Nursing Care For The Newborn & Family
advertisement

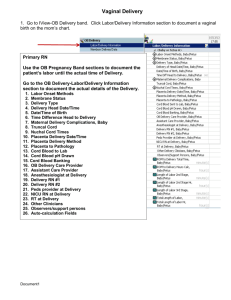
Nursing Care for the Newborn & Family Nursing Care of the Newborn Newborns undergo many profound physiologic and psychological changes. They are released from a warm, close, dark, liquid filled environment that met all needs, into a chilly, unbound, brightly lit, gravity based, outside world. Within minutes respirations are initiated and circulatory accommodation are made. Within 24 hours neurologic, renal, endocrine, GI, and metabolic functions must operate. Newborn or neonatal period is the first 28 days of life. 2/3 of deaths occur in the 1st year ½ occur in the 1st 24 hours Assessment Mother’s pregnancy history Physical exam of the newborn Lab reports Bonding Profile of the Newborn All newborns are different. Vital Statistics Weight: Plot on neonatal graph (Appendix E) Average weight R/T gestational age White female 7.5 lbs.– 3.4 kg. White male 7.7 lbs.-3.5 kg. Other races-0.5 lbs less Limits-5.5 lbs to10 lbs (17 lbs largest) Newborn loses 5 to 10 % of birth weight ( 6 to 10 oz. during first few days. Loss due to salt and fluid retaining maternal hormones. Voiding and stool, and diuresis. After wt. loss then 1 day of stable wt. then recaptures birth weight within: Breastfed 10 days Formula fed 7 days Will gain 2 lb/month (6 to 8 oz/week) for first 6 months. Length: Female-53 cm.- 20.9 in. Male-54 cm. –21.3 in. Limits 18 in. to 23 in. Head Circumference: 34 to 35 cm. (13.5 to 14 in.) Limits-less than 33 cm. or greater than 37 cm. Measure with tape drawn across center of forehead and around the most prominent portion of the posterior head. Chest Circumference: About 2 cm. less than head circumference (0.75 to 1 in.). Measure at level of the nipples. Viral Signs: Temp 99 F at birth Newborns lose heat by: Convection Conduction Radiation Evaporation They have little subcutaneous fat for insulation. Shivering is rare. They have brown fat – helps to conserve or produce body heat by increasing metabolism. Quickly dry and wrap newborns and place under radiant heat source or place directly against mothers skin. Newborn with a bacterial infection will have a subnormal temperature. Pulse: Immediately after birth 180 bpm. Within 1 hour- 120 to 140 bpm. Irregular and transient murmurs due to immaturity of the cardiac regulatory center in the medulla and closure of the shunts. Sleeping – 90 to110 bpm. Always check apical for 1 full minute Check femoral pulse for coarctation. Respiration: 30 to 60 breaths / min. Rate, depth, and rhythm may be irregular with short periods of apnea (without cyanosis) called periodic respirations. Observe movement of the abdomen. Coughing and sneezing clear the airway. Newborns are nose breathers Short periods of crying are beneficial. Blood Pressure: 80/46 mm Hg at birth 10th day 100/50 mm Hg Cuff 2/3 the length of upper arm or thigh. Physiologic Function Cardiovascular System: Peripheral circulation is sluggish for 1st 24 hours. Common to see cyanosis of the feet and hands (acrocyanosis) cold to touch. Blood values: Blood volume-300 mL Increased erythrocyte count-will decrease after 3 days. Breakdown of these cells cause an increase bilirubin >4 mg/100mL At 7 mg/ml tissue is jaundice. Physiological jaundice R/T brusing, cephalhematoma, dehydration, or intestinal obstruction. Treat at 10-12 phototherapy, fluids, >20 neuro kernicterus (permanent cell damage) Hgb 17-18 Hct 45-50% (use warm cloth on heel to increase sluggish circulation to get a more accurate value). WBC increased due to stress of birth. Blood Coagulation: Prolonged coagulation or prothrombin time for 24 hours because of low vitamin K level. Infant intestine is sterile at birth. Administer Vitamin K (AquaMephyton) 1 hour after birth in lateral anterior thigh. Respiratory: First breath initiated by Cold receptors Lowered PO2 (15 mm Hg) Increased PCO2 (70 mm Hg) Surfactant allows the alveoli to inflate more easily. 1/3 of fluid is forced out of the lungs with the pressure of delivery. Within 10 min. a good residual volume is established. Gastrointestinal System: Sterile tract for 1st 24 hours Stomach holds 60 to 90 mL Decreased ability to digest fat and starch Regurgitation due to immature cardiac sphincter between stomach and esophagus. Lower glucose and protein serum levels due to immature liver. Stools – meconium 1st 24 hours. Sticky, tarlike, blackish green, odorless. If no meconium in 24-48 hours possibility of ileus, imperforate anus, or bowel obstruction. Transitional stool- day 2-3 becomes green and loose. Day 4 breastfed will pass 3-4 light yellow stools per day. Bright green is due to increased bilirubin. Watery and loose or mucus may be a milk allergy. Gray clay stool – bile duct obstruction. Urinary System Voids within 24 hours Light color and odorless; kidneys do not concentrate urine well and no reabsorption. 6 voids /day 15 to 50 mL By 1st week total daily volume is 300 mL Immune System: Unable to form antibodies the 1st 2 months. Has passive immunity from the mother Hepatitis B vaccine during 1st 12 hours. Neuromuscular System: Reflex Maneuvers: Blink reflex Rooting Sucking Swallowing Extrusion Palmar Grasp Step-Walk in Place Placing Plantar Grasp Tonic Neck Moro Babinski Magnet Crossed Extension Trunk Incurvation Landau Deep Tendon Senses: Hearing in utero Vision see immediately, blink, follow objects Touch well developed Taste likes glucose and avoids salt Smell breast milk Adjustment to Extrauterine Life Skin Color: Ruddy due to increased concentration of RBC in blood vessels and decreased fat. Fades slightly over the 1st month. Cyanosis-lips, hands, feet Central cyanosis is a great concern Suction mouth before the nose because suctioning the nose may trigger a reflex gasp, possibly leading to aspiration. Appearance of the Newborn Hyperbilirubinemia leads to jaundice or yellowing of the skin. Occurs on day 2 or 3 in 50% of all newborns due to breakdown of fetal RBC. Indirect bilirubin > 7mg/100 mL Early feeding promotes intestinal movement and helps prevent bilirubin build up. Pallor due to anemia. Excessive blood loss when cord was cut. Inadequate flow of blood from cord into infant at birth. Fetal maternal transfusion Low iron stores Blood incompatibility Internal bleed in the baby CNS damage Harliquin Sign-newborn lying on side and it will appear red on the dependent side of the body and pale on the upper side, changing positions will make it fade. Birthmarks Hemangiomas-vascular tumors of the skin. Nevus flammeus-port-wine stain Macular purple or dark red lesion Appears on face or thigh Those above the bridge of the nose fade Can be covered by cosmetics, remover surgically, or by laser therapy. Stork’s beak marks – at nape of neck, lighter pink patches. More frequent in females. Do not fade. Strawberry Hemangiomas: Elevated areas formed by immature capillaries and endothelial cells. Appear at birth or 2 week later. Due to high estrogen levels 50 to 75% may disappear by age 7 Mark may grow in size. Surgery not recommended due to scarring Cavernous Hemangiomas: Dilated vascular spaces Raised and resemble a strawberry hemangioma but does not disappear. Surgically removed. Mongolian Spots: Collection of pigment cells (melanocytes) that appear slate-gray patches on sacrum or buttocks S/T arms and legs. Asian, Southern European, or African Disappear by school age. Vernix Caseosa: White, cream cheese-like substance that serves as a skin lubricant. Lanugo: Fine hair, covers newborn’s shoulders, back, and upper arms. Forehead and ears. By age 2 weeks it has disappeared. Desquamation: Dry skin on palms of hands and soles of feet. Milia: Pinpoint white papule found on cheek or across bridge of nose. Disappear by 2 to 4 week as sebaceous glands mature. Erythema Toxicum (flea-bite rash): Rash, appears 1st to 4th day up to 2 weeks of age. Lacks pattern and will last only hours. Due to eosinophils reacting to environment. Forceps Marks: May have a circular or linear contusion matching the rim of the blade on infants cheek. Disappears in 1 to 2 days Assess facial nerve while at rest and crying. Skin Turgor: Feels elastic, smooth if well hydrated. Head: Appears large, 1/4th total length, forehead large and prominent. Chin receding, quivers easily. Full-body of hair if well nourished Pinpoint ulcer where monitor was attached. Fontanelles: Openings where skull bones join Anterior fontanelle Junction of parietal and frontal bones. Diamond shaped-2 to 3 cm. width and 3 to 4 cm. length. Closes at 12 to 18 months Posterior fontanelle Triangle shaped-1 cm. length. Closed at 2 months. Sutures: May override at birth. Molding: Infant’s head (vertex) engages the cervix. After birth, appears prominent and asymmetric. Will restore to normal shape in a few days. Caput Succedaneum: Edema of the scalp at the presenting part of the head. Crosses the suture line, will be absorbed and disappear by the 3rd day. Cephalhematoma: Collection of blood between periosteum of the skull bone and bone itself caused by rupture of periosteum capillary at birth. Occurs 24 hours after birth, severe swelling, black and blue, egg shape. Swelling stops at suture line. Takes weeks to be absorbed. Craniotabes: Localized softening of the cranial bones. Indents easily with touch of the finger. Corrects after a few months. Eyes: Usually tearless, lacrimal ducts mature at 3 months. Irises-gray or blue Sclera-blue due to thinness. Permanent eye color between 3 to 12 mo. Erythromycin ointment EES-for chlamydia and gonorrhea Subconjunctival hemorrhage-red spot on sclera or red ring around cornea. Absorbed in 2 to 3 weeks. Edema around orbit or on eyelid. Will remain for 2-3 day until kidneys remove the fluid. Ears: External not completely formed. Top part in line with inner canthus of eye. Test hearing by ringing a bell 6 in. from ear. Nose: Appears large. Assess by closing mouth and compress one naris. Mouth: Open evenly, tongue appears large. Palate intact, check for cysts. No teeth (1-2 natal teeth sometimes). Neck: Short, chubby, skin folds, rotates freely. May try to raise head but lacks control. Chest: Breast appear engorged, may secrete a thin, watery fluid (witch’s milk). 1 wk to subside 2 in. less than head. Lungs have rhonchi due to mucus for first 24 to 48 hours. Alveoli open slowly. Abdomen: Slightly protuberant Bowel sounds within 1 hour. Liver palpable 1 to 2 cm below right costal margin. Umbilical cord-white, gelatinous structure with red and blue streaks. Count veins and arteries. Inspect cord clamp, within 1 hour cord begins to dry and shrink and turns brown. Day 2 to 3 will turn black. Day 6 to 10 breaks free and new granulating area will heal in next week. Assess abdomen by stroking each quadrant and observe umbilicus to move or wink in that direction. Anogenital Area: Check for patency. Male Genitalia: Scrotum edematous and has rugae. Penis 2 cm., check prepuce (foreskin). Circumcision Female Genitalia: Vulva swollen due to effect of maternal hormones. Mucus vaginal secretion, sometimes blood tinged. Back: Flat in lumbar and sacral areas. Back rounded, arms and legs flexed on abdomen and chest. Extremities: Appear short, hands plump,clinched and palmar crease. Fingernails soft, smooth and long. Muscle tone- unflex arm and immediately returns flexed. Fingertips cover proximal thigh. Legs bowed and short, feet turn inward. ROM Ortolani’s sign-clunk of femur head striking the shallow acetabulum. Barlow’s sign-hip slips in socket. Lying on abdomen newborns bring arms and legs underneath them and rise their stomach off the bed. Assessment of the Newborn Apgar Scoring: 1 minute and 5 minutes after birth Rated 0,1,or 2 then added together. Score of 4-6 = guarded, 7-10 = good. Heart rate-auscultate with stethoscope. Respiratory effort-cries spontaneously at 30 seconds after birth. Muscle tone-extremities tightly flexed. Reflex irritability-suctioning or sole of feet slapped. Color-cyanotic at birth, pink shortly after first breath. Respiratory Evaluation Highest priority in newborn care. Physical Examination Given immediately after birth, very quickly Height and Weight Nude, also head, chest and abdominal circumferences. Weight daily at same time. Laboratory Studies Heel stick for H&H and hypoglycemia (< 40mg/100 mL) Gestational Age Ballard’s assessment Behavior Capacity Physically active and emotionally prepared to interact with people. Brazelton Neonatal Behavioral Assessment Scale Evaluates newborn’s behavioral capacity or ability to respond to stimuli. Care of the Newborn at Birth Equipment-radiant heat table, warm soft blankets, O2, resuscitation, suction, eye care, identification, scales. Handle gently Newborn ID and Registration ID Kidnapper profile- recently lost a pregnancy or had an infant stillborn and who desires an infant very much. Familiar with hospital, pretends to be a volunteer or unlicensed health care worker and says she needs to take the baby out of the nursery. ID Band (one arm and one leg) Plastic bracelet, number corresponds to the mother’s hospital number, mother’s full name, sex,date and time of infant’s birth. Has built in sensor unit that alarms if baby is transported beyond set boundaries. Foot prints are taken and placed on chart. Registration filed with the Bureau of Vital Statistics of the state of birth. Infant’s name, mother’s name, father’s name if mother chooses, birth date and place. Important because it provides eligibility for school, voting, social security benefits, passports. Birth Record Documentation: Time of birth Time the infant breathed Whether respirations were spontaneous or aided Apgar at 1 and 5 minutes of life Whether eye prophylaxis was given Whether vitamin K was administered General condition of the infant Number of vessels in umbilical cord Whether cultures were taken Whether infant(1)voided and (2) passed stool. Nursing Interventions Keep Newborn Warm: Reassess temp in 1 hour then q 4-8 hours. Promote Adequate Breathing Pattern and Prevent Aspiration: Suction with bulb syringe Record First Cry: Aided or unaided Inspect and Care for Umbilical Cord Hazeltine or Kane clamp Count vessels Apply triple dye Coed falls off 7 to 10th day. Do sponge bath. Apply alcohol to cord site. Administer Eye Care Erythromycin ointment General Infection Precautions Wash up to elbows between babies, gown Personnel with infections excluded until clear. Isolate with contagious illness. Postpartal Period Initial Feeding: May breastfed immediately Formula fed in 2-4 hours On demand schedule may be q 2 hours First bath within 1 hour Supervise parents with 1st bath, cleanest to most soiled. No soap on face. Football hold Sleeping Position On back due to SIDS Diaper Area Care Wash with clear water and dry. A&D may be applied to buttocks Metabolic Screening Tests PKU-phenylketonuria-disease of defective protein metabolism Hypothyroidism 3 drops from heel stick on special filter paper. Hepatitis B Vaccination Within 12 hours after birth, second dose due in 1 month and 3rd due at 6 months. Care of the Newborn in Postpartal Vitamin K Administration Newborn’s are at risk for bleeding disorders Single dose 0.5 to 1.0 mg IM of vitamin K is administered within 1 hour after birth. Circumcision Surgical removal of penis foreskin 1st or 2nd day of life Check q 15 min for 1 hour for bleeding, document voiding after the procedure. Petrolatum for 3 days. Readiness To Care For Newborn Assess how prepared each family is to care for the newborn. Infants wake up during the night for 1 or more feedings for about the 1st 4 months. Numerous questions to ask to assess for an adequate and safe home. Daily care: Some consistency Satisfy the infant Sense of well-being and contentment Sleep Patterns Sleeps 16 of 24 hours in 1st week at 4 hour intervals By 4 months 15 hours of 24 and through the night. Crying 2 hours of every 24 for 1st 7 weeks. Peaks at 6 to 7 weeks then tapers off. Most typical wakeful time is between 6pm to 11 pm. Pacifier is up to parents. Cleanliness is a concern Parental Concerns Related to Breathing Stuffy nose or making snorting noises in sleep, have mucus for 2 weeks Breath irregularly Continued Heath Maintenance for Newborn Appointment with PCP in 2 to 6 weeks Parents need to judge the infants state of health, appearance, eating, activity, disposition. Car Safety Meets federal guidelines Health Dept or Red Cross has info. Place in back seat may use a blanket to support the head. Facing the back.