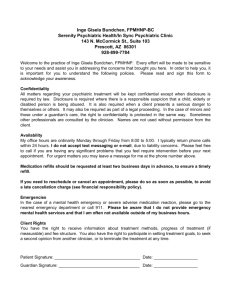
Key Point Health Services
advertisement

Key Point Health Services, Inc. Policy and Procedure Manual Revised May, 2006 Karl Weber, CEO Last saved by joycefitch2/12/2016 TABLE OF CONTENTS Introduction Overview Mission Goals & Objectives Program Goals & Objectives Adults Child & Adolescent Program Sites and Hours Population Serviced Range of Services Non-discrimination Policy Personnel Organizational Chart Intake Application For Services Intake Call Screening Intake Call Screening Form Intake Log (Sample) Client Checklist Screening Schedule (Sample) Screening Appointment Demographic Information Form Emergency Contact Form Medical Screening Form HIPAA Privacy Practices Form Termination of Services Policy Treatment Policies & Procedures Receipt of all information received (form) Financial Agreement Form Consent for Treatment of a Minor (form) Developmental and Medical History (form) Emergency Contact Form – Minor Medical Screening & Physical Exam Result Completing a Face-to-Face Assessment Screening Admission Applicants in Crisis or Danger Initial Contact Admission Criteria Adult Child & Adolescent Informal Kinship Care Affidavit Instructions 2 Informal Kinship Care Affidavit Form Patient Record Emergency Contact Emergency Contact Form – Adult Emergency Contact Form – Minor Demographic Information Demographic Information Form Admission Note Admission Note – Adult (5 page form) Child & Adolescent Admission Note (4 page form) Establishing Fees Financial Policy Financial Information and Information Update Form Encounter Forms Blank Encounter Form (sample) Patient Rights and Responsibilities Termination of Services Informed Consent Grievance Policy Grievance Form Psychiatry Psychiatric Consultation Physical Examination Laboratory Reports Psychiatric Consultation Sheet (for page form) Psychiatric Appt/Medication Status for Residential Patients Psych. Appt/Med. Status Form Fax Cover Sheet/receipt of above forms (sample) Medication Sheet Psychiatric Transfer (Controlled Substances) Prescription Pads Medical Waste Guidelines for disposal Course of Treatment Treatment Planning Individual Treatment Plan (form) Treatment Plan Review (form) Tracking Treatment Progress Patient Attendance Sheet (form) Progress Note (form) Continuing Evaluation and Treatment Signature Sheet Patient Transfer Case Transfer Form Universal Transfer Policy Patient Compliance 3 Referrals Group Therapy Reporting Requirements Abuse of a Child Child Neglect Adults Abused as Children Subpoena (sample) Report of Suspected Child Abuse/Neglect (form) Report of Suspected Child Abuse (AMAC form) (Adults Molested as Children) Duty to Warn Emergency Petition Emergency Privileges Authorization Form New Emergency Evaluation Law Petition for Emergency Evaluation (form) Incident Report Significant Event Report (form) Death Report Death Report Fax Cover Sheet (form) Death Report – DHMH Form 4364 (3 pages) Discharge Prior to Discharge from Clinic Discharge Summary Form School Based Program Application for Services Key Point Referral Form Application for School Based Program Admission Process Applicants in Crisis r Danger Patient Compliance Psychiatric and Diagnostic Evaluation Employee Safety Cell Phone Policy Cell Phone Access Program Cell Phone Reimbursement Procedure Check Requisition (sample) Quality Improvement Performance Improvement Plan Program Improvement Plan Mechanism for Implementation Continuous Quality Management Security and Confidentiality of Records Performance Improvement Indicators Record Review Chart Audit Record Review Form 4 Credentialing and Privileging Employee Supervision Supervisor/Supervisee Documentation Child and Adolescent Weekly Service Report (form) Application for Clinical Privileges Continuing Education and Required Training Students and Volunteers Policy Fire Safety Arming and Disarming Alarm System Evacuation Routes Fire Inspection Reports (copy of last report) Bomb Threats Patient and Staff Safety Anthrax Policy Violence – Policy and Procedure Waiver Addendum Program Service Annual Report 5 INTRODUCTION 6 This manual has been prepared (in compliance with State Mental Hygiene Administration regulations) to assist staff, interns, and volunteers with the policies and procedures of providing, documenting and evaluating quality patient care at the Dundalk Clinic. 7 INTRODUCTION OVERVIEW The Key Point Health Services, Inc. (Dundalk) is one of three mental health centers administered by Key Point Health Services, Inc. We are located in southeast Baltimore County (21222). PURPOSE The purpose of the center is to coordinate or directly administer a wide range of mental health services without regard to race, sex, creed, religion, or sexual orientation, to residents of Dundalk. These services are physically, psychologically, and economically accessible to the local population, with priority given to the following high risk populations: De-institutionalized and incapacitated adults and children Those recently discharge from community hospitals Those in out-of-home placement or at risk of such These services are provided in the least restrictive manner appropriate to the individual’s level of functioning. Services delivered shall be monitored in such a manner as to insure quality, efficiency, and effectiveness of treatment. Every effort shall be made to coordinate resources in the community at large, to reduce duplication of services, to increase utilization of specialized services, and to assist other agencies in developing programs needed in this area. 8 MISSION The mission of Key Point Health Services is to provide quality mental health care in an environment committed to continuous improvement. 9 GOALS AND OBJECTIVES The goal of treatment is to improve social, work and/or school functioning, reduced symptoms, increase autonomy, and prevent hospitalization. The objective is for all patients to be engaged in some meaningful daytime activity and to live as independently as possible. Because the majority of the patients admitted to the clinic are treatment refractory, the objective is not for symptoms amelioration but for symptom reduction and for patients to gain improved coping strategies for managing their symptoms and remain in the community reaching their full potential. 10 PROGRAM GOALS AND OBJECTIVES (10.21.17.05.A.05) ADULT SERVICES The Adult Services components of Key Point at Dundalk provides outpatient services to adult patients, 18 years of age and older. Services include individual, group and family therapy; psychiatric evaluation, and medication management. Referrals to inpatient units are made when appropriate. The patient is involved in all aspects of his or her treatment. Adult services employs a multidisciplinary team composed of psychiatrist, a nurse, social workers, and professional counselors, as well as interns. A. To provide comprehensive mental health services to the priority population in the Dundalk area. To individuals in the public mental health system which consist of the uninsured (see eligibility criteria attachment), Medicaid and dual eligible. 1. Staff will screen applicants to determine if they meet the admission criteria. 2. Following an initial assessment, referrals will be made to cover any presenting problems that cannot be addressed through services offered at the clinic. B. To continue to provide well coordinated treatment for clients services by various programs within Key Point. 1. Representatives from each of the local Key Point components will meet on a monthly basis to coordinate treatment of mutual and plan for improvements in coordination of services. 2. All patients will be assessed for possible referral to Case Management services. The case manager may assist a client in securing entitlement, transportation, housing, or outside supports. The case manager will be invited to participate in interdisciplinary treatment planning. 3. Any patient who admits or is suspected of substance use will be encouraged and possibly required to participate in substance abuse treatment in conjunction with their mental health treatment. The clinician will work with the patient to coordinate dual diagnosis treatment. A clinician may determine that providing mental health services would be contraindicated, if a patient refuses concurrent substance abuse treatment. Patients would be encouraged to resume mental health services when they are ready to engage in substance abuse treatment as well as mental health treatment. 11 CHILD AND ADOLESCENT These teams provide psychiatric treatment for children (up to age 18) and their families. (Services include individual, play, group and family therapies; psychiatric and medication evaluations; and consultation with schools. Additional services include collaboration with DSS and other community agencies involved with the child.) Referrals to other outpatient and inpatient programs for children and adolescents are made when appropriate. Parents are actively involved in all aspects of the services available. In addition, services are provided in local schools through our School Based Program. In this program therapists are based in the school or other community based facilities. The therapist maintains a close working alliance with the teachers, guidance counselors and other relevant staff in the school. The program works closely with parents/guardians since they become part of the local community. NEEDS The mental health psychiatric needs of children have been the subject of study by both the State Mental Health Administration and Baltimore County. In order to develop a balanced service system with an emphasis on early intervention, MHA guidelines gave priority to the needs of the following populations: Those children and adolescents being discharged from state-operated inpatient psychiatric hospitals or residential treatment centers (TRCs) and those children and adolescents being discharged from state-funded placements in private psychiatric hospitals or residential treatment centers. Children and adolescents and their families where the child has an emotional, behavioral or mental disturbance and where the child is in an out-of-home placement, particularly those who are moving from placement to placement or are at-risk of moving to a more restrictive placement (e.g. children in foster care, detention, court-committed facilities, or temporary shelter). Children, adolescents and their families where the child is experiencing the effects of an emotional, behavioral or mental disorder, and may be at-risk of being placed out-of-home (e.g. abused and neglected children, children in special education, runaway, truant children needing outpatient care to preserve intact homes or those with suicidal tendencies). Children, adolescents and their families where the child is at-risk of developing an emotional disorder (e.g. those in shelters for homeless families, children with substance abusing or mentally ill parents). The School Based Program focuses on children who are in need of mental health services but who have historically not engaged in traditional outpatient mental health services. 12 GOALS I. II. III. IV. V. VI. VII. VIII. Provide early identification, diagnosis and treatment of emotional and psychosocial problems which impair full functioning at the child’s/adolescent/s developmental level, or which would lead to significant impairment and possible removal from the home setting if undiagnosed and untreated. Children and adolescent will receive an initial face to face assessment within 5 working days if released from psychiatric facility, 10 working days if not. Maintain staff responsibility for specific school populations, which includes: A. Initiating and developing liaison with key school staff B. Orienting school staff to service, method of referral, availability for case consultation, and the goal of early identification, C. Response to Intake calls for treatment from designated school populations. Enhance and expand diagnostic evaluation and treatment services. A. Insure comprehensive evaluation, via referral for appropriate diagnostic examinations/tests (for example, EEG). B. Increase the use of referral for specialized treatment services. C. Refer child and adolescent substance abusers or those whose parents or guardians have substance abuse problems to local resources which provide specialized services for this population. D. Develop specialized group to meet the needs of identified high risk populations. Insure maximum continuity of treatment from intake to discharge or referral to another agency. Continue to hold and to document monthly clinical staff conferences of the child and adolescent team for review/consultation/supervision of intakes, admissions, case problems/progress, treatment planning and review, and discharge planning, as well as administrative/training issues. Continue the referral of appropriate patients to the child psychiatrist for psychiatric evaluation, medical/history screen review, medication evaluation, prescribing, monitoring, and crisisevaluation, if a patient is at risk of harming self or others, referral to inpatient setting. Facilitate ongoing coordination with hospitals or other residential placement schools/agencies for collaboration in aftercare planning for outpatient treatment. Refer to case management or other support services when necessary. A. Provide for emergency and crisis interventions. B. Inform parent of specific resources for after-hours. 13 IX. X. C. Update an organized list of specialized crisis resources for problems of child abuse, rape, runaway, and suicide attempts. Continue collaboration with schools and ARD Team. Conferences when a more restrictive placement of patient is under consideration. A. Recommend alternatives to residential (Level IV) placement decision if necessary and appropriate. B. Participate in deliberations about Level V, day school placement; determine whether therapy is to be provided at that school. C. Provide aftercare services to patient and family. Consult with selected agency representatives for clarification concerning referral process, resolution of occasional problems and sharing of information. Continue direct and/or indirect communication between Child and Adolescent staff and community agencies – DSS (Protective Services, Foster Care, etc.), DJS (Community Arbitration, Police Department), Health Clinics, School System, and other Mental Health Agencies and Hospitals. 14 PROGRAM SITES AND HOURS (10.21017.05.A.04) The Key Point Mental Health Clinic at Southeastern is located at 7702 Dunmanway, in Dundalk. We are directly across from the local office of the Department of Social Services, as well as Community Assistance Network office. The clinic is open Monday through Friday 8:30 a.m. to 5:00 p.m. as well as, at least two evenings per week. The clinic phone number is 410-282-1792. Key Point Health Services, Inc. provides for after-hours and weekend emergency coverage through an emergency number that is given to all patients and printed on all appointment slips. The number is 1-877-5397646. The School Based Program has contractual agreements with selected schools throughout Baltimore County. Services are offered in these sites during regular school hours as well as extended hours when the school may be open and the need warrants such. RANGE OF SERVICES Staff may attend treatment planning and collaboration meetings with other providers, schools, and other community agencies when the family has consented for such and it is determined to be clinically indicated. 15 POPULATION SERVICED (10.21.17.05.A.02) Key Point Health Services at Dundalk serves individuals with an AXIS I DMS-IV diagnosis, with special emphasis on patients with chronic and persistent mental illness, as well as those without access to health insurance. Our current population includes children ages 4-18 (28%), adults ages 1860 (63%) and older adults age 60 and above (9%). The population served is 42% male and 58% female. One percent of the population is Asian, 13% African American, 82% White and 4% other. Key Point at Dundalk specializes in the treatment of seriously and persistently mentally ill (SPMI) adults; and children with, or at risk for, the total population services is 20% Schizophrenia and other psychotic disorders; 40% Affective disorders; 10% Anxiety disorders; 12% Adjustment disorders; and 18% all other disorders. Approximately 40% of the adult population has co-occurring substance abuse problems. Poverty and other social problems, as well as somatic illnesses complicate the clinical picture of many of the patients. 16 RANGE OF SERVICES (10.21.17.05.A.01) Our services begin with a thorough needs assessment for each patient. In addition to the diagnosis and treatment of an individual’s mental illness, we also do a holistic assessment of all factors that might be affecting their mental health. We then assist patients, either directly or through referrals, to resolve these problems. We coordinate services with patients’ other health providers and various social services agencies. To address the mental health needs of our patients we provide psychiatric evaluations, medication management, crisis intervention, and individual, group and family therapy. (See also policy memo on Non-Discrimination.) 17 KEY POINT HEALTH SERVICES, INC. TO: ALL STAFF FROM: CLINICAL DIRECTOR RE: NON-DISCRIMINATORY POLICY DATE: JUNE 26, 2006 PLEASE CONSIDER THIS MEMO AS AN ANNUAL, OFFICIAL STATEMENT THAT THIS CENTER IS READY TO MEET THE MENTAL HEALTH NEEDS OF ALL CITIZENS, REGARDLESS OF RACE, AGE, SEX, DISABILITY, RELIGION, NATIONAL ORIGIN, OR POLITICAL AFFILIATION, WHO LIVE IN SOUTHEASTERN BALTIMORE COUNTY. 18 KEY POINT HEALTH SERVICES, INC. DUNDALK CLINIC 7702 Dunmanway Baltimore, MD 21222 MEMO TO: All Staff FROM: Tessa Worsham, Director DATE: June 23, 2005 RE: Non-Discriminatory Policy Please consider this memo as an annual, official statement that this center is ready to meet the mental health needs of all citizens, regardless of race, age, sex, disability, religion, national origin, or political affiliation, who live in Southeastern Baltimore County. 19 PERSONNEL (12.21.17.05.A.06) 20 Insert SAMPLE Organizational Chart *As of 02/27/02 21 INTAKE 22 APPLICATION FOR SERVICES If an individual meets the criteria for admission, and Intake Call Screening Form is completed. If the individual to be admitted has been a patient at this facility in the past, the old medical record (if available) is pulled and consolidated with the new one. The information documented over the phone for the initial screening is demographic information, such as name, address, age, date of birth, contact number, social security number and the kind of insurance. Additional information requested is suicidal or homicidal ideation, any substance abuse history, if there are any legal issues, court orders or probation. The date of the screening is given and then documented on this form and they are told to bring in their personal information, such as social security card, primary doctor’s name and address, proof of custody (for anyone under 18), insurance cards, proof of address and immunizations records (for anyone under 18). The intake worker then records the individual’s name on the screening schedule form. When the individual comes in for their screening, their information is collected, copied and returned. They fill out their paperwork and return it to the front desk when completed. The intake worker puts the chart together, notifies the screener and the face to face assessment is then completed and the appointment is given to the individual. All patients are assigned to the first available clinician unless the individual makes another request, such as a clinician he or she worked with in the past, or a female therapist; or if there is another clinician with particular experience with the presenting problem, such as EMDR and trauma survivors. In addition to recording the intake on the intake schedule, the intake worker also makes an entry in the “intake log”. The following information is to be recorded: 1. 2. 3. 4. 5. 6. 7. Date of the intake Patient’s name Social Security Number Therapist Code – adult or child Referred by School (children only) After this is completed, the intake worker gives a copy to the assigned therapist and the original stays on the chart. If the patient shows, the original is then put into the chart. COMPLETING AN INTAKE CALL SCREENING FORM If an individual meets the criteria for admission, an “Intake Call Screening Form” is completed. This can be done over the phone or in person. This form must be completed before a screening appointment can be scheduled. Some points of explanation follow. CALLER AND RELATIONSHIP: We strongly prefer that if the patient is an adult, he or she make the initial appointment for him or herself. If the person is hospitalized we will accept a call from a hospital discharge worker. If the potential patient is absolutely unable to 23 make the call, we will accept and application if we have assurance that 1.) the person is aware that the appointment is being made and 2.) that the potential patient is committed to keeping the appointment. CALLER’S PHONE: Make note of the referral source’s phone number. NOTE: At intake, the clinician should obtain the patient’s permission to follow up with the referral source. DATE: The date the Intake Call Screening Form was taken. CLIENT’S NAME: Write clearly, making sure the spelling correct. CLIENT’S PHONE: If the person does not have a phone, get a number where a message can be left. And note how the patient would like us to leave the message, i.e., with or without saying “Key Point”. INSURANCE INFORMATION: Make sure this is accurate. Determine if patient has MA, MC, or is uninsured. Get a policy number for each type of insurance. Read the number back to the caller for confirmation. PRESENTING PROBLEM: Applicant’s reason for requesting services. Obtain a general idea of the applicant’s current life situation, status of problems, and what it is he/she would like to change. Ascertain how long the problem has existed, and what he/she has been doing regarding the problem so far. PRIOR MENTAL HEALTH TREATMENT: Include names and dates of psychiatric hospitalizations or previous outpatient providers. What was the presenting problem then? Outcomes of previous treatment? Has the Applicant been a patient of Key Point Community Mental Health Center in the past? If so, who was previous clinician? MEDICATIONS: Obtain a list of current medications, the dosage and the amount remaining, if appropriate. Obtain the name of the prescribing physician and the reason for taking the medication. SUBSTANCE ABUSE HISTORY: Does the patient drink alcohol? How much and how often? Does the person use street drugs? What, how much and how often? Has the person every been in substance abuse treatment? Does the applicant think he or she has a problem with drugs and/or alcohol? LEGAL ISSUES/COURT ORDERED/PROBATION: Are there any current legal mattress? Pending court dates? Is the applicant court ordered? If so, they MUST PRESENT A COPY OF THE COURT ORDER before the appointment is scheduled. SUICIDAL/HOMICIDAL: Ascertain if any of these conditions exist. If so, intake clinicians MUST intervene at the point. (Have you thought of harming yourself or someone else?) 24 PARANOID IDEASTION/HALLUCINATIONS: Do you see or hear things that others do not? Do you feel as if people are following you, watching you? Do you think someone is trying to hurt your? TARGET/PRIORITY POPULATION: Target or Priority Population is those with a history of multiple and/or recent hospitalizations for the major DSM disorders. Also, a person meets the priority population criteria if he or she is having difficulty functioning on his or her own. INFORMATION CLIENT SHOULD BRING TO INTAKE: Proof of income Social Security Card Insurance Card(s) Proof of address Primary M.D.’s name, address, phone number For Child/Adolescents: (in addition to above information) Proof of custody, e.g. court order, birth certificate, custody agreement. ADVICE TO CLIENT: If condition worsens, call us or go to emergency room. ASSIGNED TO: The next available appointment, taking into consideration the “fit” between patient and therapist. Except under extreme circumstances, this clinician will also be the patient’s primary clinician. INTAKE WORKER: The clinician or clerk taking the information, making the screening, and assigning the applicant to an appointment should sign his/her name. 25 Insert Intake Call Screening Form (needs to be updated) 26 Insert Informal Kinship Care Affidavit Last updated 03/30/06 27 NUMBER OF DAYS BETWEEN CALL AND FIRST APPOINTMENT: Record number of business days. Notify the intake coordinator if patients are not able to see a clinician within 10 days. NOTE: If the individual is admitted to the program, this completed Application for Services is retained and becomes part of the patient’s medical record. If the individual is not accepted into the program, the following information is gathered and maintained: Identifying information The source of referral The reason the individual was not accepted Description of referral, if any, to alternate service providers INTAKE CALL SCREENING The intake clerk will review the eligibility criteria and the intake procedures with the potential client. Callers who do not meet the eligibility criteria will be given appropriate referrals. The clerk will also identify the supporting materials that the potential client will need to have in order to become a client (See “Client Checklist”). If the potential client has insurance they will need to show their card. If the potential client has no insurance, the clinic will follow the procedure outlines by the Administrative Services Organization (ASO) (See attached APS Medical Necessity Criteria for the uninsured). Those individuals who are seeking care in emergency situations will be assessed regardless of documentation or ability to pay. COMPLETING INTAKE CALL SCREENING FORM When potential client calls the clinic to schedule his/her screening appointment, the intake clerk with gather information: (see Intake Call Screening Form) Date of call Callers name, address, phone number, date of birth, and social security number Insurance information, including all types of insurance and insurance numbers If potential client has no insurance, clerical staff will verify that the individual meets the eligibility criteria to access medically necessary mental health treatment services for the uninsured (as stated above) Any history of substance abuse Any legal issues/court order/probation Current suicidal or homicidal ideation (clerk will contact backup clinician if SI or HI is present) Once all the information is given, the intake clerk will give potential client a list of materials that he/she will need to bring to the screening appointment. Those items are as follows: Social Security Card Insurance Card(s) Proof of Address Primary physician’s name, address, and phone number. If potential patient is a minor, the parent/guardian will also be required to provide: 28 Proof of custody (i.e. birth certificate, birth record, court order, or custody papers) Immunization record Individuals who are deemed appropriate for services will be scheduled for a face-to-face assessment screening within 10 business days and those being discharged from a psychiatric hospitalization will be scheduled within 5 business days. Potential patients will be seen for initial psychosocial assessment within 30 days. Once a patient has called, or walked into the clinic, and completed the Intake Call Screening Form, he/she is offered the next available date/time for screening appointment. Screening appointments are offered multiple days per week. (See sample Screening Schedule) SCREENING APPOINTMENT When the potential client attends the screening appointment, the intake clerk will make a copy of all the information the client was asked to bring (see above list). Before individuals meet with a clinician for a Face-to-Face Assessment Screening, they must first complete the following paperwork: Demographic Information Sheet Emergency Contact Form Medical Screening Form o Patient is given a copy of the following: HIPAA Privacy Practices Form (signs receipt of form) Termination of Services Policy Patient’s Rights Non-Payment Policy Treatment Policies & Procedures Form (signs receipt of form) Financial Agreement For Child/Adolescent patient (in addition to the above): Consent for Treatment of a Minor Developmental and Medical History Emergency Contact Form – minor MEDICAL SCREENING & PHYSCIAL EXAM RESULTS Since a patient’s somatic health could be a factor in their mental health, it is Key Point policy to attempt to obtain information on the patient’s physical health. At the initial visit, adult patient are asked to complete a “Medical Screening Form”, while parents of patients under 18 are asked to complete a “Developmental and Medical History”. In cases where an emancipated child is seeking treatment independently they will complete the “Developmental and Medical Form”. (see Medical Screening Form) (see also Developmental and Medical Form) 29 PROCEDURE It is responsibility of the primary therapist, at the time of admission, to: Verify that a “Medical Screening Form” or “Developmental and Medical History” has been completed by the patient or his/her guardian. The therapist will initial the form indicating that they have reviewed it for completeness and sought clarification or medical support as needed. Request that the patient (or guardian) submit a recent physical examination report or sign “Consent for Release of Physical Examination Report”. The non-medical mental health professional, in signing the “Medical Screening Form; or “Developmental and Medical History” form is not responsible for the assessment of the medical problems; their initials indicate that the process for obtaining the data was followed. It is the responsibility of the psychiatrist to review the medical screening form for information that may effect the psychiatric treatment of the patient. They indicate that they have done this in the appropriate section of Psychiatry Consultation Form. If the patient elects not to see a psychiatrist they will be urged to review any medical issues with their medical doctor. The adult patient or guardian can complete this form alone; if a patient is unable to do this, an adult accompanying the patient may be able to provide the information. The parent of a patient under the age of 18 completes the Development Medical Form for the patient. The patient (or designated provider of information) signs and dates the form. A release of confidential information should be completed by the clinician and signed by the patient on the first visit when an identified medical doctor has treated the patient within the past year. This release specifies that we are requesting the results of a physical examination not more than one year old. 30 Insert Medical Screening Form Last updated 07/2006 31 Insert Child and Adolescent Developmental and Medical History Last updated 07/2006 32 COMPLETING A FACE-TO-FACE ASSESSMENT SCREENING Once an individual completes the paperwork outlined above and gives the documents to the intake worker to file in chart, the screener will meet with them for a brief face-to-face assessment screening. Through this assessment, the screener will determine if 1.) the individual meets the clinical criteria for admission and/or 2.) has a safety risk that needs to be addressed before beginning outpatient treatment. The screener will decide whether to have an authorized staff member do an immediate evaluation for an emergency petition, refer to another facility that is more suitable for the individual’s presenting problem, or give the individual the next available appointment with a therapist at this location. An Intake Screening Form is used to document information gathered during this assessment. (See Intake Screening Form) 33 Insert Monthly Intake Log 34 Insert Intake Schedule (sample) 35 Insert Patient Checklist Last Updated 11/21/05 36 Insert Screening Schedule 37 Insert Screening Packet (child and adult forms) 38 ADMISSION 39 ADMISSON PROCEDURES The Key Point Outpatient Mental Health Clinic at Dundalk provides mental health services on a non-discriminatory basis primarily to individuals in the Dundalk area with serious and persistent mental illnesses. (See also policy on Non-Discrimination). Key Point accepts individuals 4 years of age through adulthood. Persons having legal guardianship of a child or an adult may refer, apply and/or consent to treatment for those in their care. If the child is in foster are, we may accept a referral of the child from a foster care worker, foster parent, or legal guardian. Legally required documentation is necessary from whoever makes the application or brings the child to the initial intake, in order to prove they have the legal right to make such arrangements. For children under age 16, a primary caregiver (i.e. custodial parent, foster parent) must bring the child to the screening and psychosocial assessment. Children 16 years or older may seek services without parental permission. Upon admission, every patient will receive Key Point’s Patient Orientation Package which includes items such as Patient Rights, HIPAA, Therapy Participation, Non-payment and Grievance policies among others. Child and Adolescent Therapy Participation requirements sheet is read and filled out by a parent or guardian. These forms mention the need to keep regular therapy appointments and the responsibility to call if a patient misses an appointment. Next, the demographic form is to be partially completed by patient/parent. The remainder of this form is to be filled out by the therapist. This gives pertinent personal data. Next, the emergency contact form is filled out and signed. The medical screening form is to be completed by answering yes or no to the physical questions and then signed and dated. The treatment policies and procedures are to be read and signed. Patients/family member for a child initial that they received a copy of the non-payment policy, patient rights, and termination of services policy. The patient/family member of a child read and signs the nonpayment policy applying to all Key Point patients. Patients are encouraged to pay their fee at the time of services. APPLICANT IN CRISIS OR DANGER Key Point is committed to providing mental health services to the community in a responsive and accessible manner. In the event of an emergency situation involving an applicant for services, we will make every reasonable effort to ensure the individual’s safety. If a potentially dangerous or suicidal individual walks into the clinic, he or she will be assisted by the first available clinician, who will be notified of the emergency by the receptionist or the intake clerk. The clinician will do an emergency evaluation of the situation and determine the appropriate course of action. The clinician will attempt to stabilize the individual (see also policy on violence) and will either obtain a contract for safety and schedule a screening appointment; or the clinician may determine that the individual needs immediate attention and may call 911 and/or crisis team or have an emergency petition completed by an authorized staff member. 40 If an individual calls the clinic and indicates that he or she is contemplating suicide or homicide, the receptionist will immediately summon the first available clinician. If the receptionist is unable to summon additional help (while keeping the caller on the phone), he/she will attempt to obtain the caller’s phone number. If we are unable to ascertain the name or the phone number of the caller, we will not be able to send help. If the clinician is able to reach the caller, the clinician will assess the situation and call 911 as necessary. INITIAL CONTACT Individuals seeking mental health services may walk into the clinic or inquire by phone. Potential clients (1) will receive prompt and courteous replies to their inquires, (2) will be screened for appropriateness and urgency, and (3) immediate action will be taken in the event of a crisis situation. If the intake clerk (or his/her designated substitute) is unavailable, potential clients can expect a return call within 2 business days. If the call is from an inpatient discharge worker, the call will be returned by the end of he day. Emergency walkins and emergency calls will be handled by the first available clinician. INTAKE CALL SCREENING The intake clerk will review the eligibility criteria and the intake procedure with the potential client. Callers who do not meet the eligibility criteria will be given appropriate referrals. The clerk will also identify the supporting materials that the potential client will need to have in order to become a client (See “Client Checklist”). If the potential client has insurance they will need to show their card. If the potential client has no insurance, the clinic will follow the procedure outlined by the Administrative Services Organization (ASO) (See attached APS Medical Necessity Criteria for the uninsured). Those individuals who are seeking care in emergency situations will be assessed regardless of documentation or ability to pay. COMPLETING INTAKE CALL SCREENIGN FORM When potential client calls the clinic to schedule his/her screening appointment, the intake clerk will gather information: (see Intake Call Screening Form) Date of call Callers name, address, phone number, date of birth, and social security number Insurance information, including all types of insurance and insurance numbers If potential client has no insurance, clerical staff will verify that the individual meets the eligibility criteria to access medically necessary mental health treatment services for the uninsured (as stated above) Any history of substance abuse Any legal issues/court order/probation Current suicidal or homicidal ideation (clerk will contact backup clinician if SI or HI is present) Once all the information is given, the intake clerk will give potential client a list of materials that he/she will need to bring to the screening appointment. Those items are as follows: Social Security Card 41 Insurance Card(s) Proof of Address Primary physician’s name, address, and phone number. If potential patient is minor, the parent/guardian will also be required to provide: Proof of custody (i.e. birth certificate, birth record, court order, or custody papers) Immunization record Individuals who are deemed appropriate for services will be scheduled for a face-to-face assessment screening within 10 business days and those being discharged from a psychiatric hospitalization will be scheduled within 5 business days. Potential patients will be seen for initial psychosocial assessment within 30 days. Once a patient has called, or walked into the clinic, and completed the Intake Call Screening Form, he/she is offered the next available date/time for screening appointment. Screening appointments are offered multiple days per week. (See sample Screening Schedule) SCREENING APPOINTMENT When the potential client attends the screening appointment, the intake clerk will make a copy of all the information the client was asked to bring (see above list). Before individuals meet with a clinician for a Face-to-Face Assessment Screening, they must first complete the following paperwork: Demographic Information Sheet Emergency Contact Form Medical Screening Form o Patient is given a copy of the following: HIPAA Privacy Practices Form (signs receipt of form) Termination of Services Policy Patient’s Rights Non-payment Policy Treatment Policies & Procedure Form (Signs receipt of above) Financial Agreement For Child/Adolescent patient (in addition to the above): Consent for treatment of a minor Developmental and Medical History Emergency Contact Form – minor 42 COMPLETING A FACE-TO-FACE ASSESSMENT SCREENING Once an individual completes the paperwork outlined above and gives the documents to the intake worker to tile in chart, the screener will meet with them for a brief face-to-face assessment screening. Through this assessment, the screener will determine if 1) the individual meets the clinical criteria for admission and/or 2) has a safety risk that needs to be addressed before beginning outpatient treatment. The screener will decide whether to have an authorized staff member do an immediate evaluation for an emergency petition, refer to another facility that is more suitable for the individual’s presenting problem, or give the individual the next available appointment with a therapist at this location. An Intake Screening Form is used to document information gathered during this assessment. (See Intake Screening Form) 43 KEY POINT HEALTH SERVICES, INC. TO: ALL STAFF FROM: CLINIC DIRECTOR RE: NON-DISCRIMINATORY POLICY DATE: JUNE 26, 2006 PLEASE CONSIDER THIS MEMO AS AN ANNUAL, OFFICIAL STATEMENT THAT THIS CENTER IS READY TO MEET THE MENTAL HEALTH NEEDS OF ALL CITIZENS, REGARDLESS OF RACE, AGE, SEX, DISABILITY, RELIGION, NATIONAL ORIGIN, OR POLITICAL AFFILIATION, WHO LIVE IN SOUTHEASTERN BALTIMORE COUNTY. 44 Key Point Health Services, Inc. Admission Criteria Adult Outpatient Mental Health Treatment Program All of the following criteria must be met: 1. The person must be 18 years of age. 2. The person and/or their legally appointed guardian must sign a consent for treatment. 3. The person must show evidence of any of the following: A. Acute psychiatric crisis B. Severe and persistent mental illness C. Short-term, episodic or moderate mental illness (excluded DSM “V___” codes) 4. The person does not present as being at acute suicidal or homicidal risk. 5. The person must show a willingness to participate in and to comply with the treatment plan. 6. Any person who has a history of sexual offenses or violent behaviors will be accepted only upon written consent of the Program Director and the proposed treatment team consisting of the therapist and the psychiatrist. An entry will be made in the progress notes stating the concerns and the willingness to take the case on a trial basis to be signed by all three. The person applying for services will be presented with a contact which lays out clear requirements for remaining in treatment to be singed by that person and the treatment team. 7. Each person is screened for alcohol and other drug abuse during the referral and evaluation process. When it is determined that such issues are primary, the case will not be opened, or if opened then be closed, and the person will be referred to a program specializing in the treatment of chemical dependency. 8. In other cases of dual diagnosis, a period of compliance with a chemical dependence treatment program may be required before admission to Key Point Health Services. Such dual treatment may also be required in order to remain in treatment. 9. Any person who also has a developmental disability may be required to participate in a specialized activity program or residential program as a condition for admission. 45 Key Point Health Services, Inc. Admission Criteria Child & Adolescent Mental Health Treatment Program All of the following criteria must be met: 1. The person must be between the ages of 3 and 17. 2. The person’s parent, guardian or legally appointed caretaker must sign a consent for treatment. A person 16 or older may sign their own consent for treatment. 3. The person must show evidence of any of the following: A. Acute psychiatric crisis B. Severe and persistent mental illness C. Short-term, episodic or moderate mental illness (excluding DSM “V—“ codes) 4. The person does not present as being at acute suicidal or homicidal risk. 5. The person consenting to treatment must show a willingness to participate in and to comply with the treatment plan. 6. Documentation of current immunizations must be provided or a plan to update them is recorded as part of the treatment plan. 7. Any person who has a history of sexual offenses or violent behaviors will be accepted only upon written consent of the Program Director and the proposed treatment team consisting of the therapist and the psychiatrist. An entry will be made in the progress notes stating the concern and the willingness to take the case on a trial basis to be signed by all three. The person applying for services will be presented with a contract which lays out clear requirements for remaining in treatment to be signed by that person and the treatment team. 8. Each person is screened for alcohol and other drug abuse during the referral and evaluation process. When it is determined that such issues are primary, the case will not be opened, or if open then closed, and the person will be referred to a program specializing in the treatment of chemical dependency. 9. In other cases of dual diagnosis, a period of compliance with a chemical dependence treatment program may be required before admission to Key Point Health Services. Such dual treatment may also be required in order to remain in treatment. 10. Any person who also has a developmental disability may be required to participate in a specialized activity program or residential program as a condition for admission. 46 Insert Informal Kinship Care Affidavit Instructions 47 Insert Informal Kinship Care Affidavit Last updated 03/30/06 48 Insert – 20-105 Relative Providing Informal Kinship Care to Child (From Maryland Code/Health-General Title 20.Miscellaneous Health Provisions/Subtitle 1.Consent Provisions/ 20-105. Relative providing informal kinship care to child.) 49 PATIENT RECORD 50 EMERGENCY CONTACT FORM (ADULT) The “Emergency Contact Form” is designed to provide important information about a patient’s next of kin to be used in case of emergency. Primary healthcare provider’s information is also requested, as is health information regarding allergies and patients’ physical limitations. (see Emergency Contact Form – Adult) PROCEDURE All Patients will provide this information upon admission. The patient will be asked to sign the form, authorizing the staff of Key Point Community Mental Health Center to make any necessary contacts in the event of a health care emergency. 51 Insert Emergency Contact Form (adult) Last updated 07/2006 52 EMERGENCY CONTACT FORM (MINOR) The “Emergency Contact Form” for children and adolescents is designated to provide important information about the patient’s primary caretaker, two additional emergency contacts in the event the primary caretaker cannot be reached, and the child’s known health problems, including allergies, to be used in case of emergency. Additionally, the form requests information regarding the child’s primary healthcare provider, the child’s school, and the child’s most recent physical examination and immunization record. (see Emergency Form – Minor) PROCEDURE The patient’s parent or guardian should complete the form, sign and date the form (with a witness signature as well) indicating understanding and consent. 53 Insert Emergency Contact form – Minor Last Updated 07/2006 54 DEMOGRAPHIC INFORMATION FORM The top section of the demographic form is to be completed by the patient at the time of the screening appointment, or in the case of the school based program, at the time of admission. The patient is to verify that the following information is correct: his/her street address, phone number, date of birth, social security number. The patient is also required to fill in their race, marital status, residential arrangements, living arrangements, and education level. The patient will sign and date the bottom of the form. The bottom section of the demographic form is to be completed by the primary therapist at the time of the intake appointment. The therapist will give the admission date, therapist’s name and his/her provider number, the presenting problem and give AXIS I through V diagnoses. A diagnostic impression will be given if the primary therapist has only entry level licensure. The primary therapist will sign and date the form. 55 Insert Demographic Form (two versions – needs updating) 56 ADMISSION NOTE A thorough “Admission Note” is an evaluative tool that can be used to prepare a diagnosis and a treatment plan. PROCEDURE The information to complete the Admission Note must be obtained during the psychosocial assessment. The clinician must include the following information: presenting problem(s), past psychiatric history and hospitalizations, psychosocial history, current medications, clinical assessment, mental status exam, diagnosis or diagnostic impression, including the five axes DSMIV diagnosis, and any additional comments. The form must be completed with the signature of the clinician and date. For those individual clinicians without an advanced license the form must be cosigned by a clinician with an advanced license (psychiatrist, LCPC, LCSW, LCSW-C, etc.). In this instance the patient must also receive a face to face diagnostic assessment by a clinician with an advanced license by the 5th visit. At the tie of the psychosocial assessment the clinician will ask the patient to sign release of information forms for the purpose of gathering additional historical information from the appropriate facilities. Additionally the clinician will determine if there are individuals or agencies with which ongoing open communication would benefit the patient. For example teachers, DSS workers, probation officers, substance abuse counselors. Patients will be asked to sign a release for open communication with these individuals. In the school based program releases for relevant school personnel (for example, teachers and guidance counselors) are required. If a parent/guardian is unwilling to authorize this communication then the child will not be admitted into the school based program and offered alternative sources of treatment such as the clinic. TREATMENT The clinic provides the full range of currently available treatment approaches with the goal of expanding insight, offering support, and educating patients. Treatment is offered via individual, group, and family therapy. Patients requiring additional services are referred to the appropriate rehabilitative and community programs. Treatment is provided by a multidisciplinary team. Therapists, in collaboration with the treating psychiatrist, are responsible for the day-to-day clinical management of the patient, providing psychotherapy, crisis intervention, and family work as needed. By the 5th visit, the Clinician completes an Initial Treatment Plan. The therapist in collaboration with the patient and treating psychiatrist reviews the patient’s progress formally as an ITP review at least every six months. ITP reviews may occur more frequently as the needs and progress of the patient dictates. During the time of intake, the therapist arranges for a psychiatric consult, as indicated. The diagnostic evaluation must be completed by the fifth visit if the initial intake was 57 performed by a clinician with entry level licensure. Refer to psychiatric section for further information. A diagnosis must be by a psychiatrist or an advanced level clinician on or before the fifth visit at the clinic. The psychiatrist completes the diagnosis during the Psychiatric Consult. In cases in which a psychiatric consult is not indicated or if a psychiatrist is not available by the fifth visit, an advanced level clinician will meet with the patient for a brief evaluation and complete and Admission Note Addendum to confirm the treating clinician’s diagnostic impression. 58 Insert Admission Note Addendum 59 Insert Admission Note (Adult) Last Updated 07/2006 60 Insert Admission Note (C&A) Last Updated 07/2006 New Child Admission Procedure (needs to be updated) 61 ESTABLISHING FEES 62 FINANCIAL POLICY To ensure sound fiscal operation, Key Point Health Services, Inc., will secure accurate financial information from patients and will encourage patient responsibility by holding patient’s accountable for their co-payments. Fiscal matters for all Key Point clinic are coordinated through a central office. Information about fiscal responsibilities and resources can be obtained from the administrative offices in Aberdeen. The Administrative office can be reached at 443-625-1600. PROCEDURE At the time of the screening appointment, the patient will provide a copy of all insurance cards and the Financial Information Update Form will be completed. In the school based program these forms will be completed as part of the admission interview. The form will be completed as part of the admission interview. The form will include the patient’s current address, phone number, and insurance information. The person responsible for payment will initial, sign and date the form. Some insurances, especially Health Maintenance Organizations (HMO’s), will not reimburse Key Point Outpatient Mental Health Center for services rendered. Key Point OMHC’s mission is to serve patients in the public mental health system. Because those with private insurances have additional resources and are able to receive services in the private sector, they will be referred to their insurance company for an alternate referral. Exceptions will be kept to the minimum and must be approved by the Clinic Director. While Key Point OMHC provides the full range of mental health services, there are some situations in which we prefer to refer to a specialty provider when appropriate. Questionable circumstances will be reviewed by a clinical supervisor. 63 Insert Financial Form Last updated 09/20/06 DN 64 Insert “Public Mental Health Systems – Uninsured Benefits Guide – effective 7/1/03” 65 ENCOUNTER FORMS 66 ENCOUNTER FORMS Each clinician will maintain a daily record of services provided. At the end of each day, clinicians are to submit a record of their billable services for that day. If the patient has Medicare and the billing is “incident to” another provider, the clinician should write in the name of that provider at the top of the encounter form. 67 Insert Blank Encounter Form 68 PATIENT RIGHTS AND RESPONSIBILITIES 69 Patient Rights includes information detailing rights which should be honored at each appointment. If a patient or family member of a child thinks that their or their child’s treatment is not appropriate or their rights have been violated he/she can request a conference with their therapist’s supervisor. TERMINATION OF SERVICES As termination of services is a natural part of the treatment process, the patient/family member of a child will be notified at admission of Key Point’s policy regarding termination of treatment. The patient receives a copy of the patient’s termination policy. INFORMED CONSENT The concept of informed consent is based on the legal principle that every competent adult, parent/guardian of a child has the right to make decisions concerning a proposed medical treatment and that it is the responsibility of the physician and therapist to provide the patient or parent/guardian with information that is needed in order to make an informed decision. A competent adult is a person 18 years old or older who can make a responsible decision and communicate the same to others. A 16 year old can sign them self in for treatment. It is the policy of the Key Point Health Services, Inc. to provide all patients with reasonable and relevant information concerning their treatment, to offer to the patients a reasonable opportunity to participate in the treatment process, and make decisions about the same based on appropriate and adequate information. PROCEDURE Except in an emergency, all patients shall be informed as to the nature of any recommended or prescribed treatment, with anticipated benefits and potential for significant risks. When true alternatives treatments exist, these alternatives, including the alternative of no treatment, should be presented with benefits and risks involved. The information should be presented in a way that the patient can understand and the patient should be given an opportunity to ask questions and get adequate response. All of the above should be documented in the patient’s record, not only at the initial phase before starting treatment, but also subsequently in the progress note as there are significant changes. Except under extreme emergency circumstances, treatment should not be employed against a patient’s express refusal. The physician may elect to withhold certain information from the patient if, in the physician’s clinical opinion, such information would be harmful to the patient. In this kind of situation, the physician shall document this justification in the patient’s record. 70 In extreme emergencies when there is a reasonable concern involving immediate threat of harm to self or others appropriate care and treatment may be provided without consent, but this should be documented in the patient’s record. For minors, under age of 16, the informed consent is given by parents or legal guardians, as much as possible the patient should be involved in the treatment process. For adults who are not competent to make responsible decisions or communicate the same, the informed consent should be obtained from the patient’s responsible relatives or legal guardian. As much as possible, the patient should be encouraged to participate in the treatment process and decision making process. GRIEVANCE POLICY The intent of the grievance procedure is to find equitable solutions to complaints or problems. All parties must agree that these proceedings will be kept confidential. PROCEDURE It is the policy of Key Point Health Services, Inc. to allow all patients to register complaints about any aspect of their care. The Center Director will make him/herself available to listen to any criticism about the Center or Staff. If a patient has a grievance with any staff member of Key Point Health Services, Inc. he/she is welcome to speak to the primary clinician in person, in writing, or by phone. If resolution of the complaint does not occur, the patient should contact the staff member’s supervisor, by writing or phone. If the complaint remains unresolved, the patient may contact the Center Director. The Center Director will respond in writing or by phone in a reasonable period of time. If the patient disagrees with the final disposition he/she will be referred to the CEO of Key Point for further consultation. The CEO will give a disposition within a reasonable period of time. 71 Insert Grievance Form 72 Insert Non-Payment Policy 73 PSYCHIATRY 74 PSYCHIATRIC CONSULTATION After the initial intake and diagnostic evaluation, the patient is scheduled for a psychiatric evaluation. As indicated, the psychiatrist meets face to face with the patient no later than the fifth visit to confirm the diagnosis, evaluate for medication, and determine if there are any medical conditions present, which might be causing or exacerbating mental health symptoms. The “Psychiatric Consultation Sheet” includes a description of the presenting problem, family history of mental illness and substance abuse; medical history; prior hospitalizations; brief mental status exam and diagnosis. In addition, for patients with a history of treatment with neuroleptic medications the psychiatrist completes a tardive dyskinesia examination. He or she explains possible side effects of any medication prescribed and discuss any contraindications to the plan. He or she documents that these have been discussed. The physician also documents that he or she has read the medical screening form and is thus aware of any medical problems, which may interfere with treatment. If the ITP has been completed the psychiatrist will review and sign it. Thy physician also completes the “Medication Sheet” with the name of the patient, the name of the physician, the working diagnosis, medical problems, any medication allergies or side effects, additional non psychiatric medications that the patient is taking and documents that he or she has discussed the risks as well as the benefits of the proposed medication. For benefits of neuroleptic medication including Tardive Dyskinesia and signed and dates this statement. On this and every subsequent visit the psychiatrist documents on the medication sheet the date of the visit, the name, strength, and dosage schedule of the medication prescribed, whether the side effects were explained, the date of the next appointment and then signs it. These medication management appointments are scheduled according to the clinical judgment of the psychiatrist, but not less often than every 90 days. On each visit the psychiatrist completes a progress note for the visit which provides an assessment of the patient’s mental status and reviews the patient’s progress towards their treatment goals. If there are any changes in status, goals or interventions they note these in the progress note. If they determine that there needs to be a change in the diagnosis they update the reasons for this change. As a treatment facility, Key Point Outpatient Mental Health Center provides a full range of treatment, and does not provide psychiatric evaluations except in the context and course of treatment. Therefore, individuals requesting evaluations only will be referred to alternate, appropriate services. PHYSICAL EXAMINATION As part of the admission process we attempt to obtain physical examination on all patients who receive services at Key Point Health Services, Inc. This physical examination should include documentation of the patient’s somatic health problems, if any, including a history of allergies, neurological disorders, and communicable diseases, 75 and the need if any for somatic care follow-up. If a patient has not received a physical examination and is interested in receiving one we will attempt to provide information on how they may obtain such. We have received a waiver which indicates that we are not required to obtain physical examination for all of our patients (refer to Waiver Addendum). LABORATORY REPORTS The physician on record will refer patients for medical tests whenever they determine that it is appropriate. If a patient does not have insurance to pay for the test or can not afford the test then the patient will be provided with information, if available, on where they may be able to obtain affordable lab tests. When received, lab reports will be delivered to the physician’s mailbox. He or she should review the report and then place it in the “Doctor’s Filing” box. 76 Insert Psychiatric Consultation Sheet (adult) 77 PSYCHIATRIC APPOINTMENT/MEDICATION STATUS FORM A psychiatric appointment/medication status form will be used as a means to notify the residential staff of any changes made during a residential patient’s appointment with his/her psychiatrist. The form will be completed by the psychiatrist at the time of each scheduled appointment. The form will provide written documentation to the residential staff if the patient did not show for his/her appointment, if no medication changes were made, or whether there was a change in medications made (i.e. dosage, strength, addition of new medication, etc.) Once the form has been completed by the psychiatrist it will be collected by clerical staff at the clinic. The clerical staff will then fill in the date and time of the patient’s next appointment. At the end of each day, or the beginning of the next business day, all completed forms will then be sent to the designated residential staff person via fax or interoffice mail. 78 Insert Psychiatric Appointment/Medication Status Form for Residential Patients 79 Insert Fax Cover Page – City/County Residential 80 Insert Medication Sheet 81 TRANSFER REQUEST DUE TO CONFLICTS REGARDING CONTROLLED SUBSTANCES Patients requesting transfer from one psychiatrist to another due to the current psychiatrist’s refusal to prescribe, refill, or increase prescribed controlled substances will have their requests reviewed on a case by case basis by the treatment team. If the treatment team decides that the transfer is being requested solely as a means to access controlled substances or inappropriate levels of controlled substances, the transfer will be disallowed. The patient will then be informed of their options and/or referred out. If the transfer is approved, the receiving psychiatrist must also be fully informed of the treatment team’s decision and must agree to the transfer. 82 PRESCRIPTION PADS Prescription pads should be kept in your medication box. Do not leave them in the desks (from which they may be pilfered). MA prescriptions are automatically translated to generic drugs at the pharmacy. If the physician wants to use non-generic, he or she must document “brand name medically necessary” and then give the reason – e.g. “poor response to generics”, “allergic to generic”. Information on how to use Key Point’s program for providing free medication to indigent patient sis on the inside door of the medication sample closet. 83 MEDICAL WASTE 84 MEDICAL WASTE Guidelines for disposal of needles and infectious waste Infectious Waste Always wear gloves when handling potentially infectious waste. Fomites, which are generated during normal operations (alcohol preps, saliva test paraphernalia, etc.), are to be placed in red plastic bags and disposed of in infectious waste trash receptacle. Sharps Disposal Each facility has been supplied with a sharps disposal container for the collection of used needles and syringes. When the container is ¾ full, it should be placed in the proper receptacle in the Clinic and replaced with an empty one. The sharps are then collected by Bio-Chemical Waste Company for incineration. 85 COURSE OF TREATMENT 86 TREATMENT PLANNING 87 INDIVIDUAL TREATMENT PLAN (ITP) An “Individual Treatment Plan” is the most important document in the treatment process. Because of its central role in the treatment process, much consideration should be given to its development. PROCEDURE An Individual Treatment Plan (ITP) must be written for each admitted patient, no later than the patient’s fifth visit. It should be based on the assessment performed during earlier visits. Progress notes must reflect progress on stated treatment goals. The form includes: The full name of the patient, date ITP was completed, social security number and admission date The patient’s expectations of treatment The patient’s strengths The DSM diagnosis Referrals needed Current medications Transition/Discharge Plans, as appropriate SECTION A: LONG TERM GOALS These goals should be finite, measurable and observable and based on the presenting problem. These goals are generally targets that can be completed in one to five years, or they are ongoing goals (such as absence of symptoms, maintaining stable mood). SECTION B: PROBLEMS, SHORT TERM GOALS & INTERVENTIONS The problem list should reflect the presenting problem. It may not be possible to address all of the problems in 6 months. In those cases, select the problems that are most critical to the patient’s well being. These goals must be numbered. Interventions can include individual psychotherapy, supportive psychotherapy, cognitive and/or behavioral therapy, group therapy, psychopharmacology, family therapy, play therapy, and many other recognized modalities. Also the clinician should note the frequency of the treatment, staff responsible, and a target date. The patient, his legal guardian, family, and significant others, with consent of the patient, shall participate to the extent practical in the development of the treatment plan. In the school based program the parent/guardian may not be present when the treatment plan (ITP or ITPR) is developed. In these cases the parent/guardian will be contact by phone to review the plan and/or sent a copy of the plan for review and signature. The ITP is to be signed and dated by the treatment coordinator (primary clinician) and a psychiatrist if the psychiatrist is medicating the patient. If the primary clinician is not a licensed professional or basic level “LG” clinician, the ITP should be co-signed by the treatment coordinator’s supervisor. The client shall sign ITP and designate agreement or 88 disagreement with the plan. With the individual’s consent, family, significant others or caregivers are encouraged to sign the plan as well. Individuals under the age of 18 must have a parent or guardian sign. GROUP INFORMATION SHEET (used for adult patients only) The Group Information Sheet is printed on the back of Individual Treatment Plans and is used every time an adult patient signs their treatment plan. As part of the treatment planning process, adult therapists will screen each patient for the groups currently offered and make a referral whenever possible. Patients are asked to sign that they have been informed about groups and check off whether they are being referred to a specific group or are declining group at this time. 89 Insert Individual Treatment Plan (ITP) 90 Insert Individual Treatment Plan Review (ITPR) 91 Insert ITP/ITPR Back Group Information Form 92 INDIVIDUAL TREATMENT PLAN REVIEW (ITPR) The “Individual Treatment Plan Review” is completed no more than every 180 days. The therapist, in collaboration with the patient and treating psychiatrist “if applicable”, reviews the patient’s progress. ITP reviews may occur more frequently as the needs and progress of the patient dictates. PROGRESS ON SHORT-TERM GOALS For each short-term goal documented on the ITP, an indication of the patient’s progress on this goal is noted next to the number of the goal. The clinician notes whether the goal is completed, dropped, or continued. NEW SHORT-TERM GOALS AND INTERVENTION If the patient has additional problems or needs, these are to be listed under “new problems, symptoms”. New short-term goals are to be written o address these problems. These new goals should be given unique numbers. (If the initial ITP had goals 1, 2, 3, any new goals on the review would begin with “4”). When there are substantial changes in treatment planning, due to circumstances such as case transfers, significant life events, or crises, the therapist has the option of utilizing an Initial Treatment Plan form to document these changes. The rationale for the change of goals will be explained in the progress notes. Involvement of the patient, guardian, and significant others and the signature protocols are the same as for the initial ITP. 93 Billing for a Treatment Plan Patients who are funded in any way by the Public Mental Health System (PMHS) can be billed a H0032 (internally known as a “24”) when the following conditions are satisfied: 1. The patient must be present to review the treatment plan. If they agree with the plan, they must sign the plan in order to allow for the billing process to continue. 2. The treatment plan must be done at least every six months, but the date of the billing for the H0032 must be the date that the patient signs. 3. H0032’s can be done on patients with MA, uninsured, or MC/MA. Private pay or Medicare only patients are not eligible for this billing code. 4. A separate progress note must be written for this billing stating that the patient reviewed and agreed with the treatment planning process. The note does not have to have a start time/end time. 5. An unlimited of treatment plans can be developed with the patient but only 2 H0032’s can be billed per year. Additionally, the billings must be 120 days apart. 6. Treatment plans must be written on all patients even if the patient’s insurance does not pay for this service, such as Medicare, or private insurances. 94 TRACKING TREATMENT PROGRESS 95 PATIENT ATTENDANCE SHEET 96 PATIENT ATTENDANCE SHEET The “Patient Attendance Sheet” should record all patient appointments, missed appointments, telephone contacts and written contacts either with the patient or with others involved in his or her treatment. PROCEDURE All clinicians/physicians are responsible for recording all contacts (scheduled or unscheduled) for each patient on their caseload. Every contact should have a progress note and a corresponding note on the patient attendance sheet. Record the date, the service code and the disposition of each contact. The number of billable services should be reflected in the far right column. This number may not correspond to the number of visits; if for example two services were performed in one visit. 97 Insert Patient Attendance Sheet Last updated 07/2006 98 PROGRESS NOTE 99 CONTINUING EVALUATION AND TREATMENT Patient’s treatment, including contact with the clinical staff, is documented in the “Progress Note” and on the “Patient Attendance Sheet”. Staff should document the date and start/end time of the visits, whether it was onsite or offsite and indicate the type of service provided. The progress note differs from a contact note or process note in that it details any changes the patient has made on achieving their treatment goals. The note should include a description of the focus of the session, an assessment of the patient’s psychiatric status, a note about the patient’s progress toward goals, and interventions or plans for treatment. The clinician signs the note with his or her credentials (see signature sheet). The date of the patient’s next scheduled appointment is noted. If a clinician who is not licensed to provide Medicare services independently is seeing the patient, there must be the signature of the psychiatrist or certified nurse specialist under (or “incident to”) whom these services were provided. Other events which should be documented in the patient’s chart are missed or cancelled appointments, face to face contacts outside of the therapy session, letters sent to or written on behalf of the patient, telephone calls to the patient or to a third party regarding the patient and/or their treatment. NOTE: During medication management, the physician explains in detail about the medication and the possible side effects of the medication that he/she has prescribed. Frequently a pamphlet will be given to the patient by the physician also explaining the medication. The physician answers all pertinent medical questions. If a patient is taking medication, the following issues should also be addressed in the progress note: Rationale for changes in medication Side effects, if any from the medications Other medication or health issues 100 Insert Progress Note Last Updated 07/2006 101 SIGNATURE SHEET A signature sheet is included in every chart and a copy is included in every response to requests for medical records. The purpose of this sheet is to clearly identify the individuals who may have made notes in the chart. All employees as of 09/18/01 are included on a pre-printed list. Anyone hired after this date must sign the signature sheet in the record of those patients for whom they have written notes. In addition to the name, the sheet clearly identifies the clinician’s credentials. Updated signature sheets are completed as warranted by the number of new clinicians and are added to the chart on top of the older signature sheet. The previous signature sheet remains in the chart for reference. 102 Insert Sample Signature Sheet 103 PATIENT TRANSFERS 104 PATIENT TRANSFER There are circumstances where a patient can be better served by a clinician other than the clinician initially assigned to the patient. In these circumstances, a mechanism exists to reassign the patient to another clinician. PROCEDURE In order to transfer a patient the current clinician must identify a new clinician who agrees to accept the patient. The transfer form must be completed by the current clinician with the following information: the patient’s name and case number (SS#), both clinicians’ signatures and the initials of the Director of Key Point Outpatient Mental Health Clinic. The current clinician must also make sure all information in the patient’s chart is completed and up-to-date. The current clinician will obtain the Director’s approval. If approved, the Director will return original transfer form to the records secretary. In the event a patient has a conflict of interest with their clinician or doctor they are allowed to transfer to a different clinician or doctor one time each during their admission at Key Point. The patient must indicate their desire to change in person, by telephone or in writing to their clinician or doctor. It is the clinician or doctor’s responsibility to identify a new clinician or doctor and collaborate with them regarding the transfer of the patient. If the clinician or doctor agrees to accept the patient, the patient will be provided with the clinician or doctors name and contact information so they can contact them. If the clinician is not an advanced licensed clinician they must collaborate with their supervisor prior to collaborating with an identified clinician or doctor. The clinician will then follow the transfer procedure as outlined above. In the event that a clinician leaves Key Point unexpectedly, it is the Director’s prerogative to transfer that clinician’s caseload. NOTE: If for any reason the Director is unavailable for over a two-day period, the Medical Director, Adult Services Coordinator, or Child/Adolescent Coordinator, in that order, may temporarily initial for the Director until he/she returns. 105 PATIENT TRANSFER POLICY 1. Review the chart prior to the transfer and make sure there are at least 5 APS authorizations and the ITP is up to date. 2. On the attendance sheet write “case transferred”. 3. Write a progress note stating “Case is transferred from (name of therapist and credentials) to (name of therapist and credentials) because (reason, ex: therapist left company).” This is a COMAR regulation 4. Complete transfer form. (see Case Transfer Form) 5. Put transfer form on top of chart and give to your supervisor to review. 6. The chart will then be reviewed by the Clinic Director and signed. 7. The chart is then given to the clerical staff so the change can be made in the computer. 106 Insert Case Transfer Form Last Updated 07/2006 107 UNIVERSAL TRANSFER POLICY When a patient is being transferred from one clinic to another, the following procedure will be followed: 1. The transferring clinician will contact the intake worker at the accepting clinic to ask for the name of a clinician who is qualified to handle the transferred patient. 2. The transferring clinician will give a full report to the accepting clinician, and between the two, and intake appointment will be coordinated. 3. Clerical staff at the transferring clinic will do an updated financial, and will include copies of insurance cards. 4. The transferring clinician will do an updated demographic form including diagnosis. 5. The transferring clinician will make sure there are 5 APS authorizations and the ITP is up to date. 6. The transferring clinic will make sure the patient has enough medications to last until the patient is seen by a psychiatrist at new clinic. The patient’s first appointment at the accepting clinic will be with a therapist. 7. Fees left unpaid will be the responsibility of the clinic in which the fees were incurred, unless other arrangements are made prior to the transfer. 8. Patients will not be allowed to call for their own transfer appointment. 9. Case will be closed in the transferring clinic’s computer for billing purposes, but the case will remain open. 10. The chart, with all updated information, will be sent down prior to the patient being seen at the accepting clinic, with a receipt attached for accountability purposes. 11. Any deviation from above policy must be agreed upon by both clinics and communicated to all parties involved. 12. If the patient does not show up for the first visit at the receiving clinic, the chart will be sent back to the transferring clinic. 108 PATIENT COMPLIANCE 109 PATIENT COMPLAINCE Individual Treatment Plans are used to develop a plan for treatment. In order for treatment to be successful, patients are expected to follow the agreed upon goals stated on these plans. Patients who are noncompliant with treatment recommendations may be discharged. PROCEDURE: Individual Treatment Plans are developed with the patient on or before the patient’s fifth session at the clinic and updated every 180 days thereafter. The therapists, psychiatrist, patient, and guardian (if applicable) sign the document to state that they all understand and agree with the plan. Reasonable efforts are made to ensure that the plan is congruent with patient’s wishes and the goals are manageable for the patient. However, if a patient does not agree with a recommendation on the treatment plan, the team will have to make a decision to either drop the recommendation or make it a requirement to receive services from this clinic. Risk associated with dropping the recommendation must be considered when making this decision. If the patient does not want to sign the plan or fails to abide by the agreed upon goals, the patient should be reminded of the importance of this recommendation. The treatment team should make attempts to engage the patient before sending the patient a warning letter pending discharge. Warning letters must give the patient a reasonable timeframe (typically 14-30 days) to make the necessary changes before closing the case for noncompliance. The letter should clearly specify what is expected of the patient to avoid discharge and provide the date of pending closure if the patient does not follow through. If the patient’s medications are managed by a Key Point psychiatrist, the patient may be allowed to attend on last visit with the doctor before the final discharge date. In order to achieve the goals of keeping all patients current, therapists should review their caseload every 3 months to check for patients who have not attended an appointment during this timeframe. For any 3 month period without any appointments at this clinic, a warning letter should be sent to the patient to try to reengage them into treatment, and if no response, discharge their case administratively. In addition, at each Individual Treatment Plan Review, therapists should review the patient’s progress, suggest new recommendations, develop new goals, and send warning letters to patients who have not kept up with mandatory treatment recommendations. 110 REFERRALS 111 Insert Dundalk Outreach Brief Referral Form 112 Insert PRP Referral Form 113 Insert Crisis Phone Numbers List 114 Insert Referrals 115 Insert Aberdeen Adult Day Services Application 116 Insert Group Referral Form 117 Insert Application for Residential Rehabilitation Services 118 Insert PCSA Application 119 GROUP THERAPY 120 GROUP THERAPY Group therapy services are a specialized modality of psychiatric treatment. Patients are seen in small, face-to-face groups with other patients who have similar problems, diagnoses, or life situations. The efficacy of group therapy is based on the group process, or the interpersonal relations and interactions that occur within the group setting between group members. The group process offers the benefits of a broader interpersonal situation than is available via individual, couples, and family psychotherapies. Change often occurs as a result of the interaction, influence, confrontation, and other forms of verbal and non-verbal feedback that characterize group therapy. Group therapy may function as the primary mode of services received at Key Point CMHC, or it can serve as an adjunct to other forms of psychotherapeutic or psychopharmacological treatments. REFERRAL PROCEDURE When a patient will benefit from, and seems appropriate for group therapy, the clinician will make a referral to the group that will best suit the needs of the patient. It is helpful to discuss the option of group therapy with your patient before referring her or him to a group therapy clinician. Keep in mind that some patients treated at Key Point CMHC are authorized to have only a limited number of sessions per year. Once the group therapy clinician has contact the referred patient and arrangements have been made to begin participation in the group, be sure ton inform the referring (primary) clinician. The primary clinician should monitor the patient’s participation in group therapy by reviewing the progress notes. If changes in frequency of group sessions occur, if the patient is determined to not be appropriate for the group, or if the patient does not attend the group on a sufficiently frequent basis, be sure to alert the transferring clinician. And of course, if any significant clinical concerns arise, take the appropriate steps to deal with the situation, and inform the referring clinician, enlisting her/his assistance. Progress notes are written for each group, reflecting each patient’s progress as it relates to the reasons he or she was referred to the group. These are also noted on the patient attendance sheet. 121 REPORTING REQUIREMENTS 122 ABUSE OF A CHILD Maryland law requires that in any case where a health practitioner suspects child abuse they must promptly report this to the local department of Social Services or the appropriate law enforcement agency. (This refers to the agencies responsible for the jurisdiction where the abuse allegedly occurred. If this information is unavailable a report should be made to the agency serving the area where the patient now lives). The name of the person to whom the report is made needs to be noted in the client’s file and on the written report. An oral report must be made as soon as possible with a written report provided within 48 hours of the intervention or contact where the health professional began to suspect evidence of child abuse. In Baltimore County reports are made to Baltimore County Department of Social Services with the Baltimore County Youth Division accepting abuse reports after hours. A copy of the written report needs to be provided to the local State’s Attorney. In addition, a copy of the report must be provided to the Clinic Director, the Coordinator of the Child and Adolescent Services, and the direct supervisors. An additional copy should be placed in the patient’s chart and a progress note written. The report must contain the following information insofar as reasonably possible: 1. the name, age, and home address of the child; 2. the name, relationship, and home address of the child’s parents or other person who is responsible for the child’s care; 3. the whereabouts of the child; 4. the nature and extent of the abuse or neglect of the child, including any evidence or information available to the reporter concerning possible previous instances of abuse or neglect; and 5. any other information that would help to determine: 6. the cause of the suspected abuse or neglect; and 7. the identity of any individual responsible for the abuse or neglect. NOTE: If the information is obtained by a Key Point employee who is working within a school based program, it may be also necessary to inform he school principal or their designee of the report. This information is provided as part of the cooperative agreement between Key Point and the specific school. If there is reason to believe that the child’s safety may be jeopardized then this overrides the issue of confidentiality. CHILD NEGLECT Suspicion of child neglect must be reported to the local department of social services. Follow the procedure for reporting abuse. However, it is unnecessary to report neglect to law enforcement agencies or the office of the State’s Attorney. ADULTS ABUSED AS CHILDREN In cases where the alleged victim of the abuse is now an adult, the abuse still must be reported. The legal necessity to comply with the law, and the purpose of making a report should be fully discussed with the adult client at the first face to face contact while discussing 123 our confidentiality statement. The emphasis is on identifying children currently in need of protection; it is not DSS’s intention to attempt to substantiate the historical abuse/neglect experienced by the adult client. DSS must accept the report, but they may choose not to investigate due to insufficient information. It is not necessary to provide the name of the adult client. As a general policy, we should not include the name of our client in the report. When to make the report: Generally, reports will not be made at assessment. It is clinically more appropriate for this to be done in the context of an on-going therapeutic relationship. However, if identifiable children are known to be at risk, a report must be made immediately. Otherwise, it should be documented as a part of the assessment that a report is being deferred pending further information and the onset of therapy. It will be the responsibility of the therapist to follow through with the reporting process. If a client does not return for therapy, then the Clinical Coordinator will determine if there is sufficient information to make a report from the file. When making a report please include the following information: 1. the names of current children at risk 2. settings in which the alleged abuser has access to children 3. any information regarding the identity and whereabouts of the alleged offender 4. sufficient details of the historical abuse to determine whether it meets criteria for abuse/neglect 5. information useful for interviewing children currently at risk 6. if your client is at risk or has been threatened by the perpetrator 7. if your client is willing to talk to DSS 8. a contact name and phone number of person making the report 9. whether or not the victim would like to pursue filing charges against the suspected abuser Clinically, it is recommended that the report be completed with the client. The confidentiality statement states that no report will be made without first discussing it with the client. If the client is not ready to provide any details regarding the abuse they experienced, the name of the abuser, or any children who might be at risk, there is insufficient information to make a report. This must be documented in the client’s file in writing. The clinical status of the client must be considered when choosing when to make the report, or when to press for further details. On occasion, the clinical needs of the client may supersede the reporting requirements, e.g. when the client is suicidal. Any time that a therapist feels that a report is not clinically appropriate, or when the abuse occurred out-of-state, she must consult with her clinical supervisor and the Clinical Coordinator. Documentation must be placed in the client’s file regarding consultations, the clinical reasons for delaying the report, and the plan for determining when to make the report. A written report needs to be made if it is known that the perpetrator is no longer around children,, for example if they are deceased. The written report can be made on letterhead and needs to include the information regarding the suspected abuse; a contact name and phone 124 number of the person making the report and whether or not the alleged victim would like to pursue filing charges against the suspected abuser. A call needs to be made to the local department of Social Services only if the suspected perpetrator is currently around children, if this is unknown a call needs to be made. In case of either a written or verbal report a progress note should be written. 125 Insert Maryland Mandatory Reporting Requirements – April 15, 2003 (8 pages) 126 Insert Subpoena (sample) 127 Insert Report of Suspected Child Abuse/Neglect 128 Insert Local Dept. of Social Services & States Attorney Office (4 pages) 129 Insert Report of Suspected Child Abuse (Adults Molested as Children – AMAC) 130 DUTY TO WARN 131 Key Point Health Services, Inc. Dundalk Clinic Inter office memorandum To: All Clinical Staff From: Tessa Worsham, LCPC Re: Our Duty to Warn Date: April 3, 2002 The “Duty to Warn Bill” became law on July 2, 1989. 1. Prior to 1973, no recognized obligation of therapist to protect potential victims from threatened violence of therapists’ patients. Tarasoff v. Board of Regents, 118 Cal. Rptr. 129,529 P. 2d 553 (1974) – Established obligation of therapists to exercise reasonable care to protect foreseeable and identifiable victims. a. In 1969, a UCLA graduate student murdered a fellow student who had rejected his advances. Advised therapist of intention to harm unnamed but readily identifiable victim. Therapist warned police who interviewed and released patient. No one warned potential victim. b. Cal. Sup. Ct. “Once a therapist determines or should have determined a patient poses a serious danger of violence to others, he bears a responsibility to exercise reasonable care to protect the victim from danger.” Reasonable care could include warning the victim, the police, or “whatever other steps are reasonable necessary under the circumstances.” c. Need not reveal all threats – only when disclosure is necessary to avert danger to identified others. In a nutshell, we have the “duty to warn” people our patients are threatening, either by speech, conduct or writing, to harm them. When we notify the potential victim, we are not liable for any legal suit. However, if we don’t notify an intended victim and/or law enforcement personnel, we can be held liable. 132 Our basic procedure will hold. If a patient discusses an intent to hurt themselves or others, we will schedule the patient to see a psychiatrist for a psychiatric evaluation immediately. This is a must and is part of our COMAR regulations. This is considered an emergency situation and would take precedence over a regularly scheduled patient. The next step is to confer with the psychiatrist and form a plan of action. Violating a patient’s confidentiality is not the issue here – our duty is to warn the potential victim. “Duty to Warn” 1. NO cause of action or disciplinary action against any mental health provider or administrator for failing to predict, warn of, or take precautions to provide protection from a patient’s violent behavior unless: a. knows of patient’s propensity for violence; and b. patient indicated by speech, conduct, or writing, the patient’s intention to inflict imminent physical injury upon a specified victim or group of victims. 2. Duty discharged if the mental health care provider or administrator makes reasonable and timely efforts to: a. seek civil commitment of the patient; b. formulate a diagnostic impression and establish and undertake a documented treatment plan calculated to eliminate the possibility that the patient will carry out the threat; or c. inform the appropriate law enforcement agency (mandatory) and if feasible the specified victim or victims of: 1. the nature of the threat; 2. the identity of the patient making the threat; and 3. the identity of the specified victim or victims. 3. No cause of action or disciplinary action under any patient confidentiality act against a mental health care provider or administrator for confidences disclosed or not disclosed in good faith to third parties when discharging these duties. 133 Source: Maryland Code/COURTS AND JUDICIAL PROCEEDINGS /TITLE 5. LIMITATIONS, PROHIBITED ACTIONS, AND IMMUNITIES/SUBTITLE 6. IMMUNITIES AND PROHIBITED ACTIONS - HEALTH AND PUBLIC SAFETY /§ 5-609. Mental health care providers or administrators. § 5-609. Mental health care providers or administrators. (a) Definitions.(1) In this section the following words have the meanings indicated. (2) "Mental health care provider" means: (i) A mental health care provider licensed under the Health Occupations Article; and (ii) Any facility, corporation, partnership, association, or other entity that provides treatment or services to individuals who have mental disorders. (3) "Administrator" means an administrator of a facility as defined in § 10-101 of the Health-General Article. (b) In general.- A cause of action or disciplinary action may not arise against any mental health care provider or administrator for failing to predict, warn of, or take precautions to provide protection from a patient's violent behavior unless the mental health care provider or administrator knew of the patient's propensity for violence and the patient indicated to the mental health care provider or administrator, by speech, conduct, or writing, of the patient's intention to inflict imminent physical injury upon a specified victim or group of victims. (c) Duties.(1) The duty to take the actions under paragraph (2) of this subsection arises only under the limited circumstances described under subsection (b) of this section. 134 (2) The duty described under this section is deemed to have been discharged if the mental health care provider or administrator makes reasonable and timely efforts to: (i) Seek civil commitment of the patient; (ii) Formulate a diagnostic impression and establish and undertake a documented treatment plan calculated to eliminate the possibility that the patient will carry out the threat; or (iii) Inform the appropriate law enforcement agency and, if feasible, the specified victim or victims of: 1. The nature of the threat; 2. The identity of the patient making the threat; and 3. The identity of the specified victim or victims. (d) Patient confidentiality.- No cause of action or disciplinary action may arise under any patient confidentiality act against a mental health care provider or administrator for confidences disclosed or not disclosed in good faith to third parties in an effort to discharge a duty arising under this section according to the provisions of subsection (c) of this section. [1989, ch. 634; 1997, ch. 14, § 9; 1999, ch. 44.] 135 EMERGENCY PETITION 136 Emergency Petition (EP) Policy It is Key Point’s policy that when an Emergency Petition is indicated that they should be completed by a Psychiatrist. If no staff Psychiatrist is available then the Chief Executive Officer will privilege appropriately licensed and credentialed employees to complete EP’s. The state of Maryland has indicated that Social Workers licensed with a LCSW-C and Professional Counselors licensed with LCPC may complete EP’s. In most cases the Clinic Director and one other appropriately licensed clinician may be designated at each site to complete EP’s. When none of the individuals listed above are available the Chief Executive Officer should be contacted and they can issue emergency privileges to another staff member who has a LCSW-C or LCPC to complete the EP. In this final case the CEO will complete the Emergency Privileges Authorization form which will be forwarded to the Human Resources Committee and entered in the Professional Practice Folder. The following is the order of responsibility for assessing patients and completing EP’s: EP’s are to be completed by the Psychiatrist assigned to the case. If they are not present then the patient will be evaluated by a Psychiatrist credentialed to work with that population or if none is available then by any other Psychiatrist on staff. If no Psychiatrist is available then the Clinic Director or the designated Clinician may evaluate the patient and complete the EP. If none of the above listed employees are available then the Clinician with emergency privileges (see above) will evaluate the patient and complete the EP. Whenever an EP is completed by anyone other than a Psychiatrist then a copy of the EP with an attached explanation will be provided to the Chief Executive Officer. If the Psychiatrist, Director, Designated Clinician or any other clinician is not credentialed to work with the specific patient’s age group then it is recommended that they consult with a professional credentialed to work with the specific population. The Chief Executive Officer will ensure that all employees who may complete an EP are appropriately trained on the procedures for evaluating patients and completing the EP forms and process. Possible sequence of employees for completing an EP: Psychiatrist assigned to the case Psychiatrist Credentialed with the population Any Psychiatrist Clinic Director Director’s designee LCSW-C/LCPC with emergency privileges 137 Emergency Privileges Authorization Form The following employee ___________________________________________ has been issued these privileges:_____________________________________________________ _______________________________________________________________________ . These privileges will be in effect from ___________________________ (beginning date) through ________________________ (ending date). As granted by ________________________________________________ Grantee Date (Emergency Privileges may be issued by the Chief Executive Officer) 138 Insert New Emergency Evaluation Law in Effect Oct 1, 2003 139 Insert NAMI Maryland 140 Insert Petition for Emergency Evaluation 141 Insert Certification by Peace Officer 142 INCIDENT REPORT 143 INCIDENT REPORT POLICY: An incident report will be made by the primary person related to the incident for incidents that involve personal injury, property damage, physical threat to clinicians or clients and acts of violence. This report is to be presented to the Clinic Director or Designee by the next working day after the incident. Where there continues to be danger immediate verbal reporting of incident is expected. PROCEDURE: 1. Fill out the incident report as directed on the form. Try to cover clearly the who, what, why, where and when of the situation when possible. 2. Give incident report to the Clinic Director or Designee within one working day after the incident. (Include police report if any.) 3. Clinic Director or Designee will review report and clarify incident. He/she will assess incident to see if any immediate changes need to occur. The review will be signed and dated. 4. The incident report and Center Director/Designee’s response will be reviewed by the QA committee and the form will be signed by the Chairperson of that committee. Need for further changes, if any, will be documented on the back of the Incident Report Form. 5. Incident Reports will be kept on file as part of the Quality Assurance risk management program. 144 INCIDENT REPORTING FORM 145 Insert Preparation of a Significant Event Report (From HR Manual) – 3 pages 146 Insert Significant Event Report Form (HR form 0019) 147 DEATH REPORTS 148 DEATH REPORT In accordance with the requirements of Health-General 10-714, Annotated Code of Maryland, upon notification of the individual’s death: An oral report shall be submitted immediately to: law enforcement official in the jurisdiction and by the close of business the next working day to: DHMH Secretary MHA Director Health Officer in the jurisdiction Maryland Disability Law Center In addition, upon notification of an individual’s death, the Administrative head of the program or facility or his/her designee shall complete a written report of death, using the attached form (DHMH Form 4363 – rev 3/15/04) within 5 working days from the date of the death. The administrative head of the program or facility or his/her designee shall report the death of any individual who resided in or was receiving mental health services at the time of death or who dies within 14 days of discharge or release from any program or facility for which services are funded through the public mental health system or operated by the Mental Health Hygiene Administration under Health General 10-406, 10-901 or 10-902. 149 OUTPATIENT MENTAL HEALTH PROGRAMS RESIDENTIAL CARE AND PSYCHIATRIC REHABILITATION TO: All Clinical Staff FROM: Tessa Worsham, LCPC Clinic Director RE: Death Report When completing a death report, please remember to do the following within 24 hours of your notification of the patient’s death: 1. Complete death report form (DHMH Form 4364) – with the exception of part B Notifications (page 2). 2. Attach original death report to chart and give both to Clerical Staff for notifications. Clerical staff will complete part B Notifications (page 2). 3. Once the clerical staff has made the notifications, faxed and mailed the report to the appropriate agencies, they will return chart to clinician. 4. Clinician will then close the case. 5. A copy of the death report should always be given to the clinic director. If you have any questions, please speak with your supervisor. Revised 02/09/06 jmf OUTPATIENT MENTAL HEALTH CENTER 7702 DUNMANWAY · BALTIMORE, MARYLAND 21222 Phone 410-282-1792 · Fax 410-282-3195 www.keypoint.org 150 Insert Death Report Memo Insert Death Report Fax Cover Sheet Insert DHMH Form 4364 – Death Report 151 DISCHARGE 152 DISCHARGE Termination of patient services (discharging) shall, wherever possible be a collaborative process between patient and therapist. When an individual is admitted for services, they shall be informed of the discharge policy and documented in patient’s medical record they have been so informed. PROCEDURE When a collaborative decision for discharge has been made, the therapist shall prepare a discharge plan based upon the patient’s current clinical status, service needs and mutually agreed upon goals and make necessary referrals. If a patient has not participated in treatment for a period of 90 days, a decision to discharge the patient may be made after the therapist has made a reasonable effort to re-engage the patient. (See non-compliance with scheduled appointments). Patients may be referred elsewhere for the following reasons: Patient’s request On evaluation, patient has been found to be inappropriate for clinic participation – i.e. significant substance abuse as primary diagnosis, without a willingness to see concurrent substance abuse treatment; not diagnostically appropriate Patient has been unwilling or unable to participate in treatment over an extended period of time Patient has been unable to be maintained as an outpatient for any significant interval of time PRIOR TO DISCHARGE FROM THE CLINIC Therapist attempts to speak with the patient to discuss reasons for termination and to devise an appropriate termination plan. If this is not possible, the clinician shall send out an outreach letter. When discharge is at the patient’s request, the therapist meets with the patient to discuss this wish and to help clarify the underlying issues leading to his/her desire to leave the clinic. When the patient and team determine that discharge is appropriate, the therapist works with the patient to provide an aftercare plan. When a patient refuses to participate in aftercare procedures, the therapist makes reasonable efforts to re-engage the patient or to document the patient’s reason for discontinuing services. The therapist will send the patient a written notice of pending discharge and may then discharge the patient and document that effort in patient’s medical record. If the patient does not respond within two weeks, the clinician will discharge the client. A Discharge Summary shall be prepared within 10 working days after a patient has been discharged and signed by therapist and treating psychiatrist. The discharge form is signed by 153 the Center Director and then given to the Records Secretary to enter the information into the computer. The original form must be filed into the patient’s chart. 154 Insert Discharge Form 155 SCHOOL BASED PROGRAM 156 SCHOOL BASED PROGRAM Many of the policies and procedures in the school based program are nearly identical to those in the clinic. Minor differences are integrated into the specific sections of this manual. However, some policies and procedures are distinct so they are included in this separate section. APPLICATION FOR SERVICES In the school based program the school completed the Key Point Referral Form. The completed form is forwarded to the therapist in that school. The Key Point therapist reviews the referral and if it is complete determines eligibility through the public mental health system. If eligible they contact the family. A record of all outreach to the family or contact with the school is indicated in the disposition section of the referral form. If the parent/guardian wishes to start treatment, the therapist completes the Application for School based Mental Health Services and schedules them for their Admission interview. If the family is not eligible, unable or unwilling to complete the application, or the therapist has been unable to reach them after at least two calls this is also indicated on the referral form in the disposition section. The school liaison is informed of the status of all referrals that can not be completed and encouraged to assist us in resolving obstacles whenever possible. The application form is completed by the therapist to determine eligibility and appropriateness for the school based program. It covers much of the same information that is covered in the Screening Interview in the clinic. Completed application forms will be placed in the chart in section 4 in place of the screening form. ADMISSION PROCESS In the admission interview the therapist meets with the parent/guardian to complete the various admission and official paperwork and identify their concerns or goals for treatment. In order to minimize the disruption from school time, the child will not join the session until after the office forms are completed. APPLICANTS IN CRISIS OR DANGER All children referred to the school based program will be assessed for safety as part of the admission process. If it is determined that they can not be safely managed in the program then the parent/guardian will be encouraged to take the child for emergency treatment. If it is determined that the child’s risk requires immediate attention then the clinician will notify school personnel to enlist assistance to provide immediate safety for the child as well as other children in the school. Since each school has a policy to manage children at risk the Key Point therapist will inquire about this policy and participate in the school procedure. They will notify their Key Point supervisor of the situation and if necessary an advanced level therapist who is credentialed to complete and emergency petition will meet with the child and parent/guardian to provide an emergency assessment. PATIENT COMPLIANCE In the school based program all patients are encouraged to continue treatment when school is not in session. During the summer if they are unable to continue treatment the therapist in consultation with the treatment team will determine if the case should remain open until school reopens in the fall. At that time it will be determined if the child is still in the school 157 or could receive services through another school served in the program or the clinic. If they are not interested or eligible for treatment at that time in the school based program the case will be closed. The participation of the parent/guardian is required since it is vital for the success of treatment. As part of the treatment plan the frequency of their involvement will be specified. If they do not follow through with this plan the case will be closed unless the treatment team decides that this discontinuation is contraindicated. If treatment is terminated the school liaison will be informed of this decision so they may assist in developing alternative plans. PSYCHIATRIC AND DIAGNOSTIC EVALUATION All patients in the school based program are offered the option of meeting with a Psychiatrist in the clinic. If the parent/guardian refuses to meet for a Psychiatric consultation this will be noted on the Psychiatric Consultation form. In that case the primary therapist will provide a diagnosis (if they are credentialed to do such). If they are not licensed and credentialed to provide a diagnosis then the therapist will arrange for an advanced level therapist to see the patient prior to the fifth visit to complete the diagnosis. The advanced clinician will review the Admission Note and other documentation. They will meet with the patient and parent/guardian whenever possible to complete the assessment. The advanced clinician will either complete a new Admission Note or complete the Admission Note Addendum and a progress note that details the assessment. EMPLOYEE SAFETY The safety of the Key Point therapist is a significant concern in the school based program. This is achieved through a variety of means. These include policies on the use of school facilities, home visits, and accessibility during work hours. All school facilities used by Key Point employees must be safe and in areas where other school staff are nearby. The space used must be secure and private in order to maintain the confidentiality of the treatment. Due to the limited availability of school phones all therapists must carry either a pager or cell phone so they may be reached by clinic staff. 158 SCHOOL BASED PROGRAM CELL PHOEN REIBURSEMENT PROCEDURE School Based Employees who choose to participate in the Cell Phone Reimbursement Program must follow the following procedures for reimbursement. 1. All requests for reimbursement will be submitted by the tenth of the month for which reimbursement is sought. To be eligible the employee must work at least 1 day in the school during the calendar month with their cell phone on and available for Key Point use. 2. Requests will be completed on the Check Requisition Form (see Sample) and submitted to the School Based Coordinator. 3. The School Based Program Coordinator will review all requests for eligibility. Approved requests will be submitted to Administration for reimbursement by the end of the month for payment. Requests that are not eligible will be returned to the employee with an explanation. 4. Requests must be completed in full (see sample) at the time of submission or they will be returned to the employee. 159 Insert Sample Check Requisition Insert Referral To Key Point Health Services Form Insert Application for School Based Mental Health Services 160 QUALITY IMPROVEMENT 161 PERFORMANCE IMPROVEMENT PLAN 162 PROGRAM IMPROVEMENT PLAN (10.21.17.10B) The Quality Assurance and Improvement (QAI) Plan monitors the many aspects of quality care, including the procedures for monitoring and improving staff performing. The PI Plan goals are: 1. To ensure that patients receive appropriate quality service and treatment according to presenting problems. 2. To ensure that services are accessible, collaborative, appropriate and continuous. 3. To ensure that the Clinic is accountable to patients; that all patients are treated with respect and dignity; and that patient rights are protected. 4. To ensure that clinical staff are appropriately trained, credentialed, privileged, and supervised in the execution of their responsibilities. RESPONSIBILITY The Center Director has overall responsibility for the monitoring and execution of the PI Plan. The Director delegates to the PI Committee, the responsibility for the process of quality assurance and improvement, risk management and outcome reporting. The committee consists of supervisory staff. Other staff are invited as needed. MECHANISM FOR IMPLEMENTATION The primary mechanism for implementation of this plan is the PI Committee that meets at least monthly to create, implement, monitor and evaluate clinic practices. Other PI measures are semi-annual audits (record reviews); program evaluation; periodic surveys of patient satisfaction; regular individual and peer supervision according to level of privileging. See PI Plan for specifics. PI Committee members maintain a record of minutes on a rotating basis. The results of all monitoring, evaluation, and problem solving are kept in the minutes. This following plan was revised and approved by the PI Committee of the Dundalk Clinic. 163 CONTINUOUS QUALITY MANAGEMENT 164 CONTINUOUS QUALITY MANAGEMENT Key Point at Dundalk is committed to providing quality services which are delivered efficiently and effectively, and therefore maintains a Continuous Quality Management (CQM) process which includes: Quality Assurance – the systematic and objective monitoring of the quality and appropriateness of care Performance Improvement – the pursuit of opportunities to improve patient care Risk Management – the resolution of problems identified through monitoring and evaluation activities Outcome Reporting – evaluation of the effectiveness and efficiency of the delivery of services The cornerstone of this process is a written Performance Improvement Plan, which is reviewed at least every three years. The PI Plan outlines the process for evaluating the quality of care and provision of services with emphasis on accountability, efficiency, collaboration, continuity of care and accessibility. It includes the staff responsible, and mechanisms for implementing the process. SECURITY AND CONFIDIENTIALITY OF RECORDS Files are kept in locked file cabinets in the central office. Files are opened at 8:00a.m. Charts are to be returned to be filed before the end of the business day to the locked chart room. Patient records are not to be left on desktops. PERFORMANCE IMPROVEMENT INDICATORS I. PROCESS INDICATORS A. RECORD REVIEW 1. Completed quarterly (all records opened since previous audit will be included) and reported quarterly. Monitored by Center Director and PI Committee. 2. Goal is 85% threshold for all items specified otherwise. a. Does chart meet COMAR requirements? b. Diagnostic Evaluation within 5 visits. c. Initial assessment completed on admission. d. Treatment Plans (ITP, ITP-R) meet timelines and requirements. e. All required signatures are present on the plans. f. Risks & Benefits of medication documented (within past year and when new class of medication started). g. All entries dated and appropriately signed. h. Documented contact or outreach attempt in past 90 days. B. OTHER PROCESS INDICATORS 165 1. Current identified indicators monitored quarterly and responsible party: a. The “No-show” rate will be less than or equal to 25% for adults and children. Process to be monitored by Center Director and PI Committee. II. OUTCOME INDICATORS A. Conduct client satisfaction survey yearly with a minimum of 90% satisfaction. B. Key Events Review Results reviewed at the Quarterly PI Meetings. 166 RECORD REVIEW 167 CHART AUDIT (RECORD REVIEW) A formalized audit is conducted twice a year, every 6 months, January and July. Clinicians do a self audit of their own charts. Supervisors do a representative sample of 10 of the charts. The expectation is that 85% of the charts will meet the expected COMAR standards. If the chart is deficient, the chart and records review check list is returned to the primary clinician to correct the deficiencies. At the next supervisory opportunity, deficiencies in the charts will be discussed. Once the supervisor is satisfied that the chart is up to standards, he or she will sign off on the checklist. The audit process is coordinated by the office manager. A copy of supervisees chart audit goes to the supervisor. There will be chart reviews done January and July of each year. The following questions guide the audit: 1. Are signature sheets present which allow the reader of the chart to identify the author or each progress note or med sheet notation? 2. Are the financial forms in order? 3. Is there documentation that the patient was notified of treatment policies and patient rights, and has given consent for treatment? Has the parent or guarding of a minor consented to treatment for that minor? (Adolescents 16-18 may sign themselves). For children, is there evidence of custody status? 4. Are the treatment plans timely and accurate? Are goals specific, measurable, and attainable within the timelines established? Does the diagnosis on the treatment plan match the diagnosis on the psychiatric consultation? Is the diagnosis supported by the presenting problem? Are the interventions suggested appropriate for the diagnosis? Is the frequency of the sessions noted? Are treatment plans signed by the prescribing psychiatrist? Is the treatment plan singed by a licensed therapist, or if signed by a non-licensed therapist is it cosigned by an advanced licensed therapist? If no doctor is seeding the patient, is the treatment plan singed by a licensed therapist and an advanced licensed therapist? If therapist is unlicensed, an advanced licensed therapist could sign for doctor. 5. Does the admission note clearly state the presenting problem and support the diagnosis? 6. Has the psychiatric consultation been completed with all five axes? Has the medical screening form been reviewed by the doctor? Has there been appropriate follow-up for identified medical problems? Are medication side-effects explained? Is the medication sheet completely, accurately, and clearly completed, if medication was prescribed? Is there a notation on the medication sheet of any allergies and other medications? 7. Is the treatment plan being followed? Do the progress notes reflect progress toward the goals as outlined on the treatment plan? Do psychiatric progress notes reflect rationale for changes in medication or diagnosis? 8. Has an effort been made to collaborate with other providers (past or current)? Is there authorization to speak with other interested parties (i.e. family, social workers, and teacher)? Has the clinician attempted to obtain records of past treatment particularly as they relate to the diagnosis? 168 9. Has the clinician made an effort to uphold the continuity of care by obtaining an aftercare plan for any patients coming directly from the hospital? 10. Have we received results of a recent physical exam within six months of admission? If not, has the psychiatrist granted a waiver? For children and adolescents, is there documentation of immunization? Note: Refer to record review form elsewhere in the back of the manual. A separate description and explanation will be given for the 16 questions on the form. EXPLANATION OF THE RECORD REVIEW FORM For all the number items check whether it’s ok or deficient. 1. There should be a signature sheet (current) with therapists and doctors signatures on the second flap of the chart. The HIPAA receipt signed goes on top of the signature sheet. 2. Financial form (2 signatures in past 12 months at the bottom of the page) should be completed. 3. Signatures are present on Adult Services Policy Participation. 4. Adult Emergency Contact form is to be signed and dated. 5. Treatment plan is to be done by the 5th visit. It contains signatures of the clinician of record, patient, and other licensed staff where appropriate. Circle what is missing. If patient sees a doctor for medication his/her signature should be on treatment plan. Treatment plan diagnosis should match psychiatric consultation diagnosis. If not, treatment plan should be changed to reflect the doctor’s diagnosis. Treatment plan should be reviewed every six months with signatures and 5 diagnostic Axis being used. Provider and frequency of treatment being conducted should be noted on the plan. Treatment plan goals should be operationalized in finite, measurable and observable terms. Short-term treatment goals are not to be numbered. Goals are numbered once and numbers cannot be repeated elsewhere in future plans. 6. Admission note done and signed by licensed staff. If staff is unlicensed it must be cosigned by a supervisor. All your pages of the Admission Note must be filled out. If the therapist has a LGPC or LGSW, the note must be signed and read by a licensed supervisor. 7. Psychiatric Consultation – all four pages must be filled out. The psychiatrist will complete a tardive dyskinesia exam if necessary. IF a medication is prescribed, side effects are documented and that they have been discussed. 8. Medication sheet should be completely filled out, signed, and dated. If the medications that are used cause risks or tardive dyskinesia, it must be documented that the doctor discussed this with the patient, then signed and dated. 9. Progress notes should consist of start and end time, reflect progress towards treatment plans and the focus of session contain some statements describing the patient status. The mental status part should be filled in as well as the diagnosis. Additionally, a 169 future intervention plan may be described. It should be signed by therapist, a supervisor if necessary. 10. Reports should be sent for and filled on first left flap. Such reports should be from recent hospitalizations, medical doctor, consultations, and former places of treatment, and data about the treatment. 11. An aftercare plan should be requested from a hospitalization to inpatient unit. 12. There should be a form of APS visits for therapy and for med visits. The therapist should go through the contents of chart and organize them according to the list on the back of the review form. Complete the following for child & adolescent cases only: 13. There should be a copy of recent immunizations in each child’s chart. Proof of the child’s legal status (birth certificate and if necessary, proof of custody papers). 14. The child emergency contact form should be fully filled out and signed by the parent or guardian. Parents should be prepared to give 2 emergency contacts to call. 15. The consent for treatment of a minor should be filled out and signed. 16. The parent or guardian should completely fill out the 3 page child and adolescent developmental and medial history. 170 Insert Record Review Form 171 CREDENTIALING AND PREVILEGING 172 PRIVILIGING AND CREDENTIALING Privileging is one mechanism to ensure that quality is provided to clients of the center by establishing standards for the type of clinical services each staff is qualified to provide and the level of staff supervision required. All clinical staff must apply to provide specific clinical services. There are two levels of practice for therapists. The Basic Level is designed for individuals who have at minimum a Master’s degree and are licensed at the entry level as a Mental Health Professional. These include Licensed Graduate Professional Counselors (LGPS) and Licensed Graduate Social Workers (LGSW). They receive individual supervision with an approved advanced level supervisor. The Advanced Level individuals have at minimum a Master’s degree and are licensed at the independent level as a Mental Health Professional. These include Licensed Certified Professional Counselor (LCPC), Licensed Certified Social Workers, Clinical (LCSW-C), and Advanced Practice Registered Nurse in Psychiatric Mental Health (PRNPMH). They receive supervision in the Peer group as well as individual supervision as needed. Master’s Level students from several local programs participate in internships at the clinic. These students must work under the supervision of a licensed staff member who has been approved by Key Point to perform this level of supervision as well as the school in which the intern attends. PROCESS Privileges are awarded based on an application completed by the employee and as approved by the clinic director. This approval is based on the applicant’s credentials and experience, job duties, and as limited by law or regulations specific to their profession. The Human Resources Committee assists by maintaining and verifying records of the employee’s credentials. The privileges and credentialing request form is completed at the time of employment and renewed on an annual basis. Employees maintain licensure by following the requirements of their professional licensing board. REQUIREMENTS FOR PRIVILEGING Listed below are services for which privileges may be requested. Restrictions based on licensure, experience and professional are noted (see Application for Clinical Privileges). Admission/Evaluation: An Admission Note may be completed by any Mental Health Processional. It involves obtaining a psychosocial history and mental status examination of the patient and is documented on the Admission Note. Case Management: This may be completed by any Mental Health Processional. Responsibilities are limited to the basic management of a case and referrals to other services as indicated for quality treatment rather than a comprehensive Case Management Program. 173 Psychopharmacology: Medication management may be provided by a Board eligible Psychiatrist or other professional who may prescribe medications in the State of Maryland. This includes the provision of medications and monitoring of such as based on good practices. Diagnosis: A diagnosis may be provided by an Advanced Level Mental Health Professionals who are permitted to diagnose based on the professional board. These include Board eligible Psychiatrists, Psychologists, LCPC, LCSW-C, APRNPMH. The diagnosis is based on the assessment and history of the patient and meets the criteria listed in the most recent Diagnostic and statistical Manual (DSM-IV-TR). Diagnostic Impression: This may be provided by any Mental Health Professional. It is based on the assessment and history of the patient and meets the criteria listed in the most recent DSM-IV-TR. Family/Couples Therapy: To provide these services a Mental Health Professional must have training specific to therapeutic work with families and couples. Group (not-therapy) facilitation: This entails public education and other pre-certification that are not clinical in nature. Employees who provide educational presentation to the public may be privileged. Group Therapy: This may be provided by any Mental Health Professional who has experience and training to the specific population. Individual Therapy: This may be provided by any Mental Health Professional. Injections: Injections may be provided by Nurses and Physicians. Involuntary Commitment: Involuntary Commitment covert two sections, certificates of Commitment and Emergency Petitions. Certificates of commitment may be completed by Psychiatrists. Emergency Petitions are completed by Psychiatrist or, in the absence of a Psychiatrist, by Mental Health Professionals who are permitted to do such as part of their licensure and been trained on such. These include the following professionals: LCSW-C, LCPC, and APRNPMH. Psychiatric Evaluation: This is a diagnostic and treatment assessment completed by a Board eligible Psychiatrist. It entails a thorough history of the presenting mental health problem and the obtaining of any other relevant information for the development of an accurate diagnoses and treatment plan. Psychological Testing: Individuals may be privileged for this in those cases where they have received specific training and are licensed to independently perform the application or interpretation of psychological tests. 174 Supervision: Supervision may be provide by a mental health professional who has achieved licensure as an independent practitioner, have training or experience relevant to the specific supervision and are assigned supervisory tasks. They may provide administrative and/or clinical supervision of other assigned mental health professionals in the agency. Populations: Employees are privileged to serve one or more client age groups. These are designated as follows: Child and Adolescent (age 0 to 18), Adult (age 18 to 65), Geriatric (age 65 and older). Approval is based on training and expertise with the specific group, as well as such things as criminal background checks (working with children). 175 EMPLOYEE SUPERVISION 176 EMPLOYEE SUPERVISION All clinical employees receive supervision. The level of supervision is determined by several factors: licensure level, demonstration of proficiency in a specific services, and completion of orientation to Key Point. New employees receive intensive supervision as part of their orientation. As they demonstrate skill in a particular modality they may receive supervision appropriate to their level of licensure. Employees at a basic level (LGSW, LGPC) must receive regular (usually weekly) individual supervision with an agency approved supervisor. This supervision may be divided between administrative and clinical supervisors in order to meet licensure requirements. Employees licensed as Independent Practitioners and who have demonstrated proficiency receive clinical peer supervision. This involves two or more advanced level clinicians discussing cases and is held at minimum once a month. For Advanced level clinicians, administrative supervision and periodic individual clinical supervision will continue to be provided by agency designated supervisors. Any employee, irrespective of licensure, who has not demonstrated proficiency in a particular skill will receive individual supervision until they demonstrate that skill. Student inters receive, at minimum, weekly individual supervision. All clinical staff as well as student inters are expected to participate in the peer supervision groups. These are divided between the adult and child & adolescent teams in order to focus on pertinent clinical issues of those specific populations. 177 SUPERVISOR/SUERVISEE DOCUMENTATION CATEGORIES: 1. Clinical Supervision 2. Administrative Notes 3. Productivity Information 4. Deadline Checklists 5. Corrective Measures 6. Schedules and Schedule Changes 7. Evaluations 8. Personnel Information 178 Insert Child And Adolescent Weekly Service Report Insert Application for Clinical Privileges 179 CONTINUED EDUCATION AND REQUIRED TRAINING 180 REQUIRED TRAINING AND CONTINUED EDUCATION The company ensures that staff receives the training required to perform their job duties. CPR and First Aid training is provided onsite for all direct care staff. Recertification is provided as required. Key Point also requires all employees to attend trainings in Fire & Safety and Infectious Disease Control held onside annually. The company also offers to pay the co-payment for the Hepatitis B vaccination for employees who want it. Administrative time off is provided for trainings and workshops related to job duties when the training is not offered onsite. Essential Learning is the name of a training system used by Key Point to further train and develop staff on-line. Essential Learning uses a concept called “competencies” to make the set-up, maintenance, and reporting of training requirements easy to manage. 181 STUDENTS & VOLUNTEER POLICY 182 STUDENTS, INTERNS AND VOLUNTEERS The Center Director delegates responsibility for the placement of students and volunteers to a senior staff member (Masters level and above) who coordinates prospective students and volunteers and acts as a liaison between the Center and the Schools. Licensed members of each discipline supervise students from that discipline, i.e., a psychiatrist supervises medical students, a psychologist supervises psychology interns, etc. It is the policy of this Center not to accept undergraduates for training in Clinical Work. The following supervisor practices shall be followed to ensure continuity of care and quality assurance: All students shall receive on a formal basis at least one hour of supervision each week. This supervision shall be set aside on a regular basis, at which time clinical issues, procedures for the proper maintenance of a case, clinical techniques and modalities and case management will be discussed. This supervision is on an individual and group basis, meeting for at least one hour per meeting time. All new admissions to KPCMHC that are processed by students are required to have a collaborative psychiatric consult by an M.D. and the student will have a face-to-face collaborative consult to discuss the new admission with his or her supervisor. Informal supervision is also required on a day-to-day basis, especially for beginning interns. All students, upon arrival to KPCMHC, shall receive an in-depth orientation to include a tour, review of Policy and Procedure Manual, and operating procedures. Is it the policy of KPCMHC that field training of students from appropriate counseling, social work, nursing, and psychology programs is a worthwhile contribution to the future development of professionals in the mental health field. In addition, students can provide direct clinical services such as admission, individual and group psychotherapy, the careful selection and weekly supervision of these interns assure that quality of service is maintained. PROCEDURES So that quality of service is maintained, the following procedures must be followed in the selection of students: All prospective students should submit a vitae that reflects professional experience, educational achievements and volunteer work: educational goals and professional plan should also be reflected in the vitae. All students shall be interviewed by the Program Director or his designee, prior to being assigned to a Staff Supervisor. Once accepted as an intern, the Staff Supervisor will be the person responsible for the assigning of patient cases and monitoring student work through weekly supervision. 183 FIRE SAFETY 184 FIRE SAFETY Staff, patients, and visitors shall begin to exit immediately upon receiving the verbal alert. All persons shall proceed to exit in an orderly fashion from the building, using the nearest exit, closing office doors upon exit. Do not return to the office after departure until cleared by the fire marshal(s). The Fire Marshals will station themselves in close proximity to the exits and assist in maintaining good order throughout the evacuation process. Fire Marshals will be responsible for verifying that the evacuation of the assigned area is complete, including the rest rooms. The Fire Marshals will then leave the building and congregate in the parking lot facing the building. Every effort should be made by all to make the evacuation quick and orderly. Visitors and patients are to be led to safety outside of the building. In the case of an actual fire in the building, whoever discovers the fire will begin verbal alert and notify the Front Office or a designated Fire Marshal in the main building and in each of the trailers. The front office staff or a designated Fire Marshal shall notify the Fire Department by calling 911. No employee will return to the building until directed by the Fire Marshals or by the Fire Department. No one should engage in fire suppression activities during an evacuation unless it is absolutely necessary to prevent injury to others. The Control point is the parking area. ARMING AND DISARMING ALARM SYSTEM To trigger the fire alarm grasp the bar on the fire alarm box located near the front door and pull down. The monitoring center at 911 will be notified immediately and the Fire Marshal will ensure that everyone leaves the building immediately. To turn off the alarm, open key box with key labeled “key box” remove 3 keys located on hook number 5. Use red key to set the faceplate back on the pull station; use the key labeled “fire system reset” to move the slide button from left to right (reset) and hold the button to the right until alarm bells stop ringing. The button will automatically go back to the left (the alarm has been reset). EVACUATION Floor maps showing evacuation routes are posted and evacuation drills conducted. If a fire occurs in one of the evacuation pathways, the Fire Marshal will close off the area and direct traffic to the next nearest exit. 185 ROUTES For 7702 Dunmanway: Primary exit is through doors that open directly to the outside of the building. Secondary exits are those that open to the corridor and exit at either end. (marked by exit signs) For Trailers: Exit nearest door. 186 FIRE INSPECTION REPORT 187 Insert Most Recent Fire Inspection Report 188 BOMB THREATS 189 BOMB THREAT PROCEDURES All bomb threats or suspicious objects will be treated seriously. The safety of patients, employees and the public is paramount. The building will generally be evacuated. The decision whether to evacuate a building will be made by the highestranking employee of the center who is present, with the advice of the police and/or fire department. The person receiving the call of a threat or finding a suspicious object should report it immediately. He or she should not touch the object but is to gather as much information as possible. Then he or she will report to the highest-ranking employee on the premises and then to the police and/or fire department. The fire marshal will instruct the public to evacuate by the nearest fire exit and then will also leave the building. No one is to return to the building one it is evacuated. Staff, patients and other visitors should congregate outside the building as directed and wait for further instructions. 190 PATIENT AND STAFF SAFETY 191 ANTHRAX POLICY In the extremely remote event that we come into contact with an Anthrax contaminated parcel, the following guidelines are issued by the United States Centers for Disease Control. 1. Anthrax organisms can cause infection in the skin, gastrointestinal system, or the lungs. To do so, the organism must be rubbed into abraded skin (an open wound), swallowed, or inhaled as a fine, aerosolized mist. Disease can be prevented after exposure to the anthrax spores by early treatment with the appropriate antibiotics. Anthrax is not spread from one person to another person. 2. For anthrax to be effective as a covert agent, it must be aerosolized into very small particles (made into an aerosol). This is difficult to do, and requires a great deal of technical skill and special equipment. If these small particles are inhaled, lifethreatening lung infection can occur, but prompt recognition and treatment are effective. IDENTIFYING SUSPICIOUS PACKAGES AND ENVELOPES Some characteristics of suspicious packages and envelopes include the following: Inappropriate or unusual labeling o Excessive postage o Handwritten or poorly typed addressed o Misspellings of common words o Strange return address or no return address o Incorrect titles or title without a name o Not addressed to a specific person o Marked with restrictions, such as “Personal, “Confidential”, or “Do not x-ray” o Marked with any threatening language o Postmarked from a city or state that does not match the return address Appearance o Powdery substance felt through or appearing on the package or envelope o Oily stains, discolorations, or odor o Lopsided or uneven envelope o Excessive packaging material such as masking tape, string, etc. Other suspicious signs o Excessive weight o Ticking sound o Protruding wires or aluminum foil HANDLING OF SUSPICIOUS PACKAGES OR ENVELOPES If you see a suspicious, unopened letter or package: Do not shake or empty the contents of any suspicious package or envelope. Do not carry the package or envelope, show it to others or allow others to examine it. Put the package or envelope down on a stable surface; do not sniff, tough, taste, or look closely at it or at any contents which may have spilled. Alert others in the area about the suspicious package or envelope. Leave the area, close any doors, and take actions to prevent others from entering the area. If possible, shut off the ventilation system. 192 Wash hands with soap and water to prevent spreading potentially infectious material to face or skin. Seek additional instructions for exposed or potentially exposed persons. If at work, notify a supervisor, a security officer, or a law enforcement official. If at home, contact the local law enforcement agency. If possible, create a list of persons who were in the room or area when this suspicious letter or package was recognized and a list of persons who also may have handled this package or letter. Give this list to both the local public health authorities and law enforcement officials. If you see a suspicious envelope with powder and powder spills out onto a surface (floor, table, etc.) 1. Do not try to clean up the powder. Cover the spilled contents immediately with anything (e.g., clothing, paper, trash can, etc.) and do not remove this cover! 2. Alert others in the area about the suspicious package or envelope. Leave the area, close any doors, and take actions to prevent others from entering the area. If possible, shut off the ventilation system. 3. Wash hands with soap and water to prevent spreading potentially infectious material to face or skin. Seek additional instructions for exposed or potentially exposed persons. 4. If at work, notify a supervisor, a security officer, or a law enforcement official. If at home, contact the local law enforcement agency. 5. If possible, create a list of persons who were in the room or area when this suspicious letter or package was recognized and a list of persons who also may have handled this package or letter. Give this list to both the local public health authorities and law enforcement officials. 193 VIOLENCE – POLICY & PROCEDURES 194 VIOLENCE – POLICY AND PROCEDURE 1. If clinicians has reason to believe that a client may be potentially violent, arrange to have another clinician in the office at the time of service and leave door open in order to allow easy exit. 2. A basic premise to follow is “if in doubt, shout”. Literally, this means that you should not try to handle a violent person by yourself. Get help immediately by calling aloud for help and using the telephone. You do not have to wait for actual physical violence is imminent or likely is sufficient. It is better to have to tell the police when they arrive that the situation is resolved than to risk injury to ourselves, other patients or bystanders. 3. Physical intervention is to be avoided as far as possible. We do not have the training or physical facilities for physical restraining violent persons that the police and hospitals have. Moreover, such attempts of physical restraint will only exacerbate the situation. 4. Remain calm in talking with the person while you are trying to defuse the situation. Remember, in most crisis situations, the person is fearful and is responding to a perceived threat. Shouting at the person can cause the person to become violent if he isn’t already. Speaking calmly tends to defuse violence – the person might have to stop shouting himself so he can hear you. 5. Maintain as much physical distance as possible between the person, yourself and others. Once you have summoned help, clear the area of all bystanders who are not directly involved in trying to handle the situation. Maintain an avenue of escape for yourself and the violent person. Do not attempt to block his exit from the building. Likewise, do not let him get between you and the door, even if you have to flee to prevent it. Approaching the person too closely or touching him, even in a friendly or consoling way, will provoke violence. 6. If threats have been made to a specific identified person follow procedure under “need to Notify” 7. Once the violence crisis has passed, give yourself an opportunity to recover before going back to your regular duties. Witnessing or intervening in a violent situation provokes a strong physiological response which takes time to subside. Talk about the experience with peers and supervisors. Allow others the opportunity to be responsive to you. Talking about the episode in the staff meeting allows the opportunity for staff to consider alternative courses of action and prevention for the future. 8. Within 24 hours, an incident report needs to be made and given to Center Director. It will be reviewed by the Center Director and Medical Director who will determine whether patient should continue to receive services at the Center. The key determination of this decision will be whether the individual’s presence at the Center will constitute a threat to patients and/or staff. A decision to put a hold on services 195 will be sent to the Bureau Medical Director and final approval granted by the Bureau Director. 196 WAIVER ADDENDUM 197 Insert DHMH Letter to Dr. Fraker (8 pages) 198 PROGRAM SERVICE ANNUAL REPORTS 199 Insert Adult Department, Clinic Based Services Annual Report July 04 – June 05 Insert Adult Department, Clinic Based Services Annual Report July 05 – Dec. 05 Insert Child & Adolescent Dept. Clinic Based Services Annual Report Jan 05 – Dec. 05 200