LESSON 6: BLEEDING AND WOUNDS
advertisement

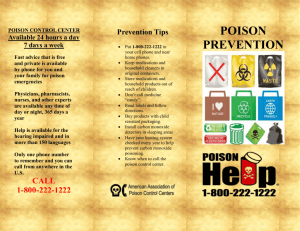
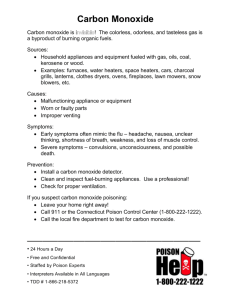
Lesson Outlines Chapter 18 Lesson 18: Poisoning Lesson Objectives After completing this lesson, participants should be able to: Describe how to care for ingested poison. Describe how to care for a victim with possible alcohol intoxication. Describe how to care for a sympathomimetic user. Describe how to care for hallucinogen use. Describe how to care for a marijuana overdose. Describe how to care for an opiate overdose. Describe how to care for a depressant overdose. Describe how to care for someone who has abused an inhalant. Describe how to care for carbon monoxide poisoning. Describe how to care for plant-induced dermatitis. Describe how to care for a stinging nettle poisoning. Points Types of Poisons Ingested (swallowed) o Through the mouth Inhaled (breathed) o Through the lungs Absorbed (contact) o Through the skin Injected o Through needlelike device Ingested (Swallowed) Poisons Poisoning from ingestion occurs when a victim swallows a toxic substance. Most ingested poisons have low toxicity or are swallowed in small amounts. Poisoning from ingestion is common among children. Some ingested substances can block the airway. Analgesics are the most common poisoning from ingestion. Most exposures to plants are minor. Recognizing Ingested Poisoning Abdominal pain, cramping Nausea or vomiting Diarrhea Burns, odors, or stains around or in mouth 1 of 8 Lesson Outlines Chapter 18 Drowsiness or unresponsiveness Poison container nearby Care for Ingested Poisons Determine the age and size of the victim, what and how much poison was ingested, and when it was taken. If corrosive or caustic, have the victim sip cold water or milk. Call the poison control center at 800-222-1222 if the person is responsive. o They can advise if medical care is needed. For unresponsive victim, call 9-1-1. Place victim in recovery position Do not induce vomiting. Give activated charcoal (neutralizer) if available and if instructed to do so by poison control. o Activated charcoal is a black, tasteless, odorless, insoluble, inert powder that binds to poison, but it does not absorb all drugs well. Save poison containers, plants, or victim’s vomit to help identify the substance. Alcohol Intoxication Alcohol is a depressant, not a stimulant. o It affects a person’s judgment, vision, reaction time, and coordination. It is the most commonly used and abused drug in the United States. It is one of the most lethal and is implicated as cofactor in drownings, traffic deaths, homicides, and suicides. Helping the intoxicated person is often difficult because the person can be belligerent or combative. Take the condition seriously. o It can be life-threatening. Recognizing Alcohol Intoxication Odor of alcohol Unsteadiness, staggering Confusion Slurred speech Nausea and vomiting Flushed face Seizures can also result. Care for Alcohol Intoxication Look for any injuries. Monitor breathing. Place in recovery position. Call poison control for advice (1-800-222-1222). If victim becomes violent, leave the area and await police. Provide emotional support. 2 of 8 Lesson Outlines Chapter 18 If victim is unresponsive, await EMS. Suspect hypothermia. Move the person to a warm place. Drug Emergencies Drug classifications: o Uppers (stimulants)—amphetamines, cocaine, caffeine o Downers (sedative-hypnotic)—barbiturates, tranquilizers, marijuana, narcotics o Hallucinogens—LSD, mescaline, peyote, PCP o Volatile chemicals—glue, cement, paint solvent, gasoline, spray paint, nail polish remover Sympathomimetics Stimulants (“uppers”) Produce excitement Amphetamines, methamphetamines Taken by mouth or injected Cocaine o One of most addictive substances known Crack o Pure cocaine, smoked Recognizing Sympathomimetic Use Disorganized behavior Hyperactivity Restlessness Anxiety or great fear Paranoia Delusions Care for Sympathomimetic Use Check breathing. Call poison center or 9-1-1. Check for injuries. Place in the recovery position. Give reassurance and emotional support. If violent, seek safety until police arrive. Seek medical care. Hallucinogens Produce changes in mood, sensory awareness Hear colors, see sounds Cause hallucinations, bizarre behavior Protect user from hurting self 3 of 8 Lesson Outlines Chapter 18 Recognizing Hallucinogen Use Visual hallucinations Intensity of vision and hearing Care for Hallucinogen Use Check breathing. Call poison center or 9-1-1. Check for injuries. Place in the recovery position. Give reassurance and emotional support. If violent, seek safety until police arrive. Seek medical care. Marijuana Flowering hemp plant Estimated 20 million people use marijuana daily in US Recognizing Marijuana Overdose Euphoria, relaxation, drowsiness Short-term memory loss Impaired capacity for complex thinking and work Depression, confusion Altered perception of time Anxiety, panic Hallucinations Care for Marijuana Overdose Check breathing. Call poison center or 9-1-1. Check for injuries. Place in the recovery position. Give reassurance and emotional support. If violent, seek safety until police arrive. Seek medical care. Depressants Often prescribed as part of legitimate medicine People may solicit prescriptions from several physicians. Includes: o Opiates (narcotics) o Sedative hypnotics (barbiturates and tranquilizers) Recognizing Sedative-Hypnotic Drug Use Drowsiness, sleepiness Slurred speech 4 of 8 Lesson Outlines Chapter 18 Slow breathing rate Opiates Pain relievers named for opium Heroin, codeine, morphine Frequently abused Addicts may start with appropriate prescription Recognizing Opiate Overdose Reduced breathing rate Pinpoint pupils Sedated condition, unresponsiveness Care for Depressant Overdose Check breathing. Call poison center or 9-1-1. Check for injuries. Place in the recovery position. Give reassurance and emotional support. If violent, seek safety until police arrive. Seek medical care. Abused Inhalants Glue, gasoline, lighter fluid, nail polish Similar effects to alcohol Can die of suffocation Can change heart rhythm Can cause permanent brain damage Recognizing Abused Inhalant Mild drowsiness, unresponsiveness Slurred speech, clumsiness Seizures Slow breathing rate Smell of solvents Care for Abused Inhalant Check breathing. Call poison center or 9-1-1. Check for injuries. Place in the recovery position. Give reassurance and emotional support. If violent, seek safety until police arrive. Seek medical care. 5 of 8 Lesson Outlines Chapter 18 Carbon Monoxide Poisoning Carbon monoxide is an invisible, tasteless, odorless, colorless, nonirritating gas, so victims are often unaware of its presence. It is the leading cause of poisoning death in the United States each year. Carbon monoxide poisoning can be unintentional or a method of suicide. People who ride long distances in older, poorly maintained cars are at increased risk. Many deaths involve people sleeping inside a running car, often after alcohol consumption. Dangerous sources of carbon monoxide include faulty furnaces, water heaters, and kerosene heaters. Carbon monoxide causes hypoxia. o Hemoglobin binds to it and the carbon monoxide does not allow cells to use oxygen. Recognizing Carbon Monoxide Poisoning Headache Ringing in ears Chest pain Muscle weakness Nausea and vomiting Dizziness and visual changes Unresponsiveness Respiratory and cardiac arrest Symptoms come and go Symptoms worsen and improve in certain places and at certain times Nearby people have similar complaints Pets seem ill. Care for Carbon Monoxide Poisoning Get the victim out of the toxic environment. Call 9-1-1. EMS can give 100% oxygen for 30 or 40 minutes to reverse CO poisoning. Monitor breathing. Place an unresponsive, breathing victim in the recovery position. Seek medical care. Plant-Induced Dermatitis Poison ivy, poison oak, poison sumac 15-25% of exposed people will have incapacitating swelling and blisters. Oil oozes out from the plant when it is brushed. The oil is not visible on human skin. It is spread by direct contact and can stay active for months or years on objects. Smoke from burning plants can cause severe dermatitis. 6 of 8 Lesson Outlines Chapter 18 Most people cannot identify these irritating plants. o The leaves grow in groups of three. Recognizing Plant-Induced Dermatitis Rash Itching Redness Blisters Swelling The greater the amount of skin affected, the greater the need for medical care. Onset usually occurs 1-2 days after contact. Care for Plant-Induced Dermatitis Wash affected area with soap and cold water as soon as possible Apply rubbing alcohol liberally, then remove the alcohol with water. For a mild reaction, have the victim soak in a lukewarm bath with 1 to 2 cups of colloidal oatmeal. Or, apply one of the following: o Wet compresses with aluminum acetate o Calamine lotion or baking soda paste o For a mild to moderate reaction, use a corticosteroid ointment. o For a severe reaction, use a physician-prescribed oral corticosteroid Stinging Nettle Plant with stinging hairs on stem and leaves Stinging hair is touched Fine needlepoint penetrates skin Injects chemical irritant Recognizing Stinging Nettle Poisoning Can affect anyone Effects limited to exposed area Immediate response Redness Rapid, intense burning Itching Reaction lasts hours, not days Care for Stinging Nettle Poisoning Wash exposed area with soap and water. Apply: o Cold, wet pack o Colloidal oatmeal, hydrocortisone cream, or calamine lotion o Over-the-counter antihistamine 7 of 8 Lesson Outlines Chapter 18 8 of 8