ACUTE PANCREATITIS - Austin Community College
advertisement

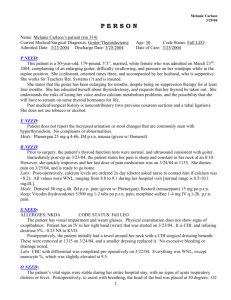
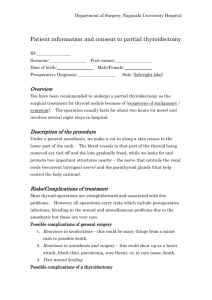
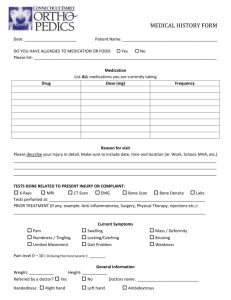
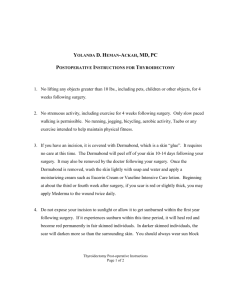
Melanie Carlson 3/29/04 PERSON Name: Melanie Carlson’s patient (rm 314) Current Medical/Surgical Diagnosis: Goiter/Thyroidectomy Admitted Date: 3/23/2004 Discharge Date: 3/25/2004 Age: 50 Code Status: Full LEO Date of Care: 3/25/2004 P NEED: This patient is a 50-year-old, 179-pound, 5’3”, married, white female who was admitted on March 23rd, 2004, complaining of an enlarging goiter, difficulty swallowing, and pressure on her windpipe while in the supine position. She is pleasant, oriented times three, and accompanied by her husband, who is supportive. She works for Teachers Ret. Systems (?) and is insured. She states that the goiter has been enlarging for months, despite being on suppression therapy for at least four months. She has educated herself about thyroidectomy, and requests that her thyroid be taken out. She understands the risks of losing her voice and/or calcium metabolism problems, and the possibility that she will have to remain on some thyroid hormones for life. Past medical/surgical history is noncontributory (two previous cesarean sections and a tubal ligation). She does not use tobacco or alcohol. E NEED: Patient does not report the increased urination or stool changes that are commonly seen with hyperthyroidism. No complaints or abnormalities. Meds: Phenergan 25 mg q.4-6h. IM p.r.n. nausea (given w/ Demerol) R NEED: Prior to surgery, the patient’s thyroid function tests were normal, and ultrasound consistent with goiter. Immediately post-op on 3/23/04, the patient states her pain is sharp and constant in her neck at an 8/10. However, she quickly improves and her last dose of pain medication was on 3/24/04 at 1135. She denies pain on 3/25/04, and is ready to go home. Labs: Post-operatively, calcium levels are ordered 2x day (doctor asked nurse to contact him if calcium was <8.2). All values were WNL, ranging from 8.8 to 9.1 during her hospital visit [normal range is 8.5-10.1 mg/dL]. Meds: Demerol 50 mg q.4h. IM p.r.n. pain (given w/ Phenergan); Restoril (temazepam) 15 mg po p.r.n. sleep; Vicodin (hydrocodone) 5/500 mg 1-2 tabs po p.r.n. pain; morphine sulfate 1-4 mg IV q.1-2h. p.r.n. pain. S NEED: ALLERGIES: NKDA CODE STATUS: Full LEO The patient has visual impairment and wears glasses. Physical examination does not show signs of exopthalmos. Patient has an IV in her right hand (wrist) that was started on 3/23/04. It is CDI, and infusing dextrose 5% - 0.25 NS to KVO. Postoperatively, the patient initially had a towel around her neck with a CDI surgical dressing beneath. These were removed at 1315 on 3/24/04, and a smaller dressing replaced it. No excessive bleeding or drainage noted. Labs: CBC with differential was completed pre-operatively on 3/22/04. Everything was WNL, except monocyte %, which was slightly elevated at 9.5. O NEED: The patient’s vital signs were stable during her entire hospital stay, with no signs of acute respiratory distress or fever. Postoperatively, to assist with breathing, the head of the bed was placed at 30 degrees. O2 1 was administered at 3 lpm via nasal cannula for the first 24 hours after surgery, but discontinued on 3/24/04. She was ambulatory on post-op day #1, and able to go to the bathroom without assistance. Labs: O2 saturation remained stable even when O2 supply via nasal cannula was removed. N NEED: No recent weight loss. Appetite is normal. Pre-op physical exam does show marked enlargement of both lobes of the thyroid, indicating a goiter. Preoperatively, the patient complains of compression symptoms associated with this goiter, especially difficulty swallowing. She prefers to drink liquids instead of eating solid foods. Immediately postoperative, the patient continues to complain of some difficulty and pain with swallowing. She chooses to remain on a liquid diet, although she is free to advance to regular diet when she feels comfortable enough to do so. Intake & output are stable and as expected. Before discharge on 3/25/04, the patient is tolerating a soft diet without difficulty. -------------------------------------------------------------------------------------------------------------------------------------- LIST OF APPLICABLE NURSING DIAGNOSES 1. Airway clearance, risk for ineffective related to tracheal obstruction secondary to swelling, bleeding or laryngeal spasms 2. Knowledge, deficient related to prognosis, treatment, self-care and discharge needs 3. Communication, impaired verbal related to tissue edema and pain/discomfort 4. Injury, Risk for (tetany) related to chemical imbalance 5. Pain, acute related to surgical interruption/manipulation of tissues/muscles 6. Disturbed sensory perception related to visual impairment without glasses MEDICATIONS Name: Vicodin (hydrocodone bitartrate) Dosage: 5/500 mg 1-2 tabs Classification: CNS agent, Narcotic (opiate) agonist analgesic, antitussive Action: CNS depressant with moderate to severe relief of pain; morphine derivative similar to codeine. Indication: Patient is post-op thyroidectomy with mild to moderate pain at the surgical site. Side Effects: Respiratory depression, constipation, nausea, drowsiness Nursing Considerations: It is important to assess a patient for respiratory difficulties when administering Vicodin after a thyroidectomy. Complications after thyroidectomy can include edema of the glottis; this complication added to the possible respiratory depression from Vicodin could be potentially harmful. Name: Restoril (temazepam) Dose: 7.5 mg po p.r.n. sleep Classification: CNS agent, anxiolytic, sedative-hypnotic, benzodiazepine Action: Relieves insomnia associated with frequent nocturnal awakenings or early morning awakenings. Benzodiazepine derivative with principal effect of significant improvement in sleep parameters. Indication: Patients may have anxiety and/or insomnia associated with a surgery and the resulting pain. Side Effects: drowsiness, dizziness, lethargy Nursing Considerations: Assess patient for paradoxical reactions (excitement, hyperactivity or disorientation) or dreams/nightmares that interfere with rest. Teach patient that medication will not improve sleep time until after 2-3 doses of drug, and that difficulty getting to sleep may continue because medication just helps increase amount of rest once asleep. 2 THYROIDECTOMY (secondary to goiter) Lemone p. 449, 459 Doenges p. 414-419 Ulrich p. 771-776 Thyroidectomy, although rare, may be performed for patients with thyroid cancer, hyperthyroidism, and drug reactions to antithyroid agents; pregnant women who cannot be managed with drugs; patients who do not want radiation therapy; or patients with large goiters who do not respond to antithyroid drugs. Patients with enlarged thyroid glands may have pressure on their esophagus or trachea that causes swallowing and/or breathing problems. Total thyroidectomy is when the gland is removed completely; usually done in the case of malignancy; and thyroid replacement is necessary for life. Subtotal thyroidectomy is up to 90% of the gland removed when antithyroid drugs do not correct hyperthyroidism or RAI therapy is contraindicated. It is the preferred procedure because the remaining gland tissue usually hypertrophies and eventually supplies adequate amounts of thyroid hormone. Prior to surgery, the patient is usually given antithyroid agents for 6-8 weeks to achieve a euthyroid state and minimize the risk of a thyrotoxic crisis. Risk Factors for thyroidectomy are either colloid goiter, tumors or hyperthyroidism that does not respond to iodine therapy and antithyroid drugs. Clinical Manifestations: Hoarseness for at least a few days; difficulty moving neck in any way; pain or difficulty swallowing; surgical incision pain; and increased secretions from irritation of the respiratory tract are all normal postoperative manifestations. If calcium metabolism is interrupted and hypocalcemia occurs, paresthesias in the lips, hands & toes and muscle twitching & spasms (tetany) can be very serious. Potential complications of thyroidectomy are (1) hemorrhage due to surgery in a highly vascular area; (2) respiratory distress due to airway obstruction (tracheal compression or closure of glottis from laryngeal nerve damage); (3) hypocalcemia due to damage of parathyroid glands during surgery; (4) thyroid storm (thyrotoxic crisis) due to excessive amounts of thyroid hormone in blood; and (5) laryngeal nerve damage due to trauma during surgery or pressure from swelling after surgery. Diagnostic Studies: Most of these are done preoperatively to help determine the cause of hyperthyroidism and to differentiate between Graves’ disease and Plummer’s disease. Thyroid function tests Serum calcium (post-op), glucose and catecholamines Ultrasound or thyroid scan Needle or open biopsy Protein-bound iodine: Increased. Urine creatitine: Increased. Liver function tests: Abnormal. Electrolytes (hyponatremia and hypokalemia often occur with hyperthyroidism) 3 Nursing Dx & Support Data Airway clearance, risk for ineffective related to tracheal obstruction secondary to swelling, bleeding or laryngeal spasms Support Data Compression symptoms before surgery (diff. breathing in supine position) Thyroidectomy performed on 3/23/04 Potential complications of thyroidectomy can all quickly lead to airway obstruction (see list in Medical Diagnosis) Goal/Outcome & Outcome Attainment 1) Maintain patent airway, with aspiration prevented. Nursing Interventions Scientific Rationale 1a) Monitor respiratory rate, depth and work or breathing. 1a) Respirations may remain somewhat rapid, but development of resp. distress is indicative of tracheal compression from edema or hemorrhage. 1b) Rhonchi may indicate airway obstruction or accumulation of copious thick secretions. 1c) May indicate edema/sequestered bleeding in tissues surrounding operative site. Outcome Attainment Patient was on oxygen for 24 hours post-op. She had no difficulties during or after O2 therapy was discontinued, and no signs of distress were ever noted in chart. 1b) Auscultate breath sounds, noting presence of rhonchi. 1c) Investigate reports of difficulty swallowing, drooling of oral secretions. 1d) Assist w/ repositioning, deep breathing exercises, and/or coughing if needed. 1e) Check dressing frequently, esp. posterior position. 1d) Maintains clear airway & ventilation. “Routine” coughing is not encouraged & is painful, it may be needed to clear secretions. 1e) If bleeding occurs, anterior dressing may appear dry because blood pools dependently. 4 Evaluation 1a) Patient’s VS were monitored q.4h. Patient was given strict instructions to call nurse using call light if any problems breathing, and patient was monitored frequently for resp. distress. No signs of difficulty were ever noted in chart. 1b) On 2nd post-op day, normal breath sounds noted. No abnormal breath sounds charted on previous days. 1c) Patient did complain of difficulty swallowing, but stated difficulty was due mainly to pain & discomfort, not swelling or compression. 1d) Head of patient’s bed was in Semi-Fowler position during her entire hospital stay (pre- and post-op). She did not have excessive secretions, but was taught to deep breath and how to support her head when moving in bed or when getting up to the bathroom. 1e) When I arrived at the hospital on Wed., the dressing had just been changed 2 hours before by the doctor, with no abnormalities or concerns noted or related to the nurse at that time. Nursing Dx & Support Data Knowledge, deficient related to prognosis, treatment, self-care and discharge needs Support Data patient is informed about surgery itself, but needs information about care for incision, prognosis, and prescribed home meds patient does not know signs/symptoms of increased/decreased thyroid hormone, and when to report to doctor need to teach patient signs of infection and other complications Goal/Outcome & Outcome Attainment 1) Patient will verbalize understanding of surgical procedure & prognosis & potential complications. Outcome Attainment Patient was very educated about her condition, the surgical procedure, and easily understood the signs/symptoms of the various complications. 2) Patient will verbalize understanding of therapeutic needs and participate in treatment regimen. Outcome Attainment Patient was planning to fill her prescriptions on her way home from the hospital with her husband. She agreed to followup with her doctor in one week. She expected no problems with incisional care. Nursing Interventions Scientific Rationale 1a) Review surgical proc. & future expectations. 1a) Provides knowledge base from which patient can make informed decisions before surgery. 1b) Discuss possibility of change in voice. 1b) Alteration in vocal cord function may cause changes in pitch and quality of voice, which may be temporary or permanent. 1c) Identify signs/symptoms requiring medical evaluation, including fever, chills, purulent or excessive wound drainage, erythema, sudden weight loss, heat or cold intolerance, N/V, diarrhea, insomnia, weight gain, fatigue, constipation or drowsiness. 2a) Review drug therapy and necessity of continuing even when feeling well. 1c) Early recognition of developing complications such as infection, hyper- or hypothyroidism may prevent progression to lifethreatening situation. 2b) Instruct in incisional care, including cleansing and dressing application. 2a) Patient needs to understand rationale for replacement therapy and consequences of failure to routinely take medications. 2b) Enables patient to provide competent self-care. 2c) Instruct patient to follow up with doctor. 2c) Provides opportunity for evaluating effectiveness of therapy and prevention of complications 2d) Review post-op exercises to be instituted after incision heals, e.g. flexion, extension, rotation, and lateral movement of head & neck. 2d) Regular ROM exercises strengthen neck muscles, enhance circulation and healing process. 5 Evaluation 1a) Patient had full understanding of the surgical procedure and the risks involved. She signed the forms, permitting the surgeon to proceed. 1b) Patient was told to contact the doctor with worsening hoarseness or if no improvement in 3-5 days. Patient understood the risks of voice alteration before proceeding with surgery. 1c) Patient verbalizes signs/symptoms of infection. She also verbalizes understanding of the signs/symptoms of low or high thyroid hormone. She was sent home with papers describing all of these symptoms. 2a) Patient verbalized understanding of prescribed meds (Synthroid & Vicodin), and understands the importance of taking the Synthroid as prescribed. 2b) Patient was instructed not to soak the incision and to use soap and warm water to clean. Patient verbalized understanding of keeping the area clean & dry. 2c) Patient understands the necessity of following up with her doctor in one week and agrees to make the appointment. The Synthroid dosage will be reevaluated at that time if necessary. 2d) Patient was provided verbal and written instructions on ROM exercises, and verbalized understanding of such.