc…, including more or less the related patient satisfaction. Many athletes are able to return to sport even with a torn ACL . 5) We have few systematic arthroscopic revisions with histology of the graft. We don’t really know the percentage of true estimate, “legamentisations” ( Amiel) reached by the autografts. For this reason I prefer, to value autografts (and also allografts) versus synthetic consider the percentage of failures instead less or more successful outcomes. A failure understood as : graft rupture, loosening of the insertion point, lengthening more than 5 to 7mm, pivot shifts remaining, sepsis, acute synovitis, or the necessity of revision surgery for any reason, is very much reliable. There are less chances to have a subjective interpretation about a more or less, good, pretty or bad result. The failure is not subject to interpretation : it is or it is not a failure case. Nevertheless several studies give a rate of good results near to 80% but some to 60%. S.Y. WOO (Pittsburgh) estimate a rate of failure by autograft to be 25% of 200 000 cases operated in U.S.A. and he says that in the last 5 years the rate of revisions increased by 50 %. Prof. Christel (France) studied 100 000 cases and found 21% of failures. He retains that, “Surgery improves the pre-operative level but doesn’t allow the patient to recover, on average, the pre-operative level.” A Swiss metanalysis with a 10 year follow up pointed out that, while 75 % of patients think to be better after surgery, only 53% declared to have been able to return to the same sporting activity they had been doing before the accident (Prof. Cristel). Therefore, I don’t think that the so-called biologic autografts can be defined as ‘gold standard’. In any case, it is necessary to find other possible grafts, avoiding “robbing Peter to pay Paul” by harvesting, respecting the proprioceptivity and vascularisation and cutting no bridges in case of further failures. 5 B) THE ALLOGRAFTS: Could allografts meet the below requisites? Sterilized or fresh frozen allografts after aseptic harvesting have the same advantages as synthetic ligaments in terms of : - - no harvesting, therefore no complications on the donor side available but less than the synthetics : by lack of donors or if the graft falls there is a problem to get another one immediately. On the contrary, to the synthetic as we need only to open another box. in the U.S.A. allografts seem to have good results and are used in primary reconstruction. This is not widely accepted in Europe where they are, at this time, used mainly in revisions, or for multiple reconstructions. However, there are many : INCONVENIENTS The fibroblastic in-growth is slower than with autografts. According to Shino it may last more than two years and graft resistance decreases significantly. In many cases “ligamentisation” doesn’t exist at all and progressive lengthening over 8mm has been observed in many studies. Immune reactions have been pointed out and could be the reason for the tunnels widening. The risk of disease transmission exists even if it is rare. If allografts are sterilized by gamma rays it is necessary to choose a dose of over 3 megarads to guarantee sterility against virus. However, with this dosage the collagen structure is damaged, weakening the graft. It is possible to use, as US tissue banks do, a dosage of 1,5 to 2,5 megarads which is less aggressive for the collagen but not strong enough to have a total guarantee against virus. The fresh frozen grafts with sterile harvesting are used more in Europe. They seem to have better integration but the follow ups are still too short to value true results for durability and the stability reached after surgery. In some cases a total eradication of the graft about one year after reconstruction surgery was observed. Even taken into account the above doubts and the quality of the results the major problem with this system is the real risk of transmitting bacterial infections (Clostridium spore infection killed 3 people in the US) or viral infections (hepatitis, HIV and so on). In spite of rigorous precaution when harvesting the graft in a sterile theatre and during the conditioning, the risk of contamination, even if bounded, still remains. Firstly, because there is a window period between the moment of the contaminated donor and death, making the infection non-detectable and secondly, human error is always possible. ( It has happened in the U.S.A. and recently in Italy with five contaminations with HIV and hepatitis B). In a recent Study, Singhal of the Kentuky University on 125 ACL reconstructions with allografts , at 4 years follow up there was 25 % of failures in the over 25 years group and 55 % failures in the under 25 group. The medium failures rate for the two groups was 38% . 6 This proves to me that using a method which can provoke the death of a patient who needs a ACL reconstruction ,for so poors results must not be considered to be a future ‘gold standard’. The third possibility is the use of SYNTHETIC LIGAMENTS : After failed success in the past they suffered, even 25 years after, they are faced with a strong prejudice from many surgeons. However, it is not a reason, when technology is not ready at a time to realise a valid concept , to abandon it completely and definitively. It was technology and the technique used which weren’t as advanced enough to realise a good concept. We now witness a come-back to metal/ metal frictions systems , resurfacing prostheses, and so on. Like so many human success stories that start with a simple idea, are confronted with failures in the realisation, then reflection on the reasons for failure allow improvement and then success. The Lars company remained the one of the only companies to continue research into synthetic ligaments because they were aware of potential advantages that could become of such a project. To reach this aim it has been mandatory realise studies on mechanic behaviour, biocompatibility, fibroblastic in-growth and particular surgical techniques imposed by use of synthetic ligaments. SYNTHETICS ADVANTAGES : they are numerous. - - no harvesting tissues from the patient. time for surgery reduced to 30’ generally. necessity of little tunnels ( 6,7, 8 mm). no complications tied to harvesting tissue. Maximum respect to the skin, capsula, tendons and bone. This is because no damage is created to the proprioceptivity neuroreceptors, explaining an immediate recovery and excellent functionality. day surgery possible ( minor bleeding, low pain). minor rehabilitation sessions necessary ( often within 1 month to 6 weeks). full availability in case of failure, revisions are easier with narrower tunnels. no risk of the device being contaminated ( except from nosocomial infection that may occur from asepsis error in the theatre by surgical team). a quick return to activity even to high intensity sports ( 6 to 8 weeks,) with excellent functionality and without any of the disadvantages that exist with auto or allografts. AND WITH SYNYHETICS NO-ONE HAS EVER BEEN KILLED ! SYNTHETICS INCONVENIENT : As demonstrated below, terrible acute aseptic synovitis, which existed in the past are now eliminated. This was a major inconvenience. We have also increased in an important way the resistance to wear. With this is mind, only one more point remained to be solved. As with every artificial product inserted into the human body and submitted to mechanic stress, artificial ligaments should have a limited life-span. 7 Why then are synthetic ligaments refused to be used? We must demonstrate that without the disadvantages of the biologics grafts, we have at least the same rate of good results and failures and with these advantages make the risk of non definitive behaviour acceptable. First, I will explain what the Lars Company has done to improve artificial ligaments. Then I will explain the results after 13 years of use. I) To increase ligament life-span We had to increase : - The resistance to continue traction after 24 hours - The resistance to flexion, traction and torsion combined stresses The increase was obtained thanks to: - polyester (terephtalic polyethylene). Polyester was chosen because of its high resistance to traction ( 3700 N for 80 fibres AC 80) ligament used for body weight under 80 kg and very good elasticity. - A new textile structure, which keeps its shape under stress, so-called open or free longitudinal fibres structure for the intra-articular portion. The longitudinal fibres going from one extremity of the ligament to the other are fully independent between them, and are free in the articular part. In the tunnels section they are joined together by transversal thin fibres making them cylindrical for easy use. So, the stress strength are applied along the longitudinal fibres axis . These fibres are more resistant to deformation than a deformable knitted or weaved structure. This allows: - - To avoid rubbing which happens between the transversal and longitudinal fibres found in knitted or woven tissue, producing chewing of the longitudinal by the transversal one. ( This was demonstrated by the French Textile Institute engineers as it is similar to what happens when a tennis racket’s strings rub against each other). It reduces, in an important way, the debris production which created chronic synovitis in the past. And eliminates transmission of rotational forces in the tunnel, lowering risks of tunnel widening. The Lars ligament ( for ACL rupture ) has a pre-twisted physiologic form reproducing the natural one and reducing fatigue under torsion. This makes half of the fibres work alternately in extension and in flexion. Of course there is a left and a right ligament for ACL. The open fibres allow a better fibroblastic in-growth because they have a high porosity ( 400 microns have been found in the knitted part of the tunnels compared to 50 microns found in some ligaments in the past.) The poor results in the eighties were also due to an approximate surgical technique. It was estimated that close to 50% of the failure cases in the eighties were caused by technique errors as : non isometric position of the tunnel insertion, too much anterior or lateral or medial of the graft, tunnels not lined up, creating killing angles and excess of tension creating cartilage stresses with lesions. One very important modification was to respect the ACL stump in which the Lars ligament must be introduced along its axis and shrouded in, to have blood and cells support for a good fibroblastic in-growth, maintaining the proprioceptive neuro- 8 receptors. This rule changed our opinion about synthetic tissue as it is no longer considered to be an inert prosthesis but as a mere scaffold for collagenic ricolonisation. - The use of arthroscopy was also of great aid for more precision, as were the improvement of the rehabilitation protocols. All these technological advances were questioned in a mechanical study by SERCOVAM ( A French laboratory studying wear fatigue of materials). The results, after 22 millions cycles in flexion traction torsion, similar to about 14 years of knee use, showed no rupture at all and a very low residual elongation of 1,9mm. Clearly, the remaining resistance is equal to 40% of the initial resistance. II) Elimination of the acute aseptic synovitis This was obtained by enhancing the bio-compatibility. Research conducted by the French institute of textile found that the rejection of the synthetic ligaments due to aseptic acute synovitis was not caused by the terephtalic polyethylene (polyester) but by mineral or natural oils and greases used to obtain an emulsion after the polymerisation was added to make the carding and spinning procedure easier. These oils ( isopalmytate, isostearate of butyle, etc…) are used for the, ‘ensimage’ procedure. They are very cytotoxic and must be fully eliminated by washing off with much accuracy. The ‘desensimage’ procedure used to eliminate them was very poor in the eighties. Only five stages were performed and they were very insufficient. The Lars procedure now uses 11 steps performed by a computerised machine. Every day each ligament is washed in 1 litre of solvent ( ether, toluene hexane, cyclohexane, etc…). Every one is appropriate to eliminate each fraction of the cytotoxic oils. Every 24 hours a sample of the liquid is checked by chromatography and washed continuously, with the solvent, until the oil concerned has been eliminated. After this preparation the ligament should already be sterile and conditioned in a white room, sent to gamma ray sterilisation with random control of sterility and absence of bacterial toxins. The whole procedure lasts from 1 month to 6 weeks. Since this accurate purification became into existence and after 50.000 ligaments implanted world wide in 14 years there have been no cases reported with related acute aseptic synovitis. III) Reduction of chronic synovitis The reduction of chronic synovitis was obtained through the elimination of debris production thanks to free fibres and better bio-compatibility. Thanks to better microporosity, after 6 weeks the new ligament is covered by fibroblastic tissue and synovial membrane. So, if any debris did exist it isn’t free to go into the articulation. Now, no more traces of polyester debris are found in the synovial liquid. Some chronic effusions have been seen in a inferior rate to those observed with biologics (under 3%), generally resolutive in 3 months. When they become chronic arthroscopic revisions generally show an ignored or new lesion, as little meniscal flap, chondral defect, plica, etc…Sometimes there are consequences of lasting pivot shift. 9 AC 80 Ligament Fatigue test resistance Fibroblastic in – growth Fibroblastic tissue LARS ligament Day + 45 10 CLINICAL RESULTS Since 1993 more than 25.000 Lars have been inserted worldwide, not only for knee surgery but also for shoulder ( acromion clavicular dislocation, rotators cuff lesions), Achille tendon rupture, patellar tendon, ankle instability, hand and wrist surgery. Not one acute aseptic synovitis was reported at this time. For cruciate ligaments we have a good rate of results. After more than 5 years of average follow up, it was close to 90 %( from 83 to 96 %) according to various authors. ( On request we can supply the results. See the bibliography). Unfortunately, we lack randomised studies which are not easy to access. Prof. Nick Duval (Montreal Canada) is drawing a prospective randomised study BTB tendon versus Lars. The results from two years of follow up were published in GBGS and Knee journal and in 2007 the results from 5 years has been published. The results found in the first two years follow up gave similar results to those found with the biologics. In October 2007 three randomised studies were drove by N.DUVAL versus BTP tendon. One studying the results of Lars in fresh lesions, one in chronic lesions and one in revisions surgeries. The results, as if better for fresh lesions are similar, with the difference that the synthetic allowed a return to sports activities in 6 weeks with a return to the same performance level as prior the accident in 95% of the cases. We also have interesting results ( Maheras Athens ) from 100 professional class A basket ball and soccer athletes who at 4 years had a 92% returned to sport at the same level. Personally, I have checked 2700 ACL implantation carried out in Italy from 1996 to September 2007 and no synovitis was found. The good rate of results is close to 95% and the return to sport is close to 92% ( Prof. Cerulli SIOT Congress 2005.) . Failures, for the moment, occurred in 27 cases ( Oct 2007), ruptures, sepsis, loosening of fixation, revision for unknown reason. The average is now under 1,5 %. Certainly this percentage of a non-scientific study will be worse in the future because a major part of the ligament inserted has only been important in the three last years (70 by year 1996 and 1048 in year 2007), and so the greater number has the lower follow up. But as the failure over the past arouse to 37 % in 4 years this evaluation set our minds to rest. Prof Giuliano Cerulli ( Perugia University, Italy ) has developed a retrospective study of his personal cases after 5 Years follow up. They were assessed by Prof. Lorentson as a blind observer. (Umea University. Sweden) in October 2007. This study ( SIOT JOURNAL October 2007 ) shows that the outcomes of the scores and the clinical evaluation by the blind observer are 95% of very good and good results. Nevertheless we haven’t had a catastrophic situation like we had in the eighties. More than 300 surgeons in Italy who used them were very satisfied. We also point out the fact that, until today, the major part of these ligaments were inserted in difficult cases like revisions, over 40 years old or multiple ligaments lesions, than in young and professional athletes. We observed honestly the principles of precaution and decided to wait 10 years follow up studies to enhance our indications. I have concentrated my paper on ACL. Regarding other applications the outcomes are very satisfying with ligaments being in full immersion in the surrounding tissues instead of being naked in the articulation. They are widely used for. knee.: - Posterior and postero lateral or medial instability 11 - Collateral medial and lateral ligament ruptures Rupture of patellar or quadricipital tendon Reconstruction of extensors muscles after knee resection for tumours Ankle: lateral and medial chronic instability Achille’s tendon rupture Hip - Instability after total prosthesis or resection for tumour Shoulder - Acromio-clavicular dislocation - Rotators cuff rupture Elbow -Chronic instability - Rupture of the biceps Wrist and hand - Scapho lunate instability, radio ulnar instability, metacarpo phalangeal instability, trapezoid metacarpal instability and arthrosis INDICATIONS : Waiting for more randomised research to be conducted before to widen the indications to all cases ( some surgeons in Austria, Italy, Greece, Venezuela and Russia already use ligaments even for high-level athletes ) the below prudent indications are for us to follow: - - - when it isn’t possible to harvest tissue on the patient ( previous pathologies or have been refused by the patient) revisions after first, second or third failed surgery, with auto or allograft PCL or knee dislocation with associated ligaments rupture ( cf Ranger Canada) Adolescents 12 to 18 and adults over 35. Women refusing scars. All the cases where a mandatory quick return to work or sport activity is required for the patient. The mentality has evolved over these past years. The use of prosthesis has accustomed people with the idea of an eventual revision surgery after some years but this requires two conditions : the second surgery mustn’t be excessively difficult and that the first operation has to give good results for some years, no pain and short time recuperation. Often with this the patient accepts the risk of an eventual revision. With these ligaments we have saved the career of a lots of athletes ( such as champion skiers in the world cup, a Canadian speed skating champion, an Austrian slalom champion, ballet-dancer star who danced again after 2 months after, a Greek class A basketball champion and several class A Italian soccer players. But this require one to be very precise and honest when speaking to the patient. You have to tell them that artificial ligaments for example can rupture in-case of a new 12 trauma like the biologic ligaments do and allow them to choose among the alternative grafts available with their advantages or disadvantages. HOW CAN WE IMPROVE THE RESULTS FOR SYNTHETIC LIGAMENTS? 1) Synthetic ligaments are less tolerant than biologic ones in case of technical errors. Often if one is honest with himself he could find the reason for failure in his technique. It is mandatory to respect the rules of their use with 6 weeks of delay before returning to sports. 2) Recent statistical studies demonstrate the results to be much better in fresh lesions operated within the first 21 days after rupture. When a good stump still present it gives also more probabilities to a good lasting result. This is certainly connected with a better fibroblastic in-growth. 3) We know that the results of the biologic grafts may be compromised by the persistence of the pivot shift. This is due to a rotational instability. We are working on the possibility to improve this case creating two new models. - a Lars ligament extended at the femoral extremity by a flat bundle is able to realise an antero-lateral plasty Lemaire type. A double reconstruction bundle with a Y ligament type Freddy FU ( Pittsburgh) or Aglietti ( Firenze). Other than the rigorous technique the same amount of rigour must be applied to the restricted indications as described above. THE FUTURE How to improve ligament repair? The actual status in ligaments repair is the use of biologics autografts, allografts or xenografts and synthetics. For biologics the ways are : - to improve the fixations systems. Over the past years several stronger fixation systems have, such as, transverse systems with pins, buttons, screws. At this moment in time it is difficult to understand what are the best. - to have a better control of rotational instability with antero-lateral plasties use a Lemaire type or a double bundle like Freddy Fu (Pittsburgh) or Aglietti (Firenze) - Improve and accelerate graft ‘ligamentisation’. by genetic engineering bringing growth factors with staminal cells For Synthetics the ways are : - a new model for ACL reconstruction has been developed. It can be used with various transverse systems, such as Transfix, Endobutton and rigid fix . We are now testing a personal new transverse system giving a rigid suspension and a strong press fit. - new models for rotational control, in cases of antero lateral instability are also being developed. 13 - In the future the navigation will certainly , thanks to a better precision of the isometric points determination, improve the rate of good results in time. Nevertheless good results are being reached with a second generation of actually use, we are improving synthetic ligaments. We are convinced that the true ‘gold standard’ could be a synthetic ligament which is able to make obsolete the harvesting of useful sane tissues from the patient or cadaver, which is able to avoid all the problems discussed above and will become everlasting. There are two considerations at the origin of the solution which we have been working on for 8 years and it seems very promising. 1) First consideration: An objective analysis shows that there is no fundamental difference for the chemist between the virtuous and angelic bio-logic ligament and the diabolic and sulphurous synthetic one. The triple collagen helix Indeed, what does happen after harvesting a BTP or an hamstring tendon? There isn’t any relevant difference that exists between organic and synthetic tissue. The first is alive until it is provided with cells and the other hasn’t any cells when it is inserted. Ligaments are composed of : - Bundles of fibrillar collagen type I, II, V which are oriented along the axis of stresses. Collagene is a glyco protein with a triple helix structure with transverse links essentials to resistance. 14 - - Structural extra cellular adhesion glyco proteins ( fibronectine, laminin, vitronectine and so on). Glycosamino glycans of extra cellular matrix and particularly the eparan sulfates. Intra and extra cellular they go through the cellular membrane of the fibroblast allowing it to fix to the matrix, it is an essential condition to have a production of oriented collagen. They are also vectors for growth factors. Fibroblasts and fibrocytes Vessels and blood cells, especially platelets, which bring growth factors and neuroreceptors. After the graft has been put on the table for preparation and all the vascular and nervous connections have been cut. What remains? A cadaver of tendon or a tendon from cadaver, as if it is an allograft. Without cells and therefore without life. It exists only collagen and glyco proteins, which are chemical components, copolymers or proteins similar to polyester chains. The collagen is no longer alive than polyester. On a molecular level there are no essential differences between tissue from a biologic origin and a synthetic one, as they are both made from the same atoms C, H, O , N , P etc… that are found in living or synthetic tissue. 15 However, a difference does exists : atoms organised in the first molecule level are recognized by the organism immune system, instead of that polyester is considered only as a foreign body, it is not aggressive therefore tolerated because it is bio-compatible. What happens when those inert substances are implanted? The autograft undergoes a progressive necrosis followed by a revascularisation, a period where it looses resistance and becomes a true collagen prosthesis ( Prof. CRISTEL) This procedure has been called by AMIEL “ligamentisation”. It presents 4 phases. - Phase I : lasts 2 or 3 weeks : avascular necrosis, the ligament is dead - Phase 2 : lasts 2 months : in this phase revascolarisation and cellular in-growth come from the Hoffa body and the majority from the ACL stump. Meanwhile the graft looses its bi-modal structure made of long fibres (100 to 125 microns) and short ones (25 to 75 microns). The length of the fibre decreases remaining a majority of short fibres. The collagen becomes mono-modal and looses it transversal links which shift between the chemical chains of the helix. This lowering of the fibres dimensions is everlasting even after 9 years follow up. (Shino) - Phase 3 : remodelling phase which lasts 12 months! In this phase the tendon is colonized again by collagen cicatricial type, with short sharpey fibres, the same that colonizes the second generation of Lars ligaments. - Phase 4 : maturation phase, in which the collagen transforms in Type I and III. It is well oriented but it will never go back to the bi-modal normal structure. The duration of this phase was under estimated it actually lasts 3 years! The above data is obtained by arthroscopical controls on humans ( Rougraf 1993 quoted from Christel). Duration of this ‘ligamentisation’ procedure is much longer than the time which has been published since now. They were based on experiments made on little animals such as rabbit, dogs and monkeys ( Amiel, Shino, Clancy ). The common resistance values were found to be after 2 years from 30 to 40% of the initial value. A TENDON WILL NEVER BECOME A LIGAMENT! The synthetic ligament : 16 It is clear that the synthetic ligaments do not suffer in the first phase, the weakening phase, and in 6 weeks there is an in-growth of fibroblastic cells which produce only definitive type of Sharpey collagen. Therefore, comparing the two ‘ligamentisation’ processes, we can see an advantage for synthetic ligaments in the first phase because of its immediate maximum resistance. In the second phase with a longer period of 10 years, the synthetic ligament would probably have to loose some resistance and therefore the biologic ligaments could have better results in this phase, but it is not sure. In fact, the readings for the duration of the ligaments on the randomised study of 5 years are similar.( Prof. DUVAL Canada). Only the future will tell if there will be a difference and a favour towards biologic ligaments. 2) The second consideration: derived from what has been said about ‘ligamentisation’. Autograft collagen, as with synthetic polyester are in reality mere scaffolds for reconstruction. If we consider Lars actual ligaments no more as an inert prosthesis fated to wear out but as for a scaffold for the biologic reconstruction, we are open to other ways, towards auto reconstruction of the ligaments. This notion of scaffold seems always to be more essential. Even using stem cells or growth factors it is necessary to have a morphologic guide of the reconstruction. It is illusory to hope that some day it will be sufficient to inject into articulation stem cells or growth factors to recreate a new ligament if there isn’t a scaffold. How can we get a reconstruction of a new ligament by the patient’s organism procedure that we call self or auto-repair. To reach this purpose we have to accelerate and improve the ‘legamentisation’ process. For the biologic scaffold: autograft, allograft or xenograft Bio-engineering research is performed two ways by many researchers. - Growth factors supply ( FGF, PGDF, TGF …) : Either directly by platelets harvested on the patient’s blood after centrifugation or by genetic engineering, transferring the gene by a modified virus carrier of which the protein expression is the selected growth factor. The problem being that this procedure is not without risks. 5 children died in France in 2003 by leukaemia lead by the virus carrier used. There is yet a lot to do before the procedure can be used clinically. - Stem cells : This way multi-potential stem cells are used. They are implanted in a tissue (nervous, cardiac, bony…) and become specialized cells producing proteins from the selected tissue. The problem is that a ligament is made of orientated collagen fibres. For the moment in time stem cells need a scaffold so collagen sponges are used for now to 17 reproduce the ligament. This scaffold hasn’t resistance before a long time. Meanwhile, what can we do to protect the reconstruction, waiting for the stem cells to finish their work? Shall we put plaster for immobilisation? Shall we have no weight bearing or long time rest before one can return to physical activity? The other problem is that the embryonic stem cells present some risks of developing tumours. They are immortals and able to reproduce themselves endlessly. The Boston group presents very variable results after 6 weeks of study ( speaking of neurological tissue) 56% of animals improved, 24% had no result but the most serious problem was that 20% developed growing tumours and died. So these promising techniques are not ready at the moment to be used without risking the problem of scaffold weakness until the new ligament is built again. They probably will be expensive procedures and not easy to be used in all hospitals but only in a few specialised medical centres. The use in ligament reconstruction with the necessity of harvest in the first steps, stem cells, wait for their development in cultures before doing the operation this seems a very heavy procedure. For the above reasons, I believe that my procedure using new synthetic material, called bio-mimetic or bio-active copolymers, has at the moment advantages : nothing to harvest, full safety, immediate resistance with return to sport within 2 months and nothing to change in the insertion procedure. The material can be used with the same actual technique used for the existing Lars in any hospital without the aid of a biologist. Concerning allografts, besides the fact that the times and the quality of the colonization by the collagen are very long and accompanied by often progressive lengthening, the risk of disease transmission, even if low, still exists. 4 people died in the U.S.A. by clostridium and 4 aids transmission ( Freddy FU ). I retain it is unacceptable to restore a ligament, to risk taking a patient’s life. I repeat, with synthetic ligaments there is no risk at all of disease transmission with the exception of the case of per-operative asepsis fault. For the synthetic scaffold, we can improve them with : - Use of new fibres in a way in which we have a more resistant and lasting ligament As I know studies have been performed with : Carbon nanotubes, which are very resistant and elastic, but it is difficult to get fibres long enough and the biocompatibility is very hazardous. - Spider silk seemed very promising as it has five times the steel resistance for the same diameter but we have no study on wear resistance and biocompatibility. For three years we have never heard again anything about this research. A study is performed in USA with worm silk.There are no clinical studies at this time. .- Synthetic collagen, with the disadvantage that we have to wait for a potential ‘ligamentisation’, before allowing a return to sport activity. 18 CREATING THE BIO-MIMETIC OR BIO-ACTIVE BIO-MATERIALS Bio-active materials are the objective of our research group for 7 years and is near completion. In 2006, began an animal study after the Laboratory of macromolecules, (PARIS XIII Universtity of France) (Prof. Veronique MIGONNEY ) achieved the invitro study. As we have seen, the difference between the polyester used as a scaffold and collagen resides only in the fact that, if both are colonized again by fibrotic cicatricial tissue with poor resistance, the collagen, in the late phase is remodelled in efficient collagen, phase I and III. Instead, with the actual Lars ligament the collagen type stays unchanged. This difference is due to the fact that an alien body introduced in the organism , cause by the immune system, sends a chemical message which is received and returned with three types of possible response. - the first case is an aggressive response: the organism rejects the foreign body: it is the case of synthetic ligaments from the eighties, poorly” disensitizited” , alien proteins or tissues etc…. - the second case: receives no response therefore consider neutral, it not rejects it but wraps it into fibroblastic tissue of Sharpey fibres collagen. It is the case of the Lars second generation ligament that we use today, mammary prosthesis, artificial crystalline lens and surgical cement for prosthesis. - The third possible response is when the immune system recognises the molecule inserted and consider it as being a part of the organism. In this case there is no rejection or intolerance but a true biologic integration. The fibroblast cells fix onto the extra cellular matrix, from spherical become spindle-shaped, which is an essential condition to make them activated and secrete collagen I and III. How does the recognition of the polyester by the immune system work? The basic idea of polyester recognition was discovered in the Macromolecules and Speciality copolymers Center from PARIS XIII University under the direction of Prof. Veronique MIGONNEY and her team. The recognition of bio-materials is due to the presence of some chemical groups in the molecule. Allowing the cells to be fixed into the extra cellular matrix through its membrane integrine. The heparan sulphates passing through the cell membrane are examples of this. They are proteoglicans, the sugar part of them remains out the cellular membrane and the protein part travels through the membrane. By the means of linking not only ionic but also stereo chemical called key/lock system these chemists were able to fix onto various copolymers (polystyrene, polyethylene, Dacron etc… ) ionic groups i.e. sulphonate and carboxyle, which mimetise the biologic radicals responsible of the researched fonction. 19 They have, in one way created a new type of bio-materials called bio-mimetics and bioactive, which, mislead the immune system into recognizing them. For instance, a modified polyethylene tube used for heart surgery called heparin like whose inner surface becomes non-coagulable. In this case, the bio-mimetic radicals fixed onto the polyethylene induce the fixation of them onto the blood prothrombine as if it would be a real heparin. Instead of trying to synthesise the whole protein (heparin) it is sufficient to place on a scaffold (here the polyethylene) the active radicals giving them anticoagulation function. They are also able to realise an AND like polystyrene to fix the bacterial toxins etc. Bioactive polyethylene like Bioactive polyester ADN like ( My contribution was to ask to the Prof. Migonney team (I read, they won the South Carolina University Clemson award for their discoveries) if it was possible to extrapolate these results to polyester. After 8 years of various attempts they found polystyrene sodium sulphate ( poly NA SS) can be fixed on to the whole surface of polyester fibres, the fibroblasts recognize it like an heparansulphate and cause their adhesion in a linear and strong manner.(Adhesion force is (8.5 dynes/cm2 for the non grafted with poly NASS ligaments versus 15 dynes / cm2 for the grafted one.) Their shape become from sphere to spindle-shape and the effective production at the third day of type I and III collagen was controlled. ( The collagene secretion by cells is double for the grafted ligaments than for the non grafted.) The cells remains alive and it was also checked the absence of toxicity or allergic reaction to the modified polyester. ( Studies on rats by BIOMATECH) The examination with the scanning electron microscope shows a perfect distribution of the cells on all of the microscopic polyester fibres surface which is better and more 20 regular than those found with the actual Lars fibers . Their strong adhesion to the polyester matrix was tested . Their spindle shape has a dimension from 50 to 80 μm. Bioactive copolymer molecule. Red arrows mark active radicals fixed on polyester 21 Scanning electron microscope. View of the actually used ligament. Anarchic distribution of spherical fibroblasts and poor resistance to rotation stresses. New ligament. Perfect distribution of fibroblast on the whole polyester fibres surface. 22 ANIMAL PHASE RESEARCH In January 2006, 16 sheep had an implantation after section or resection of the ACL, some with a second generation Lars ligament already in use for thirteen years, others with the new bio-mimetic ligament. The clinical result was perfect with no postoperative or functional problems. They have been sacrificed at 6 months and the first histological results were very promising. RX of sheep knee Non modified ligament. Giant cells (white arrows) Modified ligament. Dense fibroblastic tissue. (white arrows) Blood vessels (red arrows) Absence of giant cells. We are going to continue with the animal study and we hope to begin very soon in the hospital of Prof. Giuliano CERULLI of Perugia University phase 1 and 2 of the human study on randomised prospective series. The revision of the clinical results will be performed by Prof . Ronnie Lorentson of the Umea University (Sweden) as a blind observer at the Nicolas foundation in Arezzo (Italy) and ruled by Prof. Cerulli and myself under the Ethic Comity control. We hope that by the end of these studies we will be able to offer bio-mimetic and bioactive ligaments to orthopaedic surgeons and that they become one of the ‘gold standards’ in ligament reconstruction. This is because, having eliminated the only disadvantage of actual synthetic ligaments which is the incertitude of its duration (even if we have 13 years follow up), this product will be able to induce the auto reconstruction of a new ligament, without the necessity of bringing stem cells or growth factors, still 23 maintaining the immediate resistance of the polyester, allowing a very early return to physical activities ( 6 to 8 weeks,) and without any damage for the patient because nothing is harvested.