calculator assessments
advertisement

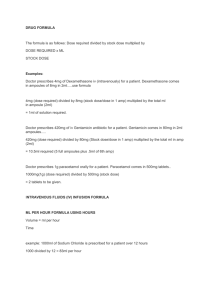
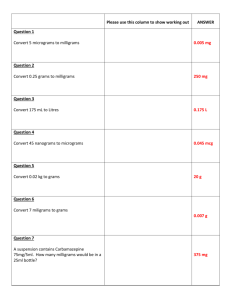
BSc (Hons) Midwifery Pre registration Student Numerical Assessment in practice workbook Name: Intake group: The purpose of this workbook is to help you practise your Numeracy skills. These are required by the NMC for the achievement of Practice Learning Outcomes relating to competence in numeracy, calculations and the safe administration of medicines. This workbook may be used as supportive evidence of your preparation, and therefore can be used in your discussions with your assessor/mentor. 2 Advice to Students Work your way through this workbook, working on the practice questions as you go. The answers are provided but try not to look at them before you have completed the exercises. Always show how you have worked out a particular question – this helps you identify any errors you might make, and could help you, and a reviewer, understand how you have arrived at the answer. Try wherever possible not to rely on using a calculator. By working things out on paper and using your own numeracy skills, you are more likely to be able to spot where an answer seems to be wrong – for example, you know ‘in your head’ that the answer is likely to be 3 tablets and yet the calculator answer suggests 12. Remember “For entry to the register, programme providers will use the ESC’s (Essential Skills Clusters) to inform the nature and content of numerical assessment where a 100% pass mark is required and all assessment must take place in the practice setting. The number of attempts is to be determined by the education provider.” NMC Circular 07/2007. The Essential Skills Cluster states: Summative health related numerical assessments are required to test skills identified (*) within the ESCs that encompass calculations associated with medicines. A 100% pass mark is required and assessment must take place in the practice setting. Medicines management in the context of midwifery practice is predicated on a partnership approach between the woman and the midwife. Its purpose is to provide therapeutic intervention when necessary throughout childbirth to facilitate a positive outcome. In order to meet the NMC’s directive that students’ numerical assessment must take place in the practice setting, it is proposed that students meet the following requirements: First Progression Point (End of year 1 midwifery modules) Competence statement: safely’ ‘Undertake medicinal product calculations 3 ESC skill Competent in calculating common dosages of medicinal products used in normal midwifery practice Requirement 1. Completion & pass of on-line numeracy assessment 2. Pass of Essential Skills Cluster in clinical practice Assessment Students must achieve 19 out of 25 questions and the test may be taken a maximum of 5 times in order for the standard to be achieved. Evidence to be assessed within practice and will include a drugs calculation test. Pass mark 75 % 100% As preparation for the practice assessment to be conducted by the mentor, students will be required to show evidence of achievement in the UWE on-line numeracy test. Students must present the on-line results prior to undertaking and demonstrating their achievement of the essential skills cluster to their Sign-off Mentor at progression point one. At the end of year two students should show Completion & pass of online Numeracy assessment. 80% (20 out of 25 questions.) in preparation for year three. Second Progression Point: for entry to the register. (End of year three midwifery modules). Competence statements: 1. ‘Within the parameters of normal childbirth, ensure safe and effective practice through comprehensive knowledge of medicinal products, their actions, risks and benefits including the ability to recognise and respond safely to adverse drug reactions and adverse drug events’. 2. ‘Undertake medicinal product calculations safely’. ESC skill Requirement Assessment 1. Manages drug administration and safely monitors its effect. 1. Completion & pass of on-line numeracy assessment. Students must achieve 20 out of 25 questions and the test may be taken a maximum of 5 times in order for the standard to be achieved. Evidence to be assessed within practice and will include a drugs calculation test. 2. Calculates accurately the medicinal products frequently 2. Pass of Skills Cluster in clinical practice to include administering of medicinal products safely via appropriate routes including specific Pass mark 80% 100% 4 encountered within the field of practice. requirements for neonates. As preparation for the practice assessment to be conducted by the mentor, students will be required to show evidence of achievement in the UWE on-line numeracy test. Students must present the on-line results prior to undertaking and demonstrating their achievement of the essential skills cluster to their Sign-off Mentor, at progression point two for entry to the register. Students must achieve a pass in both components in order to meet the NMC requirements. This Numeracy related workbook is available as an additional supportive resource for students at the start of the programme. Whilst this is not assessed by mentors, the Sign-off Mentor may utilise it as further evidence in making their judgement of the assessment of the student’s numerical competency. Summative health related numerical assessments are required to test skills identified (*) within the ESC’s that encompass calculations associated with medicines. A 100% pass mark is required and assessment must take place in the practice setting Thanks to colleagues for help in preparing this pack Author : Sue Davis Critical reader : Dorothy Cook 5 The Metric System SI units This is another name for the metric system of measurement. The aim of metrication is to make calculation easier than with imperial measurements. SI stands for System international and is now recognised as the standard system for measurement in most disciplines around the world. It was introduced to the NHS in 1975. Weight 1 kilogram 1 gram 1 milligram = = = 1000 grams 1000 milligrams 1000 micrograms 1 microgram = 1 nanogram = 1000 nanograms 1000 picograms Recognised abbreviations of these units are: kilogram = kg microgram = mcg gram = g nanogram = ng milligram = mg (Abbreviations for microgram and nanogram should not be used in prescribing.) Volume 1 litre = 1000 millilitres Recognised abbreviations of these units are: litre = L millilitre = ml Height 6ft 2inches = 1.88 metres 5ft .3inches = 1.6 meters Converting height 1 feet = 30.5 cms 1 inch is 2.5cms Height conversion = Feet to height X30.48 centimetres to feet x 0.328 Inches to cms x 2.54 centimetres to inches x0.3937 (Lapham and Agar 2003 ) 6 Strength of a solution This can be expressed as: a) % weight versus volume = number of grams per 100mls e.g. sodium chloride 30% = 30g in 100mls b) Parts e.g. Adrenaline 1 in 1000 = 1g in 1000ml = 1mg in 1ml Adrenaline 1 in 10,000 = 1g in 10,000ml = 1mg in 10mls Converting Larger Units to the Next Smaller Unit To convert a larger unit to a smaller unit you need to multiply by 1000. Example: Convert 5g to milligrams: Convert 0.25kg to grams: 5 x 1000 0.25 x 1000 = = 5000mg 250g Practice: Convert the following to micrograms 1. 0.5mg 2. 0.0625mg 3. 0.25 mg Convert the following into nanograms 4 0.25 mcg 5 0.0625 mcg 6 1.5mcg Converting Smaller Units to the Next Larger Unit: To convert a smaller unit to the larger unit you divide by 1000. Example: Convert 6000g to kilograms : Convert 325mg to grams: 6000/ 1000 = 325/ 1000 = 6kg 0.325g 7 Practice: Convert the following into milligrams 7 300mcg 8 75mcg 9 187.5 mcg Dealing with Decimal Points 25 x 0.5 ____ 12.5 25 x 0.05 _____ 1.25 There is one number after the decimal point There are two numbers after the decimal point in the sum therefore one in the sum therefore two after the point in the answer. after the point in the answer. Practice 10. 2.5 x 100 = 11. 0.3 x1000 = 12. 7.5 x 30 = 13. 36 60 = 14. 125 550 = 15. 5.5 50 = 16. 250 1000 = 8 Fractions To simplify fractions divide the top number into the bottom number, which divides into both of these exactly. This number is called a common factor. e.g. 24 = 2 (both numbers have been divided by 12, which is a common factor 36 3 used in this fraction). This could also have been completed in several steps: 24 36 = 12 18 (common factor is 2) = 4 6 (common factor is 3) = 2 3 (common factor 2) Then 12 18 Then 4 6 Converting Fractions to Decimals In order to convert a fraction to a decimal, you need to divide the top number by the bottom number. e.g. 1 = 2 2 (divide the bottom number into the top number) 0.5 1.0 = 0.5 Practice 17. 3 9 = 18. 6 = 12 21. 3 4 = 22. 1 100 19. 25 = 75 = 20. 7 8 9 Fluid Requirements First 10kg = 100ml/kg Second 10kg = 50ml/kg Subsequent = 20ml/kg Practice: Using the above formula calculate the daily fluid requirements 23. 6.2kg 24. 3.8kg 25. 29kg Unit Conversion 26. 4000 micrograms = mg 6mg 2 litres = 0.24 micrograms = ml = micrograms 75 mg = grams 187.5 micrograms = 650 ml = litres 0.25 micrograms = nanograms mg nanograms 10 Oral Liquids A sedative produced in concentration of 500mg/5mls. Calculate the volumes for the following doses: 27. Dose Prescribed (mg) 250 350 65 150 750 Volume Required (ml) Ranitidine comes in a concentration of 150mg in 10mls; calculate the volumes needed for the following doses: 28. Dose Prescribed (mg) 25 16 35 65 150 Volume Required (ml) Drug Dosages for Injection Volume Required = Dose prescribed Dose you have available x volume of stock solution e.g. A patient is prescribed cortisone 40 mg. The ampoules contain 50 mg in 2mls. Calculate the volume required. Using the formula 40 mg x 2ml 50mg = 40 x 2 50 1 11 Answer = 8 5 = 1.6 mls Practice 29. If 50 m.g of a drug is contained in 10ml of solution, how much must be given to give 25mg? 30. Prescribed: Erythromycin 270 mg Available: 300mg in 10 mls 31. Morphine 9 mg is required and the stock solution is 15mg in 1 ml. How much is required? 32. The ampoule reads 500micrograms in 5 mls of solution. How much solution is needed to give 10 micrograms? 33. Sally Ali is in hospital following surgery. She has an intra-venous infusion of 1 litre normal saline every 8 hours; she has vomited twice (30ml and 45ml); and her catheter has drained 1 300ml of urine during the last 12 hours. What is the difference between Sally’s fluid intake and output (in ml) over the last 12 hours ? 12 34. Jane, who has a bi-polar disorder, is going through a period of significant depression and there is some concern that her fluid balance is not being well maintained (see chart below for details). a) Complete this table to give the daily total for both intake and output FLUID INTAKE (millilitres) TIME 3rd March 4th March 5th March 08:00 09:00 10:00 11:00 12:00 13:00 14:00 15:00 16:00 17:00 18:00 19:00 300 300 250 DAY TOTALS 20:00 21:00 22:00 23:00 00:00 01:00 02:00 03:00 04:00 05:00 06:00 07:00 FLUID OUTPUT (millilitres) 6th March 3rd March 4th March 5th March. 6th March 250 280 280 230 250 250 125 135 225 300 135 133 240 270 140 152 200 300 250 175 220 370 230 270 250 525 225 250 300 450 330 125 100 380 150 350 320 400 300 NIGHT b) What TOTALS is Jane’s average daily fluid intake over these 4 days? 24 c)HOUR What TOTALS is Jane’s average daily fluid output over these 4 days? 35. d) Jane is thought to be developing a chest infection, so 400mg of an antibiotic is prescribed, to be administered 6-hourly. The antibiotic comes in a suspension of 125mg in 5 ml. How many ml will be needed for all doses over a 24-hour period? 345 13 36 . Susan has regular epileptic seizures but these are reasonably controlled through the use of medication. Currently she is prescribed Phenytoin in a suspension which contains 15mg/2.5ml. The initial dose is worked out according to body weight (3.5mg per kg daily). a) If Susan is 86kg what would her initial daily dose be (to the nearest 10mg)? Because Susan’s epilepsy is now generally well-controlled she is actually prescribed 255 mg Phenytoin a day to be given in 2 equal doses. b) How many millilitres of suspension should be given in each dose? Dosage calculations It is the midwife’s role to ensure the woman is given the correct amount of tablets which means finding out the amount of drug in each tablet and then calculating how many tablets to give to the woman. Sally is prescribed Drug A - 120 mg. but the tablets are only available as 40mg each How many tablets are required? The formula is the number of tablets + Amount prescribed Amount in each tablet The prescription is the total quantity to be given or what you want. The availability is the quantity in each tablet or what you have got So you can use the following formula to remember . The number of tablets = what you want What you have got Answer for this example is 3 tablets 14 Another important point is the need to ensure that the prescribed amount and the availability are in the same units. So you may need to convert milligrams into grams or convert grams into milligrams. Try the example below. 37. Mrs James is prescribed 350mg of drug A, four times daily for one week. Drug A is dispensed in tablets containing 175mg. Mrs James daily dose of drug A in grams is: Remember in practice it is highly unlikely that you will need to give the woman more than three or four tablets. So if this is occurring check with the pharmacist who may be able to advice. Also note that paediatric doses are usually only half the adult dose. Intravenous Drugs The rate of flow of fluid down an intravenous line must be regulated and this is normally controlled by a machine called an infusion controller. In some case you may have a giving set that needs you to set the drip rate measured in drips per minute. It is important that you know which you are dealing with as some infusion controllers allow you the operator to alter the flow of liquid and they may also require you to set the flow rate which is measured in millilitres per hour. And other requires a drip rate. This is normally written on the machine. To calculate the flow rate, you need to divide the volume in mls by the duration in hours. A woman may be prescribed 500mls Intravenous Infusion (IVI) over 12 hours . What is the flow rate? Answer 500 divided by 12 is 41.66ml/hr. If you do not have the facility to enter decimals, then round to the nearest whole number the answer would then be 42ml/hour. 15 On some types of flow controller, the size of each drop of liquid given is governed by the machines internal functions. These are normally fixed at the factory and cannot be altered for safety. The constant quantity gives rise to the drop factor which is the number of drops which make up every millilitre of fluid delivered. Special paediatric infusion controllers are also available. The drop rate +Total drops Time in minutes If the total volume of fluid is given in millilitres and the drop factor for the controller is known (written on the machine), the total number of drops which the woman will receive can be calculated by the expression. Total number of drops = drop factor X volume in ml Also if the time is given in hours we can calculate the time in minutes by multiplying 60 x time n hours. Drop rate = drop factor x volume in ml 60 x time in hours 38. Calculate the drop rate if the women requires 5% dextrose solution to be given IV over 12 hours via a machine that has a drop rate of 20. 20 = 20 drops per ml x 500ml = 60X 12 hours Infant Artificial feeding This is a further example of the use of formulae If babies are artificially fed it is important that feeds are made up correctly. Infants are normally fed on demand, but if the Paediatrician feel it is important and the condition of the baby requires regular feeds, the infant should receive 150 -200ml/kg body weight /24 hours. To calculate the volume of feed, values are substituted into the following equation. Amount of milk x weight of baby Number of feeds in 24 hours 16 To calculate the volume of a feed for a baby weighing 4.8Kg to receive 4 hourly feeds 150x4.8 = 120 ml per feed. 6 Or 200 x 4.8 = 160ml per feed 6 39. An infant (Max) is expected to regain his birth-weight after 2 weeks, then gain 200g per week until 3 months of age; 150g per week for a further 3 months of age. Assume 3 months = 13 weeks. The volume of feed Max requires is calculated according to the formula: Max requires approximately 115kcal/kg body weight per 24 hours. The birth weight of baby Max is 2.9kg. a) Calculate the volume of feed required if Max is to be fed every three hours. Secondly b) Calculate the expected weight of Max when aged 14 weeks 40. You may also have to calculate the energy requirements If the baby requires approximately 115 kcal/kg body weight per 24 hours. and the birth weight of baby Sam is 2.9kg. What is the energy requirements? Given that 1kcal = 4.2kJ, calculate the energy Sam receives in a day, when she is 14 weeks old (to the nearest whole number)? 17 Another calculation midwives may need to do is the Body Mass index.(BMI) The most common measurement is BMI (kg/M²) = Weight(KG) [Height(M)]² Below 18.5 18.5 -24.9 25 - 29.9 30 & Above Underweight Normal Overweight Obese 41. Calculate the following BMI Sarah is 1.6 m (height)and weighs 82kg = 42. Calculate the following BMI Polly is 1.72m (height) and weight 72kg = Insulin These drugs are expressed in terms of units as a standard measurement. There are no calculations involved in the administration of insulin either by injection or devices such as pens. Insulin comes in units and all you have to do is draw up the prescribed units or use the pen with the required dose. Insulin syringes are calibrated as 100 units in 1ml and are available as 1ml and 0.5 ml syringes. So if the dose is 30 units, you draw up to the 30 unit mark on the syringe. Heparin is also expressed in terms of units rather than weight. The strengths available are: 1,000units/mL 1mL, 5mL, 10mL ampoules 5,000 units /ml 1mL.%mL ampoules 10,000 units /ml 1mL ampoules 25,000units/mL 1mL ampoules. 18 A strength of 25,000 units ml is also available for subcutaneous use as 0.2ml ampoules containing 5,000 units. Calculations are required depending on the dose prescribed and the mode used to give it to the client. E.g. subcutaneous or intravenous. 43. You need to give an infusion of heparin containing 29,000 units over 24 hours. Assuming that the only strength you have available are 25,000 unit/ml and 5,000 units per ml, how much do you need to draw up for the dose prescribed.? You are advised to read the Nursing and Midwifery Council Standards for Medicines Management (2008) before YOU start to give any medicines. Standard 8 in particular Also read the Midwives rules and standards (2004) rule 7. Remember Safe medication means giving the correct medication, to the right person, in the right amount, at the right time and by the correct route You need to ensure you familiarise yourself with administrations routes, common abbreviations, and the pharmacy drug charts used in your Trust. Other aspects such as trade names /brand names/ pharmaceutical forms/ clinical details/contraindications and interactions should be considered. Pregnancy and lactation- clinical trials are mainly based on animal studies and any observations in humans recorded. Reference in the text Lapham R Agar H (2003) Drug calculations for Nurses a step b step approach 2nd edition. Hodder and Arnold London Coben D Atere-Roberts E (2005) Calculations for Nursing and Health care 2nd Edition Palgrave Macmillian Hampshire. Or UWE http://learntech.uwe.ac.uk/numeracy 19 Common midwifery drugs used in OSCE practice. Syntometrine Dosage : 1ml. - 5 units syntocinon 500mcg ergometrine Route: Intramuscular Action: Syntocinon – uterine contraction Ergometrine – sustained contraction 45 minutes Syntocinon Dosage either 10 units Intramuscularly or 30 - 40 units /500mls Normal saline Intravenously Rate: 125 mls/hour Ergomentine Dosage : 500mcg Route: Intramuscular/intravenous Action: Sustained contraction/living ligature effect. IM – 7 minutes IV - 45 seconds Only 2 doses of ergometrine can be given Other drugs Magnesium Sulphate: ACTION: Relieves Cerebral Vasospasm DOSE: IV route preferred: Loading dose 4g over 5-10 minutes followed by a maintenance infusion of 1g/hr (continued at least 24 hours after the last seizure). Recurrent seizures should be treated by a further bolus of 2g (RCOG, 1999) Side Effects: Magnesium Sulphate Magnesium toxicity Loss of deep tendon reflexes Respiratory Depression Respiratory Arrest Clinical Observations Required: 20 Hourly measurements of the patellar reflex (if absent, withhold further doses of Magnesium Sulphate until reflexes return) ECG (BNF, 1996) Respiratory rate Oxygen saturation Regular monitoring of serum levels should be considered in women with oliguria (urine output < 100mls in 4 hours) as this drug is excreted by the kidney Monitor fetal heart rate continuously if not delivered Respiratory Depression: Treat with Calcium Gluconate 1g IV given over 10 minutes Diazepam: Dose: 10 mgs IV Hydralazine (5mgs iv repeated every 20 minutes to a MAXIMUM dose of 20mgs) Labetolol (20 mgs iv can be titrated escalating to 40-80mgs every 10 minutes to a maximum dose of 300mgs (RCOG, 1999) These drugs can cause fetal distress. If fetus undelivered continuous CTG is advocated (RCOG, 1999) Paracetamol Lignocaine Hydrochloride 1% Pethidine Naloxone Hydrochloride Vitamin K by injection and oral Ranitidine Human Anti D immunoglobulin Ibrupofen Ferrous sulphate A number of these drugs come under either Patient group protocols or Patient group directives. These will be discussed on your wards and during the programme. 21 Answers to Practice Questions 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. 22. 23. 24. 25. 500 micrograms 62.5 micrograms 250 micrograms 250 nanograms 62.5 nanograms 1500 nanograms 0.3 mgs 0.075 mgs 0.1875 mgs 250 300 225 0.6 0.2272 0.11 0.25 0.333 0.5 0.333 0.875 0.75 0.01 1310 mls 380 mls 1680 mls 26. 4000 micrograms = 4 mg 6mg = 6000 micrograms 2 litres = 2000ml 0.24 micrograms = 240 nanograms 75 mg = 0.075grams 187.5 micrograms = 0.1875 mg 650 ml = 0.65 litres 0.25 micrograms = 250 nanograms 27. Dose Prescribed (mg) 250 350 65 150 750 Volume Required (ml) 2.5 3.5 0.65 1.5 7.5 22 28. Dose Prescribed (mg) 25 16 35 65 150 Volume Required (ml) 1.66 1.066 2.33 4.33 10 29. 30 31 32 33 5 mls 9 mls 0.6 mls 0.1 mls 125mls 34 a) Daily intake and output. FLUID INTAKE (millilitres) TIME 3rd March 4th March 5th March 08:00 09:00 10:00 11:00 12:00 13:00 14:00 15:00 16:00 17:00 18:00 19:00 300 300 250 DAY TOTALS 20:00 21:00 22:00 23:00 00:00 01:00 02:00 03:00 04:00 05:00 06:00 b)What 07:00 FLUID OUTPUT (millilitres) 6th March 3rd March 4th March 5th March. 6th March 250 280 280 230 250 250 125 135 225 300 135 133 240 270 140 152 200 300 250 175 220 370 230 270 250 525 225 250 300 1645 925 920 1215 950 450 695 330 700 125 100 760 380 150 350 320 is Jane’s average daily fluid intake over these 400 4 days? 300=1270mls 345 NIGHT TOTALS 0 100 125 150 850 630 670 725 24 HOUR TOTALS 1645 1025 1045 1365 1800 1325 1370 1485 23 c) What is Jane’s average daily fluid output over these 4 days 1495ml 34 B)Average daily fluid intake = 1270mls C) Average daily output. =1495ml 35 D ) 64mls 36 . Susan has regular epileptic seizures but these are reasonably controlled through the use of medication. Currently she is prescribed Phenytoin in a suspension which contains 15mg/2.5ml. The initial dose is worked out according to body weight (3.5mg per kg daily). a) If Susan is 86kg what would her initial daily dose be (to the nearest 10mg)? 300mg Because Susan’s epilepsy is now generally well-controlled she is actually prescribed 255 mg Phenytoin a day to be given in 2 equal doses. B ) How many millilitres of suspension should be given in each dose? 21.25ml 37. Mrs James daily dose of drug A in grams is: 1.4g 38. Calculate the drop rate if the women requires 5% dextrose solution to be given IV over 12 hours via a machine that has a drop rate of 20 = 13.89 drop rate.( Rounded up would be 14 drops per minute ) 39. a) Calculate the volume of feed required if Max is to be fed every three hours.= 72.5ml b) Calculate the expected weight of Max when aged 14 weeks= 5.25kgs 40. Calculate the energy requirements for Sam = 2.536 Kilojules 41. Sarah is 1.6 m and weighs 82kg = 32 BMI 42. Polly is 1.72m (height) and weighs 72kg = 24 BMI 43. Amount required 1XHeparin 25,000 unit /ml ampoule and 0.8ml of Heparin from the 1X5,000 unit/ml and then add to the infusion. 24