Mother - Institute for Healthcare Improvement
advertisement

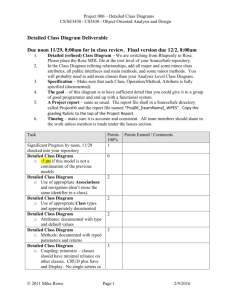
Defensibility Assessment of the Mother’s Medical Record This tool has been tested by 6 organizations. As with any tool, and as more hospitals use this tool, we will refine and update based on input from users. The findings from the use of this tool should not be considered as the final decision about the defensibility of care after an adverse event. As you know, there are many factors that may influence the defense of care. The purpose of this tool is to determine if the changes implemented as part of improving perinatal care are also improving the documentation of the care provided. The goal is to improve the defensibility of the care through appropriate documentation. Background One of the goals for the Perinatal Collaborative is to ensure the defensibility of adverse events. Reviews of medical malpractice claims report that documentation is often lacking or incomplete. Many lacked documentation of the physician's recognition of the risk factors involved.1 A review of claims from the Harvard system includes inadequate documentation of care as a contributor to inadequate identification and response to fetal distress.2 Appropriate documentation serves to ensure communication among providers and continuity of care and it can be the only history of the care that was provided. Incomplete or missing documentation makes it difficult to remember why decisions were made and particular interventions applied. Legible and complete documentation can often prevent an adverse outcome from progressing to a malpractice claim. In order to assist the perinatal teams to assess the quality of the documentation when reviewing a medical record, we have developed the following tool. The purpose of this tool is to provide reviewers with prompts that may help determine whether the documentation in the medical record supports the care delivered or is a liability. This is not all encompassing and represents general principles of loss prevention/risk management. You may add items that in your judgment are critical in your state/jurisdiction. We recommend using this tool to review any medical record, not only if there has been an adverse event. _______________________ 1Ogburn PL Jr, Julian TM, Brooker DC, Joseph MS, Butler JC, Williams PP, Anderson ML, Shepard AC, Ogburn SL, Preisler WC Jr, et al., Perinatal medical negligence closed claims from the St. Paul Company, 1980-1982. 2 http://www.rmf.harvard.edu/files/documents/Forum_V21N1.pdf Accessed June 16, 2006 How to use this tool In order to protect your findings from discovery, consider using this tool under your existing quality improvement/peer review/risk management process. We suggest that you not record the medical record number on these documents. Data should be aggregated and only aggregated data should be reported on the IHI extranet. We suggest you also have your risk manager and legal counsel review the tool prior to any data collection. We suggest that you use this tool in the same manner as you use the IHI Perinatal Trigger tool. Our suggestion is to use the same charts randomly selected for your harm review (Perinatal Trigger Tool). Use the criteria listed for each record (Mother or Infant) and determine if the expected elements of documentation are present. You will be reviewing medical records in which no harm occurred. The goal is to review adherence with desired practices of documentation in all charts. The random sampling methodology will provide a representative sample. A registered nurse from the labor and delivery area and the risk manager should review the records, discuss their findings, and then make a final decision about the defensibility of each medical record reviewed. As with the trigger tools, reviewers should not be reading the entire medical record entry by entry, page by page but rather looking in the record to see if the items listed are appropriately addressed on a consistent basis throughout the medical record. Your judgment and experience will determine if the documentation in the medical record can either assist or damage the defense of a case. In the event of serious harm, the absence of any of these elements may result in an opportunity for the plaintiff attorney to question the quality of care. Conversely, a complete and well documented medical record demonstrates the meticulous manner of patient care. We suggest a review of 20 couplet charts (total of 40) each month. Results posted onthe extranet website by the 15th of the month following the completion of the review. 1. Collect the 20 pairs of charts (20 for mother and 20 for baby). 2. Review all the charts using the elements in the enclosed tools for Mother and Infant, regardless of the trigger tool results. 3. Indicate deficiencies in documentation. 4. Determine if the documentation of the care provided is complete, legible and indicates teamwork and communication among the team. 5. Report on the extranet: (https://www.ihi.org/extranetng/projecthome.aspx?contextGUID=fdb3913c-db0f481f-9553-1ee7ed523088) a. Numerator: enter the number of records you have determined; based on your standards and review, to be defensible. b. Denominator: enter the total number of medical records reviewed. c. The extranet will then calculate the percentage of records considered defensible. For the Mother ______Yes ______Yes ______Yes ______No ______No ______No ______Yes ______No ______Yes ______No ______Yes ______No ______Yes ______No ______Yes ______No ______Yes ______No ______Yes ______No ______Yes ______No ______Yes ______No ______Yes ______No Labor and Delivery ______Yes ______No 13. Plan of care is documented. 14. Nursing and physician/midwife documentation compliments each other. 15. Mother and fetal vital signs are appropriately documented. (Frequency of the documentation is consistent with policy guidelines for fetal monitoring and epidurals and any post procedure monitoring). 16. There is documentation in the medical record by healthcare providers, during the course of the labor period, which is consistent with any hospital policies in terms of the frequency of patient checks, epidural insertion and patient monitoring, etc. These entries also contain appropriate assessment notes and the patient’s progress and any concerns by the provider. 17. There is documentation of any calls to members of the healthcare team regarding a change in maternal or fetal status. 18. There is documentation that appropriate action was taken by ______Yes ______Yes ______No ______No ______Yes ______No ______Yes ______No ______Yes ______No ______Yes ______No Documentation In General for the Whole Patient 1. All entries are dated and timed. 2. All entries are signed or initialed. (If initialed a key is available to determine the identity of the individual for each set of initials.) 3. All pages in the medical record contain the patient’s name and correct identification information 4. Unused lines or spaces have a single line through them to prevent late entries or additions to the record. 5. There is documentation that dictated notes are reviewed and signed. 6. Entries by residents either notes or dictation are co-signed by attending as required (ACGME) N/A (Not Applicable) no residents on staff _________ 7. There is no indication that the medical record has been altered and sections of the record have not been removed. 8. Entries in the medical record are legible, have not been altered nor are letters or numbers written over each other or obliterated to correct errors. 9. Abbreviations on the “Do Not Use” list are not used by employees, midwives, physicians or other healthcare providers. 10. Verbal orders are documented and authenticated within defined time frame per hospital policy. 11. Notes are documented as if a patient will read the record. (Are objective, factual and do not contain judgmental or subjective comments.) 12. If a language barrier was identified, there is documentation that steps were taken by healthcare team members to communicate on an ongoing basis with the patient and written materials provided in the patient’s preferred language. N/A Not applicable ________ nursing staff if a resident or attending did not respond to a nurse’s concern about the patient’s condition (i.e. chain of command policy was carried out). Fetal Monitoring 19. There is documentation of when the fetal monitor is applied to the laboring patient and when it is removed and or restarted. 20. Electronic fetal monitor (EFM) strips and recorded ultrasound images are retained for each patient. (EFM strips are retained per policy of the hospital and can be provided if needed.) 21. EFM documentation is consistent with hospital policy to include the frequency of patient assessments, any interventions performed, medications administered or dosages of IV medications changed, the presence of healthcare providers at the bedside, etc.) 22. Documentation of care in a spontaneous vaginal delivery is in accordance with institutional policy. (Labor and Delivery form documentation is complete.) N/A Not a Vaginal delivery ____________ 23. Indications, rationale and performance of procedures or maneuvers selected for operative vaginal delivery are documented in the medical record. N/A Not an operative vaginal delivery ___________ 24. Documentation of care in a cesarean section is in accordance with institutional policy. (Indications and procedure are documented, including the application of forceps and/or a vacuum). N/A Not a cesarean section _________ 25. For emergency situations – for example emergency c-section, documentation provides a record of what took place, when, where, and who was involved and the outcome. Decision to incision time can be determined from this documentation. N/A No emergency situations occurred ________ 26. For an emergency c-section the time from incision to decision is appropriate per hospital policy. (Should be no greater than 30 minutes or per hospital policy) N/A Not an emergency c-section _________ 26. Identification of the parent and infant is verified prior to discharge and documented in the medical record. (Identification bands may be retained, etc.) ______Yes ______No ______Yes ______No ______Yes ______No ______Yes ______No ______Yes ______No ______Yes ______No ______Yes ______No ______Yes ______No ______Yes ______No _____Yes ______No _____Yes ______No _____Yes ______No _____Yes ______No Consents 27. General treatment consent is properly signed by all parties to include date and time, etc., per the hospital form/policy. 28. Informed consent for the delivery is properly signed by all parties to include date and time, etc. If patient was unable then signature was obtained from legally responsible person. 29. Informed consent for any delivery or procedure includes information about the proposed treatment, benefits and drawbacks, alternatives, likelihood of success and problems related to recovery, prior to the procedure/treatment. Results 30. There is documentation in the medical record that critical lab/test results have been reported to the appropriate healthcare team members to include the time of notification. Education and Discharge Instructions 31. Education of the mother regarding infant care is documented in the medical record. 32. Education regarding infant care is documented in the medical record for other caregivers if applicable. N/A _____ 33. Education regarding the mother’s self care and follow-up after discharge is documented in the medical record. (Breast feeding, wound care, etc.) 34. Written discharge instructions are provided and copies are retained in the record to include acknowledgement of the instructions having been provided to the patient. Total Number of responses _____ Yes _____ No _____Yes ______No _____Yes ______No _____Yes ______No _____Yes ______No _____ N/A Is this medical record defensible from a risk management perspective? Based upon: the number of “Yes” responses, and documentation standards in your hospital ______Yes ______No