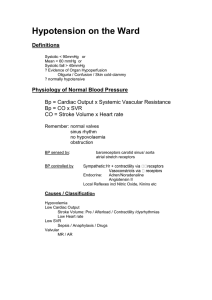
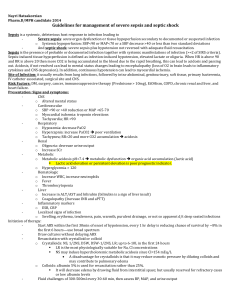
hypotension and tachycardia
advertisement

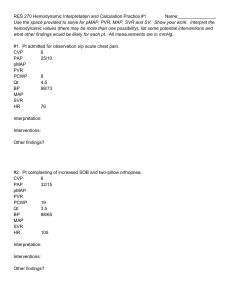
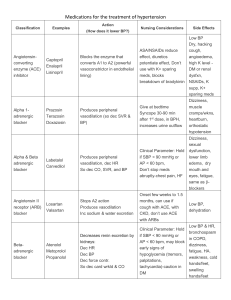
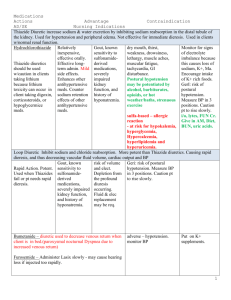
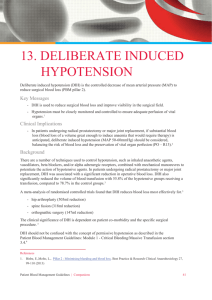
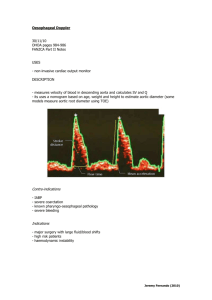
Intern’s approach to hypotension When a nurse calls you for hypotension… Ohm’s Law: V = IR MAP = CO x SVR MAP = (HR x SV) x SVR SV preload, afterload, and contractility 1. Confirm hypotension –proper cuff, A-line zeroed 2. Heart rate – is the heart rate appropriate for the amount of hypotension? (too slow, too fast, loss of AV synch) 3. SVR – examine if a patient is warm and dilated (low SVR) or cold and clamped (high SVR). Check for supportive evidence such as fever/hypothermia, leukocytosis, source of infection. Check also other etiologies of vasodilation, including adrenal insufficiency, medications. 4. Stroke volume – determined by 3 factors a. Preload – their intravascular volume status. Check ins/outs, UIOP, BUN/Cr, CVP. b. Afterload – refers to intrinsic afterload of the heart contributing to hypotension. Examine for MR, AS, VSD. c. Contractility – cannot be assessed by exam. NEED quick look echo or swan. 5. Classification of shock – excluding massive PE, there are 3 types a. Cardiogenic – decreased cardiac output. Traditionally with elevated SVR. b. Hypovolemic – decreased CVP and PCWP c. Vasodilatory – due to increased eNOS production, vasopressin deficiency, and stimulation of K/ATP channel; or meds. 6. You cannot treat hypotension properly (and may harm pt) if you do not know the etiology. 7. If you cannot determine the etiology at the bedside, or hypotension not responding to treatment, you may need a swan-ganz catheter. a. CVP b. PA c. PCWP d. CO Intern’s approach to tachycardia (aka…Doc this patient’s HR is 130. What do you want me to do?) 1. Is the patient stable? 2. Get a stat EKG (and/or go look at the tele strip/monitor yourself!)