Ch 7 Liquids for Injection
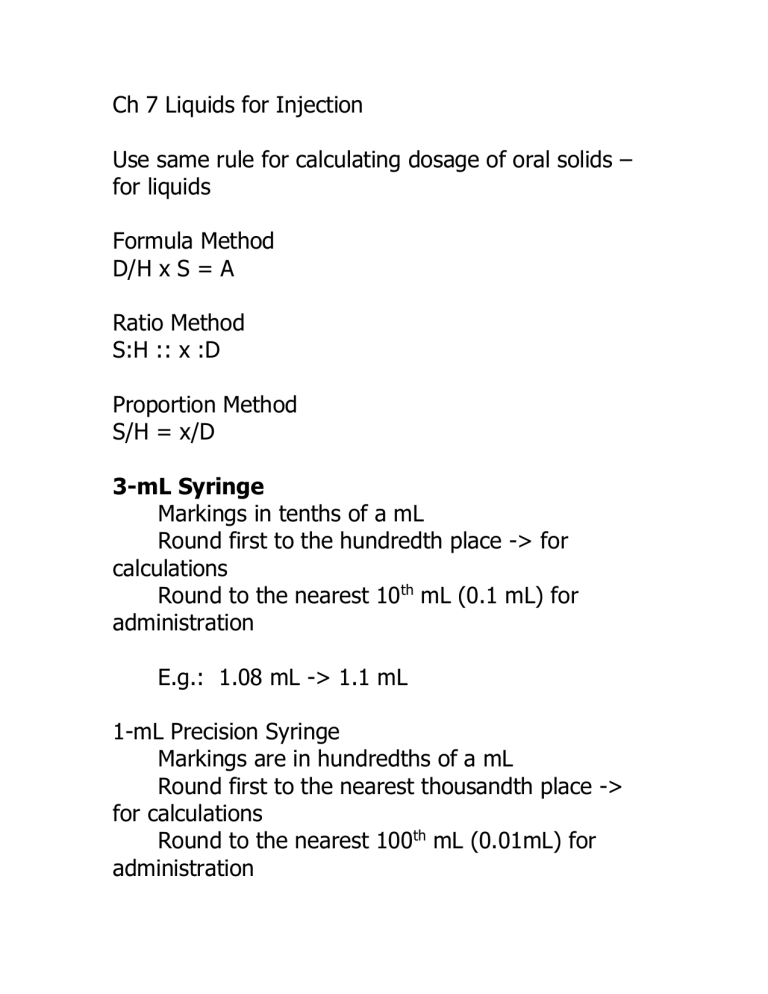
Ch 7 Liquids for Injection
Use same rule for calculating dosage of oral solids – for liquids
Formula Method
D/H x S = A
Ratio Method
S:H :: x :D
Proportion Method
S/H = x/D
3-mL Syringe
Markings in tenths of a mL
Round first to the hundredth place -> for calculations
Round to the nearest 10 th mL (0.1 mL) for administration
E.g.: 1.08 mL -> 1.1 mL
1-mL Precision Syringe
Markings are in hundredths of a mL
Round first to the nearest thousandth place -> for calculations
Round to the nearest 100 th mL (0.01mL) for administration
E.g.: 0.658 mL -> 0.66 mL
Order: Demerol HCl 75 mg IM q4th prn
Supply: read label: 50 mg/mL
D/H x S = (75 mg/50mg) x 1 mL = 1.5 mL
Use 3-mL syringe for delivery
Order: heparin sodium 1500 units subcutaneous bid
Supply: read the label: 5000 units per mL
[Note: unit represents units of biological activity]
1500 units x 1 mL = 3/10 mL = 0.3 mL
5000 units
Use 1-mL precision syringe
Order: Lanoxin 120 mcg IV every day
Supply: read the label: 0.25 mg/mL
120 mcg x 1 mL = 0.48 mL
250 mcg
Use 1-mL precision syringe
Order: furosemide (Lasix) 20 mg IV q12h
Supply: Read the label: 40mg/4mL –> 10mg/1mL
20mg x 1 mL = 2 mL
10mg
Use a 3-mL syringe
Note: IVpush (IVP) medications: have to be diluted and administered according to nursing drug book or
HOSPITAL POLICY
think about the rate of administration (mL per min)
Lasix IVP: given undiluted at a rate of 20 mg/1 minute
Order: promethazine (Phenergan) 12.5 mg IV q4-6h prn
Supply: Read the label: 25 mg/mL (single dose)
12.5 mg x 1 mL = 0.5 mL
25 mg
Promethazine IVP given undiluted if less than 25 mg.
Give each 25 mg over 1 minute
If there is no “hospital policy” a.
look it up in nursing book b.
call the physician
Special Types of Problems in Injections from a Liquid
When supply is as a Ratio
Labels may state the strength of the drug as a ratio
Ratio: grams per milliliter
1:25 -> 1 gram of drug in 25 mL
2: 45 -> 2 grams of drug in 45 mL
Ratios: 2: 1100
2 grams in 1100 mL
2 grams = 1100 mL
2 grams/1100 mL
Look at label on p. 150
1:1000 (1mg/1mL)
1:1000: 1gram per 1000 mL
Order: epinephrine 1 mg subcutaneous stat
Supply: ampule labeled 1: 1000
1mg x 1000 mL = 1 mL
1000mg mg – solid
mL – liquid
Order: isoproterenol HC 0.2 mg IM stat
Supply: ampule labeled as 1: 5000 -> 1 g per 5000 mL
Solution: 1000mg/5000mL
0.2mg x 5000 mL = 1 mL
1000mg
See p. 92 for needle length
When supply is a Percent
Lidocaine 2% (2 g in 100mL)
2 g per 100 mL
2 g = 100mL
2g/100 mL e.g. 30 %
30 g per 100 mL
30 g/100 mL e.g. 0.33%
.33 g per 100 mL e.g. 0.002%
0.002 g per 100 mL
1% -> 1 g per 100 mL
Order: lidocaine 30 mg for injection before suturing wound
Supply: read the label
2% -> 2 g per 100 mL
20 mg/mL
30 mg x 1 mL = 1. 5mL
20 mg
Use 3 mL syringe
Order: magnesium sulfate 1 g; add to IV stat
Supply: read the label
50% -> 50 g per 100 mL (1 g per 2 mL)
(4.06 mEq/mL Magnesium)
1 g x 100 mL = 2 mL
50 g
1g x 2 mL = 2mL
1 g
Insulin Injections
Insulin – hormone secreted by the pancreas
Given in units
Rapid-Acting Insulin – act within 1 hour; peak in 2 to
4 hours; via IV Sub-Q
Humulin R
Humalog – unique, rapid acting insulin – newest insulin made via recombinant DNA technology; lowers blood sugar but much more rapidly; acts within 5 minutes after injection, peaks in 1 hour/ lasts 2 to 4 hours
Lantus Insulin – not to be mixed with other insulins
Onset is 1 hr, no peak, lasts 24 hrs (like normal insulin)
[sliding scale??]
Intermediate-Acting Insulin: begin action in 1 to 3 hours, peak 6 to 12 hours, may last 24 hrs; labeled N
(or isophane) to L (zinc and protamine suspension)
Delay absorption/prolong time of action
NPH N: solution is neutral (pH = 7)
P: protamine content
H: Hagedorn lab (credited with creating this insulin type)
Long-Acting Insulins: modified with addition of zinc and protamine; 4 to 8 hours to act; 12 to 20 hrs to peak; can last up to 36 hr
Humulin U or Ultralente
Mixed Insulins: can get order that may require two insulin types to be mixed in 1 syringe and administered together
Humulin 70/30 : 70 % insulin
High-Potency Insulins: 500 units/1mL: for patients who need large doses and for emergency situations –
STORE these high-potency insulins AWAY from usual 100units/mL insulins http://www.clevelandclinic.org/health/healthinfo/docs/3300/3376.asp?index=11452
Never shake the vial; rather: rotate the vial to assure
“mixing”
Types of Insulin Syringes
50 units: Low Dose
100 units: 1 mL syringe: each line = 2 units
Mixing Two Insulins in One Syringe
2 facts:
1. regular insulin is always drawn up first into the syringe (Clear)
2. total number of units in the syringe will be the addition of the two insulin orders
Regular insulin often ordered with NPH insulin
“Clear to Cloudy” – which insulin is drawn up first.
Steps to prepare two insulins in one syringe
1.
inject amount of air equal to amount of NPH insulin into the NPH vial
2.
inject the amount of air equal to the amount of regular insulin into the regular vial
3.
withdraw the correct amount of regular insulin
(“clear”)
4.
withdraw the correct amount of NPH insulin
(“cloudy”)
5.
total number of units = units of reg. ins + units of NPH
Use alcohol wipes to clean top of the vial and patient’s skin target for injection
Injections from Powders
Powders (more stable) - > reconstitute as liquids -> unstable and can lose their potency/activity over time
Pharmacist usually responsible for reconstituting medications. But it may be nurse’s responsibility.
Reconstituted drugs may be delivered via a special reconstitution device.
Once powdered drug becomes a liquid, then calculations are same as for oral solids and liquids and for injection of a liquid
E.g.
Order: cefonicid sodium 0.65 g IM every day
Supply: read the label
Add 2.5 sterile water for injection. Shake well. Volume now 3.1 mL (325 mg/mL)
Supply: 1 mL reconstituted
D = 0.65 g = 650 mg
650 mg x 1 mL = 2 mL
325 mg
Use 3-mL syringe
Label vial with date, time, solution that was made
(e.g., 325/mL0, nurse’s initials
Store in refrigerator at 5 degrees C
Distinctive features of injections from Powders
Need to use Sterile technique to prepare and administer medications: given parenterally (IM, IV,
IVPB).
Choose strength closest to the amount ordered.
Powder is usually diluted with one of following:
-Sterile water for injection
-Bacteriostatic water for injection with a preservative added
-Normal saline for injection (0.9% sodium chloride)
Directions: will state which fluids may be used.
Read directions/information as some fluids may be incompatible as diluents
Steps to Reconstitute Powders with Directions
1.
Read the order
2.
Identify the supply (original form: powder in vial/ampule)
3.
Dilute the fluid
4.
Identify the solution and the new supply
(new form for administration: liquid -> mL)
5.
Apply the rule and arithmetic
6.
Obtain the amount to give
E.g.,
7.
Write on the label
8.
Store according to directions
Order: cefoperazone 0.5 g IM q12h
Supply: 1-g vial of powder
Step 6: to make 250 mg/mL, following added: 2.8 mL sterile water and 1.0 mL 2% lidocaine
New supply 250mg/mL
D 0.5 g -> 500 mg
500 mg x 1 mL = 2 mL
250 mg
Where to find info about reconstitution of Powders
-label on vial of powder
-package insert that comes with vial of powder
-nursing handbooks
-PDR
Order cefazolin sodium 0.3 g IM
Supply: 500 mg powder
Diluting fluid: 2.0 mL sterile water for injection
Solution and new supply: 225 mg/mL
D: 0.3 g = 300 mg
300 mg x 1 mL = 1.33 mL
225 mg
Use 3 mL syringe and round to 1.3 (nearest .1)
Write on label: 225/mL, 09/27/07, 1320, KP
Storage: refrigerate; stable for 96 hr
Order: penicillin G potassium 1 million units IM q6h
Supply: 5 million-unit vial
Diluting fluid and number of mL: use sterile water for injection. We chose 3 mL as will give 1000000 units/mL
1 million units x 1 mL = 1 mL
1 million units
Give 1 mL Im
Write on label: 1 million units/mL, date, time, KP
Storage: refrigerate; stable for 1 week
Note: solution is “so concentrated” that it may be/will be painful for the patient – so dilute the amount to be administered
Do the CRITICAL THINKING as well as the proficiency tests!