MHC
advertisement
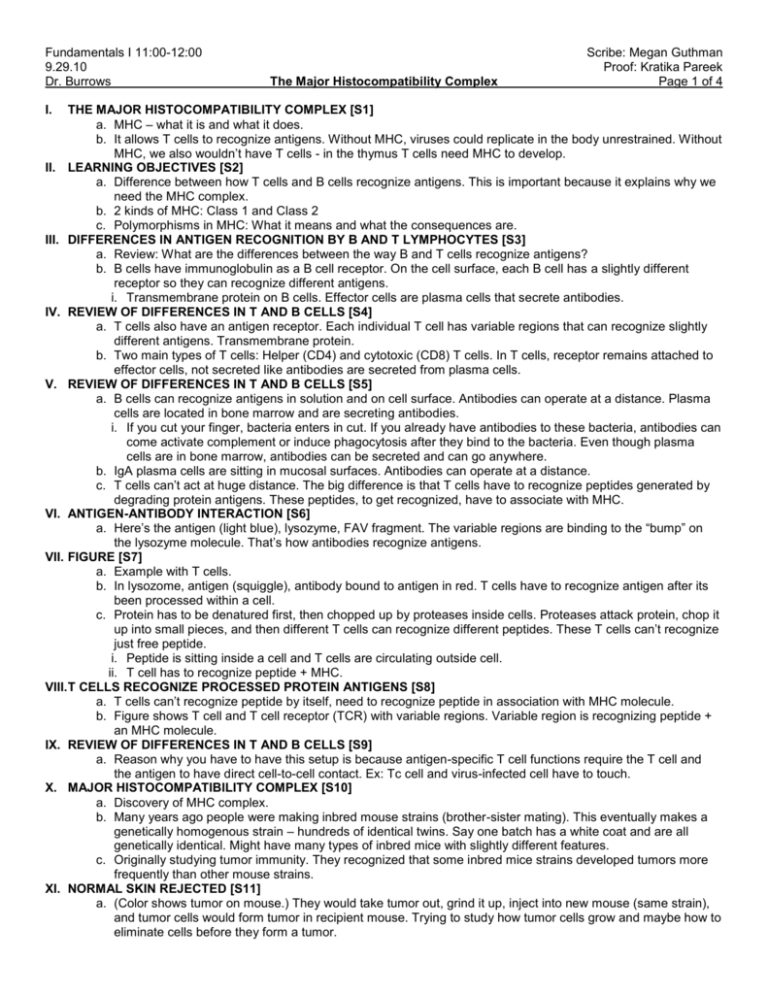
Fundamentals I 11:00-12:00 9.29.10 Dr. Burrows I. The Major Histocompatibility Complex Scribe: Megan Guthman Proof: Kratika Pareek Page 1 of 4 THE MAJOR HISTOCOMPATIBILITY COMPLEX [S1] a. MHC – what it is and what it does. b. It allows T cells to recognize antigens. Without MHC, viruses could replicate in the body unrestrained. Without MHC, we also wouldn’t have T cells - in the thymus T cells need MHC to develop. II. LEARNING OBJECTIVES [S2] a. Difference between how T cells and B cells recognize antigens. This is important because it explains why we need the MHC complex. b. 2 kinds of MHC: Class 1 and Class 2 c. Polymorphisms in MHC: What it means and what the consequences are. III. DIFFERENCES IN ANTIGEN RECOGNITION BY B AND T LYMPHOCYTES [S3] a. Review: What are the differences between the way B and T cells recognize antigens? b. B cells have immunoglobulin as a B cell receptor. On the cell surface, each B cell has a slightly different receptor so they can recognize different antigens. i. Transmembrane protein on B cells. Effector cells are plasma cells that secrete antibodies. IV. REVIEW OF DIFFERENCES IN T AND B CELLS [S4] a. T cells also have an antigen receptor. Each individual T cell has variable regions that can recognize slightly different antigens. Transmembrane protein. b. Two main types of T cells: Helper (CD4) and cytotoxic (CD8) T cells. In T cells, receptor remains attached to effector cells, not secreted like antibodies are secreted from plasma cells. V. REVIEW OF DIFFERENCES IN T AND B CELLS [S5] a. B cells can recognize antigens in solution and on cell surface. Antibodies can operate at a distance. Plasma cells are located in bone marrow and are secreting antibodies. i. If you cut your finger, bacteria enters in cut. If you already have antibodies to these bacteria, antibodies can come activate complement or induce phagocytosis after they bind to the bacteria. Even though plasma cells are in bone marrow, antibodies can be secreted and can go anywhere. b. IgA plasma cells are sitting in mucosal surfaces. Antibodies can operate at a distance. c. T cells can’t act at huge distance. The big difference is that T cells have to recognize peptides generated by degrading protein antigens. These peptides, to get recognized, have to associate with MHC. VI. ANTIGEN-ANTIBODY INTERACTION [S6] a. Here’s the antigen (light blue), lysozyme, FAV fragment. The variable regions are binding to the “bump” on the lysozyme molecule. That’s how antibodies recognize antigens. VII. FIGURE [S7] a. Example with T cells. b. In lysozome, antigen (squiggle), antibody bound to antigen in red. T cells have to recognize antigen after its been processed within a cell. c. Protein has to be denatured first, then chopped up by proteases inside cells. Proteases attack protein, chop it up into small pieces, and then different T cells can recognize different peptides. These T cells can’t recognize just free peptide. i. Peptide is sitting inside a cell and T cells are circulating outside cell. ii. T cell has to recognize peptide + MHC. VIII. T CELLS RECOGNIZE PROCESSED PROTEIN ANTIGENS [S8] a. T cells can’t recognize peptide by itself, need to recognize peptide in association with MHC molecule. b. Figure shows T cell and T cell receptor (TCR) with variable regions. Variable region is recognizing peptide + an MHC molecule. IX. REVIEW OF DIFFERENCES IN T AND B CELLS [S9] a. Reason why you have to have this setup is because antigen-specific T cell functions require the T cell and the antigen to have direct cell-to-cell contact. Ex: Tc cell and virus-infected cell have to touch. X. MAJOR HISTOCOMPATIBILITY COMPLEX [S10] a. Discovery of MHC complex. b. Many years ago people were making inbred mouse strains (brother-sister mating). This eventually makes a genetically homogenous strain – hundreds of identical twins. Say one batch has a white coat and are all genetically identical. Might have many types of inbred mice with slightly different features. c. Originally studying tumor immunity. They recognized that some inbred mice strains developed tumors more frequently than other mouse strains. XI. NORMAL SKIN REJECTED [S11] a. (Color shows tumor on mouse.) They would take tumor out, grind it up, inject into new mouse (same strain), and tumor cells would form tumor in recipient mouse. Trying to study how tumor cells grow and maybe how to eliminate cells before they form a tumor. Fundamentals I 11:00-12:00 Scribe: Megan Guthman 9.29.10 Proof: Kratika Pareek Dr. Burrows The Major Histocompatibility Complex Page 2 of 4 b. What about transplanting tumor into different inbred mouse strain? Tumor into different mouse strain, and the tumor was rejected (other strain = Mickey). Second mouse is resistant to tumors? No. Did the control study – took skin from mouse (white) and transplanted it to the other mouse (Mickey), and normal skin was rejected. Not tumor immunity but transplantation immunity. XII. MAJOR HISTOCOMPATIBILITY COMPLEX [S12] a. MHC – histocompatibility = tissue compatibility. Transplantation between different individuals. It’s the major one that has to be matched to prevent organ transplant rejection. b. Called a complex because several genes are closely associated that makes up MHC. c. Causes a powerful immune response to foreign tissues – we didn’t evolve MHC to prevent tissue transplantation. Why do we have it? Normal function of MHC is to display peptide antigens (both self and non-self antigens) to T cells. XIII. MHC [S13] a. MHC1 and 2 - Similarities and differences, structure, genes, and polymorphisms. XIV. MHC CLASS I [S14] a. MHC Class 1: i. Proteins Expressed by all nucleated cells – everything in body but RBC’s. ii. MHC Class 1’s job is to present peptide antigen to CD8 T cells. CD8 T cells’ main function is to become cytotoxic/killer T cells. Can kill virus infected cells and incipient tumor cells. b. That’s what’s shown here in the time lapse strip: the killing of a virus infected cell by a Tc cell. Small cell (with red dot) is T cell, bigger cell is infected with virus. i. Cell has virus replicating inside it. Viral proteins are being produced, viral peptides are being associated with MHC Class 1 and are expressed on cell surface. ii. T cell recognizes viral protein + MHC as foreign antigen, and now will kill the cell. Red inside T cell is what it uses to kill target cells. It binds to target, and it eventually blows up target cell. Kills virus infected cell. c. After it kills, nothing happens to T cell. Can go around and kill more of these cells to help clear the virus infection. d. MHC1 is on all nucleated cells. Involved in antigen presentation to CD8 cytotoxic T cells. XV. FIGURE [S15] XVI. FIGURE: CD8 T CELL AND VIRUS INFECTED CELL [S16] XVII. MHC CLASS II [S17] a. Class 2 is more restricted in the kind of cells that express it. Expressed by antigen presenting cells (dendritic cells, macrophages). b. Class 2 molecules present peptides to helper (CD4) T cells. Helper T cells can help B cells do everything we previously talked about: proliferate, differentiate, isotype switching - all of that is through the help of helper T cells. Help primarily from cytokines. c. Can also activate macrophage to kill intracellular pathogens. Macrophages can be infected, for example, with tuberculosis – an intracellular parasite. They have a hard time getting rid of it. Stimulated by helper T cells, macrophages then can kill intracellular pathogen. XVIII. CD4 T CELL HELPING A B CELL [S18] a. This is a helper T cell helping a B cell. b. B cell (yellow) has a peptide antigen on an MHC Class 2. Helper T cell is blue. i. Helper T cell recognizes peptide + MHC and gives B cell help. ii. (2nd frame) Forms close contact between T and B cell. T cell is secreting IL-4 (a cytokine). Look at green – labeled IL-4 – just in little pocket formed between T cell and B cell. Expose B cell to high concentration of IL-4 at point of contact between T cell and B cell. T cell only secreting it right into small area of contact. IL-4 is cytokine that induces isotype switching. c. Antigen specific response – B cell has to recognize antigen, T cell has to see same antigen in form of peptide. On yellow cell (B cell) – recognizes antigen by B cell receptor, internalizes it, and expresses as MHC class 2 on the surface as a peptide. XIX. FIGURE: CD4 T CELL AND ANTIGEN PRESENTING CELL [S19] XX. FIGURE [S20] a. Here we have our B cell – it has class 1 MHC because it’s nucleated. Since it’s an antigen presenting cell, it will also expresses class 2. b. Normally, proteins on cell surface have peptide in them. With no infection, peptide is self-antigen peptide (green). B cell is sitting in a lymph node expressing class 1 and 2 with self peptides attached. c. Assume the correct antigen for the particular B cell binds to the receptor, the complex is brought inside cell. Lysozyme denatures and chops protein into small peptides. Class 2 molecules are turning over (making new, getting rid of old), they pick up that peptide and display it on the cell surface. d. Now B cell has foreign peptide in its class 2. Peptide derived from original antigen that B cell recognized. Fundamentals I 11:00-12:00 Scribe: Megan Guthman 9.29.10 Proof: Kratika Pareek Dr. Burrows The Major Histocompatibility Complex Page 3 of 4 XXI. FIGURE [S21] a. Here (left) is a B cell with foreign antigen peptide (red). And another B cell (right) that has a different B cell receptor, sitting with self peptides. b. T cells are always circulating checking out all the MHC class 1 and 2 molecules, depending if the T cell is CD4 or CD8. T cell looks at B cell on right, it has self peptides so nothing happens. c. On left B cell, T cell has T cell receptor that recognizes that specific foreign peptide with class 2. Activates the B cell, starts secreting cytokines, etc. Makes a B cell-specific antigen response. XXII. FIGURE [S22] a. The B cell recognizes antigen by its B cell receptor, then displays peptide from that antigen to helper T cell. That’s how you get antigen-specific help for B cells. b. Middle frame - get proliferation, differentiation into plasma cells. B cell grabs antigen and makes a peptide. c. Question on clarification of self peptides: B cell has several thousand MHC Class 2, has mostly self peptide bound, only a few with foreign peptide. Only need a couple of foreign peptides to activate T cell, system is very sensitive. XXIII. MHC [S23] a. A structural look at class 1 and class 2 molecules. Similar. b. Class 2 (left) – 2 proteins: alpha and beta chain. c. Class 1 (right) has a bigger alpha chain and small molecule called beta-2-microglobulin that associates with it. d. MHC there to bind peptides. Look where arrows are pointing – it’s a good place to stick a peptide. XXIV. CLASS I AND CLASS II MHC MOLECULES [S24] a. MHC’s are membrane bound glycoproteins. b. They look similar. c. Each have four domains: membrane proximal and distal. Distal domains are involved in peptide binding -form peptide binding cleft XXV. 3D STRUCTURE OF HUMAN CLASS I HLA MOLECULE [S25] a. 3D crystal structure of human class 1. Alpha1, alpha2 and alpha3 domains and a small beta-2-microglobulin molecule. Region at top forms peptide binding cleft. XXVI. FIGURE [S26] a. Top-on view of peptide binding cleft, looks like a good place to drop a peptide. Top of MHC class 1 is open, can lay a peptide in there, then it is expressed on cell surface, and that’s what the T cell is going around looking at. XXVII. PEPTIDES IN THE MHC GROOVE [S27] a. Another picture of same idea. Class 1 MHC with alpha 2 and 3 domains (white), peptide sitting in there. CD8 T cells can recognize class 1 + peptide. T cells are busy circulating, looking for whether or not there’s a foreign peptide in the groove. b. Class 2 MHC on right, looks similar but peptides can drape out of the end. c. Class 1 is hot dog bun and hot dog, buns sealed at end. Class 2 hot dog droops over ends of bun. d. CD4 T cells also circulating around. They have less cells to look at – CD4 T cells looking at antigen presenting cells that have class 2 + peptide, see if they have a foreign peptide in there. immune surveillance. XXVIII. THE HUMAN MHC GENE COMPLEX [S28] a. Genes are simple for MHC – no rearrangement or recombination. b. Figure is human MHC: HLA (human leukocyte antigen). i. There’s 3 class 1 genes called A, B, and C (blue). Class 1 has alpha chain with 3 domains that hooks up with beta-2-microglobulin to make the class 1 molecule. A given cell with class 1 MHC has 3 different class 1 molecules – A, B, and C. ii. There’s 3 sets of class 2 genes. Remember class 2 has an alpha and beta chain. In humans called DP, DQ, and DR. c. This shows one chromosome but remember we have 2 – one maternal and one paternal. A given cell (any cell with a nucleus) is expressing class 1 – have A, B, and C class 1 from maternal chromosome and A, B, and C class 1 from paternal chromosome. 6 different class 1’s, and each can bind to slightly different peptides. This is good, gives a lot of peptides you can display to T cells. d. Same with class 2 – if cell expresses class 2, it expresses DP, DQ, and DR from two chromosomes. e. The idea is to maximize the ability to bind to different peptides so you can protect yourself from different pathogens. XXIX. MHC POLYMORPHISMS [S29] Fundamentals I 11:00-12:00 Scribe: Megan Guthman 9.29.10 Proof: Kratika Pareek Dr. Burrows The Major Histocompatibility Complex Page 4 of 4 a. Polymorphisms are allelic variations in the MHC genes. What that means is if you take DNA from everyone in the room and sequence class 1 and 2 genes, there’s slight differences between all of us (unless you’re identical twins). Everyone has a slightly different class 1 and 2 gene sequence and protein sequence. b. Not like each B cell being different in variable region. Within a given individual, all MHC class 1 and 2 genes are identical. Comparing individuals, MHC class 1 and 2 genes will be slightly different. XXX. MHC POLYMORPHISMS [S30] a. Shows allelic variation in MHC genes. Variation is concentrated in the region of the molecule that actually binds peptide. b. Graph looks at specific residue and how much variability is seen – makes peaks. Look at structure of MHC molecule and color red where most variable parts are. Sequence MHC’s from everyone in the room and look at variability. The part of molecule that binds peptide is where the variability is located. This allows for different MHC alleles to bind different peptides. XXXI. MHC POLYMORPHISMS [S31] a. This is important at a population level. We all have different MHC. Virus comes in that can only bind particular MHC proteins. 50% might die because we lack MHC that can bind that virus. Other 50% would live. Helps us at a population level. Polymorphisms allow huge diversity in terms of peptide binding. b. Remember: no gene rearrangements in individuals! XXXII. CONSEQUENCES OF MHC POLYMORPHISM [S32] a. The result of these polymorphisms – organ and tissue transplants are difficult. Each one of us has a different MHC. T cells see difference in MHC as foreign and they go crazy and reject organ. Because of polymorphisms, you can’t randomly transplant tissues and organs from one person to another. b. Polymorphisms change peptide binding specificity of MHC. As a population, we can survive attack by many different pathogens. c. What’s the most common tissue transplanted? Blood – just have to match ABO, not nucleated so you don’t have to worry about this. If RBC’s were nucleated, it would be more difficult to do a blood transfusion. d. Hard to match people but there’s still a high number of transplants. How? With immunosuppressant drugs. Has nothing to do with matching organs between people. Give cyclosporine or other powerful immunosuppressant that tampers down T cell response and allows the organ not to be rejected. XXXIII. WHY HAVE TWO ANTIGEN RECOGNITION SEQUENCES? [S33] a. Why do we need two? B cells and T cells to protect us against pathogens. b. Yellow is virus, virus has to get inside cells and replicate, escape, infect more cells, creates massive viral infection. To get rid of this, antibodies neutralize the virus, prevent it from infecting other viruses. c. Still have infected cells. Role of cytotoxic T cells: come in and eliminate the source of virus production= sterilizing immunity. Helper T cells helping to make antibodies. That’s why we need both T cell and B cell antigen recognition system. d. Important to get sterilizing immunity, particularly to viral infection. [End 40:15 mins]