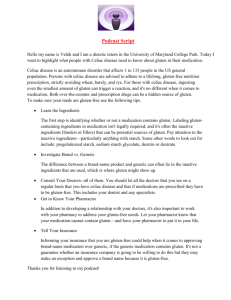
the potential role of gluten in equine inflammatory small bowel disease
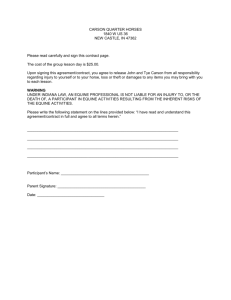
advertisement

THE POTENTIAL ROLE OF GLUTEN IN EQUINE INFLAMMATORY SMALL BOWEL DISEASE RESEARCH PROJECT, veterinary medicine. Lotte Anna van Putten 3155919 The potential role of gluten in equine inflammatory small bowel disease. Department of Equine Sciences, Medicine Section, Faculty of Veterinary Medicine, Utrecht University The VUmc Research Institute for Cancer and Immunology & the Department of Gastroenterology and Hepatology SUPERVISOR: Dr. J.H. van der Kolk EXTERN SUPERVISOR: Prof. dr. C.J.J. Mulder Dr. B.M.E. Blomberg (Dr. M.W.J. Scheurs) DATE OF SUBMISSION: 01-10-2010 UTRECHT UNIVERSITY Research Project Veterinary Medicine Oct2010- March2011 Research supervisors: UU: Dr. J.H. van der Kolk Dr. G.C.M. Grinwis VUmc: Dr. B.M.E. von Blomberg M. Reijm Dr.N.C.T. van Grieken Prof. Dr. C.J.J. Mulder Lotte van Putten, 3155919 Motivation Equine inflammatory small bowel disease (ISBD) is an idiopathic pathologic condition of the small intestine characterised by substantial reduction of the available absorptive surface area. Signs include a dull hair coat, weight loss, recurrent colic and at times soft faeces, depression and oedema. The condition is regularly associated with anaemia. ISBD is a rare disease that in recent years seems to be increasing in frequency. Different etiologies are suggested in today’s literature, such as abnormal host inflammatory reaction to intestinal bacteria, parasitic antigens and dietary components. Could gluten, being the known cause of coeliac disease in humans and gluten-sensitive enteropathy in Irish setter dogs, be involved in the aetiology of this dreadful disease in horses? 2 THE POTENTIAL ROLE OF GLUTEN IN EQUINE INFLAMMATORY SMALL BOWEL DISEASE ABSTRACT Background Equine inflammatory small bowel disease (ISBD) is an idiopathic pathologic condition of the small intestine characterised by substantial reduction of the available absorptive surface area. Signs include a dull hair coat, weight loss, recurrent colic and at times soft faeces, depression and oedema. ISBD is a rare disease that in recent years seems to be increasing in frequency. Different aetiologies are suggested in today’s literature, such as abnormal host inflammatory reaction to intestinal bacteria, parasitic antigens and dietary components. Aims To clarify the role of gluten in equine ISBD, aiming at improved diagnostic and t reatment modalities. To find out if there is an analogy between coeliac disease in humans and ISBD in horses. Methods Comparing different tests: the blood samples of 3 different groups (ISBD patients (n=12), gluten rich controls (n=22) and gluten-free controls (n=25)) were ELISA tested for IgA antibodies against E. coli, human recombinant tissue-transglutaminase (rh-tTGA), guinea pig tissuetransglutaminase (gp-tTGA), antigliadin, deamidated-gliadin-peptides (anti-DGP) and, by using IFT, antibodies against endomysium (EmA). Differences between groups were statistically compared by means of the Mann-Whitney U-test. ρ values < 0,05 were considered significant. One patient was followed after adjustment to a gluten-free diet period for 6 months. Results Both ISBD patients and the gluten-rich controls had significant ( ρ < 0.0004) higher rh-tTGA than the gluten-free controls. Concentrations of anti-DGP antibodies were significantly ( ρ = 0.024) higher in ISBD patients then in the gluten rich controls. The ELISA’s for gp-tTGA, antigliadin antibodies and the IFT for EmA’s were inconclusive as no clear relation was found between these and the use of gluten or ISBD. The patient, followed after a gluten-free diet period of 6 months showed reduced concentrations of all measured serological coeliac disease parameters. Conclusion This is the first study to investigate the potential role of gluten in the aetiology of equine inflammatory small bowel disease. On the basis of these data it is not possible to draw clear conclusions on the role of gluten in equine inflammatory small bowel disease yet. But, the finding that rh-tTGA and DGP antibody concentrations are raised in horses fed a gluten-rich diet suggest an immune-stimulatory effect of gluten that could play a role in the aetiology of ISBD. The case, showing both clinically as well as serological improvement after a gluten-free diet supports this possibility. However, further research is needed to clarify the specifics. 2|Page 3 THE POTENTIAL ROLE OF GLUTEN IN EQUINE INFLAMMATORY SMALL BOWEL DISEASE PREFACE This research project was carried out within the study of Veterinary Medicine at Utrecht University. The study was performed in joint venture with the VU University Medical Center’s Research Institute for Cancer and Immunology, the Department of Pathology and the Department of Gastroenterology and Hepatology, Amsterdam, The Netherlands. The research was executed to get more knowledge about the potential role of gluten in the aetiology of equine inflammatory small bowel disease. 3|Page 4 THE POTENTIAL ROLE OF GLUTEN IN EQUINE INFLAMMATORY SMALL BOWEL DISEASE CONTENTS Content Abstract Preface Contents Part 1: Introduction and background 1.1 Equine inflammatory small bowel disease 1.2 Coeliac disease in humans 1.3 Gluten-sensitive enteropathy in Irish Setter dogs 1.4 Gluten 1.5 Aim of the study 1.6 Hypothesis Part 2: Materials and methods 2.1 Animal selection 2.2 Sampling 2.3 Adaption of human coeliac related ELISA’s for testing equine ISBD patients 2.4 Histopathology 2.5 Statistical analysis 2.6 Clinical trial: measuring the effects of a gluten-free diet Part 3: Results 3.1 Adaption of human coeliac related ELISA’s for testing equine ISBD patients Page 2 3 4 5 5 7 10 11 12 12 13 13 14 14 16 16 16 17 17 Goat anti horse IgA:HRP testing 17 ELISA: IgA antibodies against E. coli 18 ELISA: Antibodies against recombinant human and guinea pig tissuetransglutaminase 19 ELISA: Antibodies against gliadin 22 ELISA: Deamidated gliadin antibodies 23 IFT: Anti-endomysium antibodies 24 3.2 Histopathology 3.3 Clinical trial: measuring the effects of a gluten-free diet Part 4: Discussion Part 5: Conclusion Acknowledgments References Abbreviations Annexes 1-9 25 26 28 31 32 33 34 34 4|Page 5 THE POTENTIAL ROLE OF GLUTEN IN EQUINE INFLAMMATORY SMALL BOWEL DISEASE PART 1: INTRODUCTION AND BACKGROUND Inflammatory small bowel disease is a dreadful disease, both for horses as well as for humans. The number one cause of inflammatory small bowel disease in humans is known to be an intolerance to gluten, the main substance in wheat, barley and ray. Since the uniqueness of man, in comparison to non-human mammals, is becoming more foggily every day, except maybe for their “sophisticated spoken language” (Jane Goodall), why could not gluten be a cause of this idiopathic disease in equines? Earlier research suggests a dietary component as a possible cause.7 Originally, horses are steppe animals that used to spend most of the day searching for grasses and herbs to eat. This feeding pattern is still visible in the way the equine digestive system is build: the relatively small stomach, the highly developed small intestine and the large caecum. Nowadays these horses have become major athletes whose energy requirements are met by a diet of highly concentrated power feed and hay. Researchers have shown that almost all variants of concentrate contain seeds of the agricultural grown cereals; wheat, barley and rye. 5 And these components contain gluten proteins. Gluten is the known trigger of, next to human coeliac disease, glutensensitive enteropathy in the Irish setter dog. In analogy with both diseases this study was carried out to learn more about the potential role of gluten in equine inflammatory small bowel disease. A rare idiopathic disease that, in recent years, seems to be increasing in frequency. Because of their broad knowledge about coeliac disease and their wide range in human coeliac disease diagnostic tests this study was carried out at the VU University Medical Center in Amsterdam. So, what is known already? 1.1 Equine inflammatory small bowel disease Epidemiology Inflammatory small bowel disease (ISBD) is an idiopathic pathologic condition of the small intestine characterised by substantial reduction of the available absorptive surface area. 5,6 ISBD is a rare disease that, in recent years, is diagnosed more frequently in the Equine Clinic of the Utrecht University. Different aetiologies are suggested in today’s literature, such as abnormal host inflammatory reaction to intestinal bacteria, parasitic antigens and dietary components. 7 Causation and types of inflammatory bowel disease in the horse The disease is characterized by villous blunting to atrophy and crypt hyperplasia. Histopathologically different types of ISBD are distinguished depending on the cell type that infiltrates the gut: Eosinophilic enteritis and multisystemic eosinophilic epitheliotrophic disease Eosinophilic enteritis is recognized as diffuse inflammatory cell infiltration of the small intestinal mucosa with eosinophils and lymphocytes. Horses of any sex, age, or breed may be affected with eosinophilic enteritis, but it seems most common in young (2-4 years of age) Standardbred and Thoroughbred horses. Recurrent colic is a common clinical sign with this form of inflammatory bowel disease, and the disease may be diffuse or focal. Circumferential mural bands can form because eosinophilic enzymes stimulate mural fibrosis that partially obstructs the lumen of the small intestine. This obstruction can lead to low-grade chronic colic or result in an acute episode if significant obstruction and distension occurs. Other findings include mucosal ulceration, enlargement of ileal Peyers patches, and mesenteric lymphadenopathy.7 5|Page 6 THE POTENTIAL ROLE OF GLUTEN IN EQUINE INFLAMMATORY SMALL BOWEL DISEASE The cause of this form of inflammatory bowel disease is thought to be a type I hypersensitivity reaction possibly caused by inhaled, dietary, or parasitic antigens. Therefore elimination of these antigens is a necessary part of the treatment plan. Diet change, anthelmintics, and corticosteroids are all used for treatment of eosinophilic enteritis. Treatment options are discussed in more detail in a later section. Most of the current literature reports that treatment usually is unsuccessful, but occasionally horses do respond favourably.7 A subset of affected horses also suffer from eosinophilic infiltration of other organs and tissues including the skin, liver, pancreas, oral cavity, oesophagus, lungs, and mesenteric lymph nodes. This more severe form of the disease is known as “multisystemic eosinophilic epitheliotrophic disease”.7 Granulomatous enteritis Granulomatous enteritis is characterized by lymphoid and macrophage infiltration of the mucosal lamina propria with variable numbers of plasma cells and multinucleated giant cells. There usually is marked villous atrophy, and the ileum typically is the most severely affected portion of the gastrointestinal tract. This condition is similar to Crohn’s disease in humans and Johne’s disease in cattle. The cause of Johne’s disease in cattle is Mycobacterium avium ssp. paratuberculosis.7 Horses diagnosed with granulomatous enteritis can be of any age, sex, or breed, but young Standardbred horses, 4 years old or younger, are over-represented, and there seems to be a familial predisposition. One study showed that more than 80% of the cases of granulomatous enteritis in horses were in Standardbreds. As with the other forms of ISBD, the cause is unknown.1,7 Possible causes include an abnormal host inflammatory reaction to intestinal bacteria or dietary components. Aluminum exposure via invading microorganisms, particularly parasites, also has been linked to granulomatous enteritis in horses.7, 13 Lymphocytic-plasmacytic enteritis Lymphocytic-plasmacytic enteritis is characterized by excessive infiltration of lymphocytes and plasma cells in the lamina propria of the gastrointestinal tract with the absence of granulomatous change. There is no age, breed, or sex predilection for this form of ISBD. It has been suggested that this condition may be an early stage of intestinal lymphosarcoma.7 Lymphosarcoma Intestinal lymphosarcoma can affect horses of any breed, sex, or age and has been reported in a horse with selective IgM deficiency. Lesions can be primary or secondary metastases from another site, most commonly mediastinal lymphosarcoma. Horses present with recurrent colic and weight loss, which can be acute despite the progressive nature of the disease process. The presentation of the disease may range from discrete tumors to diffuse infiltrates (Fig. 1). Additionally, enlarged mesenteric lymph nodes infiltrated by malignant cells may be detected. Mucosal ulcers may contribute to protein loss in horses with lymphosarcoma. Anaemia and thrombocytopenia are common, and lymphocytosis is rare. The prognosis for this form of IBD is poor, because horses usually present in an advanced stage of the disease.7, 16 Fig. 1. Small intestinal lymphosarcoma. A discrete nodule within the small intestine of a 5- year-old Warmblood gelding. The horse presented with acute colic necessitating surgical intervention. The affected portion of small intestine was resected. No additional lesions were found during surgery, but biopsy of a mesenteric lymph node revealed metastasis had already occurred. 7 Fig. 2. Abdominal ultrasound identifying thickening of the wall of the small intestine. 8 6|Page 7 THE POTENTIAL ROLE OF GLUTEN IN EQUINE INFLAMMATORY SMALL BOWEL DISEASE Clinical aspects Clinical signs of ISBD include a dull hair coat, weight loss (despite a good appetite), oedema and at times soft faeces, depression and occasionally (recurrent) colic. The condition affects both young and adult horses. 5 Diagnosis The tentative diagnosis is based on the clinical signs and physical examination. By rectal exploration small bowel loops will be palpable. Haematology may show anaemia and slight increases or decreases in white blood cell counts. Blood biochemistry shows a normal to decreased total protein concentration and decreased albumin concentration. Additionally a percutaneous ultrasound can be made to determine the thickness of the wall of the small intestine usually revealing its thickening (Fig. 2). One can also perform an intestinal absorption test or glucose tolerance test. 5 The diagnosis is confirmed by either a trans-endoscopic duodenal or a laparoscopic biopsy and subsequent histopathology. The type of ISBD is based on the degree of inflammation and the predominant type of infiltrating leucocyte. 7 In the same animal the staging of the pathological changes may differ in different regions of the small and/or large intestines, thus influencing the severity of clinical signs and absorption findings.5 Common treatment If the diagnosis is confirmed there may be different treatment options. Focal lesions can be surgically removed and multifocal or diffuse changes can be treated with corticosteroids or metronidazole, an anti-microbial agent with anti-inflammatory effects (Table 1.). It is also recommended to adjust the diet to short-fibre roughage instead of long-fibre, because of the altered motility of the intestine. 5,7 In general, long-term treatment of ISBD in horses is reported to be unsuccessful. 7 Table 1. Reported treatment options used in the management of infiltrative intestinal disease in horses. 2,7 Drug Dexamethasone Prednisolone Metronidazole Dose 0,02-0,2 mg/kg 0,2-4,4 mg/kg 15 mg/kg Route PO, IM, IV PO PO Frequency q 24 h q 12-24 h q 6-8 h Prognosis and complications The prognosis of a patient with ISBD varies by type. Eosinophilic granulomatosis has the most favourable prognosis, i.e. 60-70% chance of recovery. Granulomatous enteritis has less than 50% chance of healing and lymphocytic plasmacytic enteritis has a very poor prognosis. 5 1.2 Coeliac disease in humans Epidemiology A possibly similar disease to equine ISBD in humans is coeliac disease. Coeliac disease (CD) is a chronic inflammatory disorder of the small bowel induced in genetically susceptible people. CD is characterized by flattened villi on the small bowel mucosa and nutrient malabsorption, and is induced by proline-rich and glutamine-rich proteins (gluten) in wheat, rye, and barley and in combination with cofactors related to drugs (interferon α), intestinal infections and infant feeding practices. Epidemiological studies in first world countries report that the prevalence of CD disease is around 1:100. 4 7|Page 8 THE POTENTIAL ROLE OF GLUTEN IN EQUINE INFLAMMATORY SMALL BOWEL DISEASE Causation Genetic linkage studies show that the disease is strongly associated with HLA -DQ genes. Most patients carry the DQ2 variant and others carry a variant of DQ8 (HLA-DQ genes are part of the major histocompatibility complex type 2 on antigen presenting cells). Other environmental cofactors known to enhance gluten immunogenicity are interferon alpha and rotavirus infections.4,14 Pathophysiology The coeliac lesions develop by a T-helper-cell type 1 response. After gluten peptides crossed the epithelium into the lamina propria, they are deamidated by tissue transglutaminase and then presented by DQ2+ or DQ8+ antigen-presenting cells to pathogenic CD4+ T cells. The CD4+ cells drive the T-helper-cell type 1 response which leads to intraepithelial and lamina propria infiltration of inflammatory cells, crypt hyperplasia and villous atrophy .4 [Intermezzo: T-helper-cell type 1 response: CD4+ cells produce interferon gamma which leads to macrophage activation and the CD40 ligand produced causes B cell proliferation and immunoglobulin A secretion as well macrophage activation.] Gut permeability is enhanced in coeliac patients and gluten can reach the lamina propria through different routes. Investigators have described a paracellular route, as a consequence of impaired mucosal integrity, a transcellular route, based on interferon-ɣ-dependent transcytosis and a protected transport pathway, which is driven by retrotranscytosis of secretory IgA through transferring receptor CD71, that promotes the influx of intact and thus harmful, gluten peptides.4 Tissue transglutaminase is a calcium-dependent, ubiquitous enzyme that catalyses the posttranslational modification of proteins and is released during inflammation . It could have at least two crucial roles in coeliac disease: as the main target autoantigen for antiendomysial antibodies and hTTG (human tissue transglutaminase) antibodies, and as a deamidating enzyme that raises the immunostimulatory effect of gluten. Expression and activity of tissue transglutaminase are raised in the mucosa of patients with CD, where, by deamidating glutamine to glutamic acid, this enzyme makes gliadin peptides negatively charged and therefore more capable of fitting into the pockets of the DQ2/DQ8 antigen-binding groove. 4 In the mucosa of patients with active coeliac disease, gluten-reactive CD4+ T cells produce several pro-inflammatory cytokines, interferon ɣ being dominant, that trigger various effector mechanisms including raised secretion of tissue-damaging matrix metalloproteinases and heightened cytotoxicity of intraepithelial lymphocytes against enterocytes with increased enterocyte apoptosis and villous flattening. 4 Some gluten peptides can directly induce mucosal damage via a non-T-cell dependent pathway (innate response). 4 Clinical aspects Although CD affects approximately 1% of the population of first world countries, most affected individuals remain undiagnosed. This probably reflects the fact that patients with CD can manifest a spectrum of intestinal and/or extraintestinal symptoms. In some cases, they can be relatively asymptomatic, with their disease first being detected by antibody screening because they were identified as being at high risk of developing CD (for example, by being a family member of an affected patient). 14 Symptomatic patients complain about dyspepsia, abdominal discomfort and bloating, unexplained anaemia or it manifests with evident symptoms of malabsorption such as diarrhoea, steatorrhoea, weight loss, cramps, tetany and peripheral oedema.4 8|Page 9 THE POTENTIAL ROLE OF GLUTEN IN EQUINE INFLAMMATORY SMALL BOWEL DISEASE Diagnosis Coeliac disease is diagnosed based on the symptoms, serology and histology. Endoscopic two major changes can be identified, namely the disappearance or reduction of the Kerckring folds and the scalloped configuration of reduced folds. 20 Serological there are different enzyme-linked immunosorbent assay’s (ELISA) available with high sensitivity and specificity. The VU University Medical Center Immunology diagnostics lab uses inhouse ELISA’s to test for either IgA or IgG antibodies against recombinant human tTG (specificity 98-100% and sensitivity 92-96%), gliadin antibodies (showed a sensitivity and specificity range from 31% to 100% and 57% to 100% 21) and an in-house for IgA antibodies against E. coli to rule out a IgA deficiency, which has a prevalence of around 1:400.17 Additionally there is an ELISA available to test for antibodies against deamidated gliadin. A variant to the recombinant human tTG antibody ELISA is one that uses guinea-pig tTG derived from the liver. The VUmc also has an IgA-class anti-endomysium immunofluorescence antibody test on hand, by which an indirect immunofluorescence analysis is performed using unfixed cryostat sections of monkey oesophagus (showing a sensitivity and specificity range from 85% to 100% and 95% to 100% 21). Histological the diagnosis of CD is based on the presence of characteristic lesions in smallintestinal biopsy samples. Major features of mucosa suggestive of coeliac disease are: proximal small bowel involvement, decreasing distally and in some cases patchy distribution. Mucosal architectural changes include villous atrophy, crypt hyperplasia, thickening of the basement membrane under the surface epithelium and a reduced numbers of goblet cells. Mucosal inflammation is revealed by increased intraepithelial lymphocytes and an influx of immune cells in the lamina propria. Enterocyte changes include cuboidal morphology, loss of basal nuclear orientation and cytoplasmic vacuoles. Biopsy samples are usually taken from the distal duodenum and the Marsh-Oberhuber classification is used to grade the severity of the lesions (Table 2 & Fig. 3). 4,19 Table 2. The modified Marsh–Oberhuber classification.19 IEL count* Crypt hyperplasia Villous atrophy Marsh 0 Marsh 1 Marsh 2 >30/100 + Marsh 3 3a >30/100 + <30/100 − >30/100 − 3b >30/100 + 3c >30/100 + − − − Mild Moderate Total Pre‐infiltrative Infiltrative Infiltrative‐hyperplastic Flat destructive IEL= intraepithelial lymphocytes; *= Number of intraepithelial lymphocytes per 100 enterocytes. Minor lesions, such as increased intraepithelial lymphocytes, have a low specificity for diagnosis of CD since a wide variety of immunologic stimuli can raise intraepithelial lymphocyte numbers. Therefore diagnosis of CD is confirmed only by clinical symptoms, a positive serology, or histological improvement after commencement of a gluten-free diet. 4, 26 Fig 3. Marsh–Oberhuber type 1 and type 3 lesions.19 Additionally, HLA typing for HLA-DQ2/DQ8 can be performed which is, when negative, almost absolute in ruling out coeliac disease in high-risk individuals such as first-degree relatives and patients with type-1 diabetes. 4 9|Page 10 THE POTENTIAL ROLE OF GLUTEN IN EQUINE INFLAMMATORY SMALL BOWEL DISEASE Treatment The only proven treatment for coeliac disease is strict and life-long adherence to a gluten-free diet. 4 Complications Known complications to coeliac disease are non-hodgkin lymphoma, refractory coeliac disease, ulcerative jejuno-ileitis, and enteropathy-associated T-cell lymphoma. The latter is of importance, given the fact that the histopathology is similar to the alimentary form of malignant lymphoma in the horse. So this may be another interesting research topic. 4 1.3 Gluten-sensitive enteropathy in Irish Setter dogs Epidemiology Gluten-sensitive enteropathy in dogs has some similarities to coeliac disease, but the severity of intestinal damage and clinical signs tends to be less marked then in humans. Wheat sensitivity has been confirmed by morphologic and biochemical examination of jejunal biopsies obtained during challenge studies performed on a litter bred from affected dogs and reared on a normal wheat-containing diet. 9 Causation The disease is characterized by partial villous atrophy and increased intraepithelial lymphocytes. The studies described above introduced the possibility that there might be an age-related delay in the expression of aminopeptidase N, the most abundant brush border peptidase. This could be important, since severely reduced levels of this enzyme might allow high concentrations of potentially toxic gluten peptides to reach the lamina propria due to defective degradation, resulting in development of hypersensitivity. A permeability disorder could have similar consequences. 9 A study performed on a litter of affected animals has shown that the dogs reared and kept on a cereal-free diet until 12 months of age appeared to be resistant to gluten challenge. The litter mates kept on a normal diet until 12 months of age, followed by a period of a cereal-free diet and then back on a normal diet 6 weeks after the introduction of a cereal-free diet failed the gluten challenge. It resulted in clinical relapse manifested with diarrhea and weight loss. This suggest that there might be a critical age for the introduction of gluten to the diet beyond which gluten sensitivity does not develop. 9 Clinical aspects Affected dogs typically present with poor weight gain or weight loss, in most cases accompanied with chronic diarrhea, and clinical signs are often first observed at approximately 6 months of age. 9 Diagnosis Dietary sensitivity may be suspected from the clinical history, which may suggest an association between a specific dietary antigen, such as gluten, and the presence of clinical signs. Subsequent investigations should exclude intestinal parasites and pathogens, partial intestinal obstruction, systemic disease, exocrine pancreatic insufficiency, and bacterial overgrowth. Assessment of the intestinal mucosa is then needed to show that a specific dietary antigen causes intestinal damage, which is likely to be the most severe in the proximal small intestine, where antigen concentration is the highest. The assessments of intestinal damage need to be repeated following exclusion diet and challenge in order to make a definitive diagnosis. 9 10 | P a g e 11 THE POTENTIAL ROLE OF GLUTEN IN EQUINE INFLAMMATORY SMALL BOWEL DISEASE Treatment An exclusion diet consisting of a selected protein source should be used as trial therapy in suspected cases, and should be fed for a period of at least 6 weeks. Boiled white rice or potato is generally a suitable carbohydrate source, and lamb or chicken is often used as a protein source. Oral prednisone, 0,5 to 1 mg/kg twice daily for two to 4 weeks, followed with a reducing dose at 2-weeks intervals, may assist some cases if dietary sensitivity in the initial response to exclusion diet is disappointing. 9 Prognosis After being put on a strict long-term gluten-free diet the dogs should improve dramatically within a few weeks. The diarrhea should resolve and they should gain weight. Within the year no recurrence of diarrhea has been reported. 15 1.4 Gluten The history of gluten The discovery in the Neolithic age, beginning about 9500 BC, of ways to produce and store food has been the greatest revolution mankind ever experienced. Archeological findings suggest that this revolution was initiated by the observations made by woman. The woman carried the daily burden of collecting seeds, herbs, roots and tubers. During the excavation of roots and tubers she probably observed the fall of grain seeds on the ground and their penetration into the soil with rain. Finding new plants in the places which she herself digged with a stick, lead to the connection between fallen seeds and new 'cultivated' plants. 18 The origin of farming practices should be located in South East Asia. In the highlands of this area the neo-thermal switch caused abundant rainfall. In all of this area existed, and still exists, a wide variety of wild cereals, sometimes in natural extended fields, induced by the rainfalls. Triticum Dicoccoides (wheat) and Hordeum Spontaneum (barley) were common and routinely collected by the local dwellers. The wild cereals had very few seeds (2-4) that fell easily on the ground on maturation. 18 The people from the Uadi el-Natuf Tell of South East Asia (7800 B.C.) provided the first traces of the gradual shift from hunters to grain cultivators. Their economy was based on the hunt of the gazelle, but their diet also included collected grain seeds. These gradually came to form a substantial proportion of their energy input, as cultivation practices ensued. Around 5000 B.C. wild animals, more rare due to incoming drought, formed only 5% of the daily diet, while cereals and farmed animals became a sizeable part of it. The farmer's expansion lasted from 9000 B.C. up to the 4000 B.C. when they reached Ireland, Denmark and Sweden covering most cultivable lands in Europe. The expansions followed the waterways of Mediterranean and of Danube across the time of Egyptians, Phoenicians, Greeks and Romans. 18 Early bread making activities pushed towards grains that contained greater amounts of a structural protein, which greatly facilitated the bread making: the gluten. Over the last 200 years of our modern age active genetic selection, and genetic manipulation, have changed the aspect of the original Triticacee enormously: from few grains and little gluten to great wheat harvests very enriched in gluten (50% of the protein content), well adapted to cultivation practices and ready to be handled by monstrous machineries. 18 The chemistry of gluten proteins Gluten can be defined as the rubbery mass that remains when wheat dough is washed to remove starch granules and water-soluble constituents. These gluten proteins have different solubility’s in alcohol-water solutions and, thus, can be roughly separated into two fractions - gliadins and glutenins. Gluten proteins have a complex chemistry and are responsible for determining the unique baking quality of wheat by conferring water absorption capacity, cohesivity, viscosity and elasticity on dough. 10 11 | P a g e 12 THE POTENTIAL ROLE OF GLUTEN IN EQUINE INFLAMMATORY SMALL BOWEL DISEASE Analysis of gliadin has identified more than a hundred components that can be grouped into four main types (ω5-,ω1,2-, α/ß-, ɣ-gliadins). The immunogenicity and toxicity of several gliadin epitopes has been established for humans. A distinction exists between a peptide being immunogenic or toxic. Glutenins can be divided into groups of high molecular weight and low molecular weight. Immunogenicity and toxicity in the high-weight group has been shown. Storage proteins (prolamines), with a similar amino acid composition to the gliadin fractions of wheat, have been shown in barley (hordeins) and rye (secalin), and show a close relation to the taxonomy and toxic properties of wheat cereal that affect people with coeliac disease. Although several gluten epitopes are immunostimulatory, some are more active than others. 4 Gluten in the equine diet To meet the energy requirements of today’s equine athlete concentrate feeds are given. As mentioned before most regular concentrate feeds contain wheat, barley and rye, the main carriers of gluten. Some specialised concentrate feeds are known to consist of up to 25-30% of barley. Horses that are housed in a field year round or are fed a diet consisting of only hay or silage are thought be gluten-free (or at least gluten-poor), since it are mainly the seeds of agricultural grown cereals that contain gluten. 1.5 Aim of the study 1. To clarify the role of gluten in equine inflammatory small bowel disease, aiming at improved diagnostic and treatment modalities. 2. To find out if there is an analogy between coeliac disease in humans and inflammatory small bowel disease in the horse. 3. To develop ELISA tests as additional diagnostic tool in inflammatory small bowel disease. 4. If the study reveals a correlation between gluten and ISBD in horses this could provide some further understanding of the characteristics of the disease for both human and veterinary medicine. 1.6 Hypothesis The hypothesis of this study is that: equine patients suffering from ISBD will have higher levels of human recombinant tissue-transglutaminase (rh-tTGA), guinea pig tissue-transglutaminase (gptTGA), antigliadin, deamidated-gliadin-peptides (anti-DGP) and anti-endomysium (EmA) antibodies compared to the two different control groups. 12 | P a g e 13 THE POTENTIAL ROLE OF GLUTEN IN EQUINE INFLAMMATORY SMALL BOWEL DISEASE PART 2: MATERIALS AND METHODS We’ve subjected equine ISBD patients to human coeliac disease diagnostics; to compare the results two different control groups without ISBD have been tested as well: one group being on a gluten-rich diet, the other on a gluten-free diet (or at least gluten-poor). 2.1 Animal selection Patients Twelve horses with signs of ISBD were referred to the Department of Equine Sciences, Section of Internal Medicine, Utrecht University in the years 2010 and 2011. The clinical history was taken, a physical examination was performed and peripheral venous blood was collected for routine haematological and biochemical examination and further research. The (tentative) diagnosis of inflammatory small bowel disease was based on the clinical signs, physical examination, abnormal findings during rectal exploration (thickening of the small intestine), blood chemistry and a percutaneous ultrasound. Haematocrit and lymphocytes were determined as well as albumin and total protein. In 7 out of 12 cases an oral glucose tolerance test was performed and 6 out of 12 cases were diagnosed based on histological examination of gastroduodenoscopyassisted biopsies taken from the proximal duodenum. Breed, gender, age, sampling date and findings by examination are summarized in Table 3. The patient group consists of 5 mares, 6 geldings and 1 stallion, ranging in age from 8 till 18 years (mean 10,8 ± 3,48 SD). Except for 1 Friesian all horses are Dutch Warmbloods. All samples were taken between February 2010 and January 2011 (Annex 1). Table 3: Background of the 12 patients suspected to have ISBD ID No Breed 1 2 3 4 KWPN KWPN KWPN Frisian Sex Age (yea rs) 5 6 7 8 9 10 11 12 gelding gelding mare Clinical presentation Ht Lymphoc ytes (L/L) ( x*10^9/L) Total protein ( g/L) Albumin (g/L) Percutaneous ultrasound / rectal exam (+) Glucose tolerance test Histopat hology 18 5 7 Anorexia, fever 0,33 1,1 73 33 + nd nd Weight loss 0,36 1,2 58 34 + 63% enteritis Weight loss 0,33 1,1 73 33 + Normal Mild LE Reduced 0,34 5,3 58 34 + 47% nd performance, mare 11 underweight KWPN gelding 8 Recurrent colic 0,30 1,3 60 33 + nd Mild LPE KWPN mare 9 Recurrent colic 0,33 1,4 51 31 5-6mm, + Normal nd KWPN Weight loss, 0,41 2,4 66 35 + 40% Broaden reduced villi, mild stallion 14 performance atrophy KWPN gelding 11 Colic 0,34 1,5 63 35 4,5mm, + nd nd KWPN mare 14 Recurrent colic 0,38 2,0 64 38 + Lowered LE KWPN gelding 14 Recurrent colic 0,40 1,3 72 36 nd Lowered nd KWPN gelding 9 Recurrent colic 0,33 1,2 62 38 + nd Mild LPE KWPN mare 10 Recurrent colic 0,37 2,8 63 37 + nd nd KWPN= Dutch Warmblood horse; LE= Lymphocytic Enteritis; LPE= Lymphocytic-Plasmacytic Enteritis; += distended small intestine are palpable and/or visible on ultrasound; nd= not determined In-house: gluten-rich controls 22 “in-house” controls were used for this study. During the experimental period all these controls were housed at the Department of Equine Sciences, Utrecht University. They were fed with hay and concentrate according to their nutritional needs. Their mean age is 10,9 ± 4,46 SD years. The 22 controls consist out of 19 Dutch Warmbloods, 2 Shetland ponies and one Standardbred. 19/22 are mares, 3/22 are geldings. All samples were taken between February 2010 and January 2011 (Annex 1). 13 | P a g e Sampling date 160210 040210 020210 160210 040210 180610 080610 060610 150410 200810 101210 060111 14 THE POTENTIAL ROLE OF GLUTEN IN EQUINE INFLAMMATORY SMALL BOWEL DISEASE Wild controls: suspected gluten-free population A group of 25 Shetland ponies that are housed, year round, in nature reserve park Zeepeduinen in Zeeland, the Netherlands were used as a gluten-free control group. They are most presumably living a gluten-poor live, since their diet consists out of wild, non-agricultural grasses and herbs. All 25 gluten-poor controls are mares and their age ranges from 1-27 years (mean unknown). All samples were taken the 6 th of October 2010 (Annex 1). Histology The duodenal biopsies, taken by endoscopy, from patients after admittance between 2010 and 2011, were used for histopathological evaluation by both a veterinary and a human pathologist. For comparative histology, between humans and horses, old, paraffin fixed, sections of affected small bowel were used. These sections were collected, on necropsy, between 1993 and 2004. These equine patients were diagnosed with eosinophilic enteritis, granulomatous enteritis, lymphocytic-plasmacytic enteritis or lymphosarcoma. Histopathology rapports are available. (Annex 7) 2.2. Sampling Either plasma (using lithium-heparin tubes) or serum (using serum collection tubes) was collected from peripheral venous blood. Buffy coats were collected using EDTA blood collection tubes. Both samples were centrifuged after and the plasma/serum respectively buffy coats were stored at -27°C. The collected biopsies from duodenal mucosa were fixed in 10% formalin and processed to paraffin wax, cut at 4 mm and stained with haematoxylin and eosin (HE). 2.3 Adaption of human coeliac related ELISA’s for testing equine ISBD patients Human coeliac disease diagnostics; enzyme-linked immunosorbent assay’s (ELISA) have been altered for detection of equine IgA antibodies against E. coli, recombinant human tissuetransglutaminase, guinea pig tissue-transglutaminase, gliadin and deamidated gliadin. Table 4: Antibodies used for ELISA testing. Marker Name Source Specificity Format Goat anti AAl34P AbD Serotec IgA HRP horse IgA:HRP Goat anti AAl34F AbD Serotec IgA FITC horse IgA:FITC HRP= horseradish peroxidise, FITC= fluorescein isothiocyanate isomer 1 Isotype Polyclonal IgG Target species Equine Polyclonal IgG Equine Goat anti horse IgA:HRP testing To determine whether the goat anti horse IgA:HRP (Table 4.) could be used as a conjugate and at which dilution, an in-house ELISA for E.coli antibodies was performed. Since E. coli is a common pathogen all horses are suspected to carry antibodies. The goat anti horse IgA:HRP conjugate was tested in three dilutions: 1:1000, 1:10.000 and 1:100.000. The serum was diluted to 1:20, 1:40 and 1:80. TMB was initially used as a substrate for the enzyme-substrate reaction. After 15 minutes, when staining had occurred, the reaction was stopped using H 2SO4. The degree of staining was determined using a spectrophotometer (ELISA reader TECAN Sunrise, 450nm). The extinctions are thought to reflect the antibody concentration. 14 | P a g e 15 THE POTENTIAL ROLE OF GLUTEN IN EQUINE INFLAMMATORY SMALL BOWEL DISEASE ELISA: IgA antibodies against E. coli Because the ELISA’s mentioned above are based on IgA antibodies, all sera were teste d for the presence of IgA, using an E. coli antibody ELISA, to rule out IgA deficiency. The concentration antibodies against E. coli is quantitatively determined using 96-wells microtitre plates (Nunc Maxisorp©), which were coated with E. coli strain EB1. After washing (ELx 405 Auto Plate washer, Bio-Tek Instruments) the still free binding sites, on the microtitre plates, were filled using bovine serum albumin (BSA). Next the serum was put on to the plate in an 1:20 dilution. If the serum contains antibodies against E. coli these will bind to the plate. After washing, the plates were incubated with the goat anti horse IgA:HRP. After washing again the attached antibodies were made visible following an enzyme-substrate reaction, using OPD. After 15 minutes the reaction was stopped using H 2SO4. The degree of staining was determined using a spectrophotometer, at 492 nm. The extinctions are thought to reflect the antibody concentrations against E. coli. Patient No. 10 is used for a calibration curve and as a positive standard (per definition containing 100 AU E.coli antibodies/ml). The exact protocol of this in-house ELISA is retained by the VU medical center. ELISA: Antibodies against recombinant human and guinea pig tissue-transglutaminase The most important serological parameter to diagnose human coeliac disease is tissue transglutaminase antibodies (TGA). The TGA concentration is quantitatively determined based on the TGA binding to either rh-tTG or to purified guinea pig tTG. 96-wells microtitre plates were used, which were coated with rh-tTG (source: Diarect) or gp-tTG (source: Sigma) according to standard operation procedures. After washing the still free binding sites, on the microtitre plates, were filled using bovine serum albumin (BSA). Next the serum was put onto the plate. The serum was diluted from 1:20, 1:40, 1:80 till 1:160 in PBS with 1% BSA and 0.05% Tween 20 and pre-incubated at room temperature for 30-60 min to allow potential anti-BSA to bind to the BSA . If the serum contains TGA these will bind to the rh-tTG. After washing, the plates were incubated with the goat anti horse IgA:HRP conjugate, in an 1:5000 dilution. After washing again the attached antibodies were made visible using an enzyme-substrate reaction; reduced from H2O2 till H2O and when oxidized by HRP, using hydrogen peroxidase, the substrate OPD is turned into a colored product. After 15 minutes, when staining had occurred, the reaction was stopped using H2SO4. The degree of staining was determined using a spectrophotometer, at 492 nm. The extinctions are thought to reflect the concentration of TGA. Patient No. 7 is used as calibration curve and as a positive standard (per definition containing 100 AU TGA/ml). The exact protocol of this in-house ELISA is retained by the VU medical center. ELISA: Antibodies against gliadin In addition, to determine whether gliadin antibodies were present in the equine plasma an in house ELISA for antibodies against gliadin was executed. 96-wells microtitre plates were used, which were coated with gliadin (source: Sigma). Next the serum was put onto the plate. The serum was diluted from 1:20, 1:40, and 1:80 till 1:160. If the serum contains antibodies against gliadin these will bind to the plate. Bound antibodies are made visible as described abov e for TGA. Control No. 28 is used for a calibration curve and as positive standard (per definition containing 100 AU gliadin antibodies/ml). The exact protocol of this in-house ELISA is retained by the VU medical center. ELISA: Deamidated gliadin antibodies After tissue transglutaminase transforms the gliadin (glutamin glutamic acid), the remaining gliadin is termed “deamidated” gliadin. A commercial ELISA (source: Euro Diagnostica), based on a set of deamidated gliadin peptides as target, was used for testing antibodies against these deamidated gliadin peptides. 15 | P a g e 16 THE POTENTIAL ROLE OF GLUTEN IN EQUINE INFLAMMATORY SMALL BOWEL DISEASE The 'human' ELISA was adapted for measuring specific horse IgA as described for TGA. A 1:50 serum dilution was used. Unfortunately, the kit was limited, so not all horses were tested. Gluten-rich controls No. 34, 35 and 42 and gluten-free controls 70-75 were not tested. IFT: Anti-endomysium antibodies The VUmc also has an IgA-class anti-endomysium immunofluorescence antibody test on hand, by which an indirect immunofluorescence analysis is performed using unfixed cryostat sections of monkey oesophagus. Oesophagus is used because the endomysium antibodies are directed against proteins in between the smooth muscle cells of the muscularis mucosae, such as tissue transglutaminase. The plasma was put on the 3-wells glasses in a 1:2 dilution. PBS was used as a negative control. If anti-endomysium antibodies are present these will bind to the endomysium during incubation. After washing the goat anti horse IgA:FITC conjugate (table 4) was incubated. The conjugate incubation was tested in three dilutions, 1:20, 1:50 and 1:100. After washing, the glasses were covered, and viewed under a fluorescence microscope, and scored for staining pattern and fluorescence intensity of the muscularis mucosae (as -, +/-, +, ++ or +++). Antiendomysium antibodies are ineffective in detecting individuals with silent or subclinical gluten sensitivity. 21 2.4 Histopathology A human pathologist performed comparison of histopathological biopsies, from equine ISBD patients to human coeliac patients. The sections were fixed in 10% formalin, processed to paraffin wax, cut at 5 µm, stained with HE and examined under a light microscope. 2.5 Statistical analysis During the study all results were analysed using, the statistical analysis specialised software, MedCalc. Because the sample sizes are relatively small and it is not clear if these are samples taken from normally distributed data the Mann-Whitney U-test was chosen to assess the statistical differences. ρ values < 0.05 were considered significant. Pearson’s correlation was used to determine the correlation coefficient between two substrates (TMB and OPD) used. Corrections ELISA testing The extinctions measured by the spectrophotometer were settled with the extinctions of the blanks and the positive standards. As mentioned before, patient No. 10 was used as a positive standard in the antibodies against E. coli ELISA. No.7 is used as a positive standard in both tTG ELISA’s. Gluten-rich control No. 28 was used as a positive standard in the antibodies against gliadin ELISA. Patient No. 10 was used as a positive standard in the antibodies against E. coli ELISA. The extinctions are thought to reflect the concentration of antibodies measured. The positive standards were used to determine a calibration curve, by diluting them from 1:20 till 1:2560. The extinction of the positive standard per definition containing 100 AU/ml. Cut offs were not yet determined in this phase of the study. 2.6 Clinical trial/case study: measuring the effects of a gluten-free diet The owner of patient no. 7, a horse known to suffer from ISBD and with an exceptional high tTGA concentration, was asked to adjust their horse diet to a gluten-free one (Annex 4). Patient no. 7 was diagnosed with ISBD, based on abnormal findings during rectal examination, a lowered glucose tolerance test and histopathological examination of a (duodenal) biopsy by a pathologist. After a dieting period of 6-7 months another plasma sample was collected, from peripheral venous blood using lithium-heparin tubes. This sample was, again, subject of all ELISA tests. 16 | P a g e THE POTENTIAL ROLE OF GLUTEN IN EQUINE INFLAMMATORY SMALL BOWEL DISEASE PART 3: RESULTS 3.1 Adaption of human coeliac related ELISA’s for testing equine ISBD patients Goat anti horse IgA:HRP testing To determine whether the goat anti horse IgA:HRP (Table 5.) could be used as a conjugate in all other ELISA’s and at which dilution, an in-house ELISA for E.coli antibodies was performed. This test was also used to determine which conjugate dilution suited best, 1:1000, 1:10.000 or 1:100.000. Since TMB was initially used as a substrate, extinctions were measured at a wavelength of 450nm and they are shown in table 5. Table 5. Extinction overview antibodies against E. coli ELISA at 450nm. Serum 1:1000 conjugate 1:10.000 conjugate 1:100.000 conjugate Patient 9 1:20 2,542 2,491 1,142 1,01 0,166 0,161 Patient 9 1:40 2,273 2,195 0,767 0,673 0,121 0,114 Patient 9 1:80 1,841 1,766 0,211 0,432 0,09 0,09 Patient 8 1:20 2,775 2,739 1,779 1,788 0,297 0,305 Patient 8 1:40 2,535 2,53 1,116 1,099 0,177 0,181 Patient 8 1:80 2,192 2,211 0,645 0,614 0,117 0,115 Patient 10 1:20 2,778 2,792 2,161 2,119 0,455 0,467 Patient 10 1:40 2,681 2,669 1,757 1,759 0,317 0,315 Patient 10 1:80 2,549 2,487 1,155 1,136 0,202 0,202 Control 30 1:20 2,676 2,64 1,436 1,257 0,208 0,199 Control 30 1:40 2,504 2,41 0,953 0,868 0,141 0,134 Control 30 1:80 2,079 1,924 0,604 0,508 0,092 0,088 Blanco 0,09 0,066 0,043 0,043 0,039 0,037 Blanco 0,073 0,062 0,042 0,047 0,04 0,041 Blanco 0,058 0,056 0,043 0,04 0,052 0,048 Blanco 0,059 0,056 0,043 0,043 0,049 0,047 The extinctions shown in table 5 confirm that the goat anti horse IgA:HRP conjugate works, because staining has occurred, resulting in an extinction measured by the spectrophotometer. Fig. 4 shows the extinction outcome of patient No. 9 for all conjugate and serum dilutions. This demonstrates that the 1:1000 conjugate dilution has the clearest regression curve. Fig. 4: Multiple comparison line graph showing the extinctions per dilution. Outcome extinctions at 3 different dilutions, for both conjugate as plasma. Extinction patient no. 9 17 3 2 *1:1000 1 *1:10.000 0 *1:20 *1:40 *1:80 *1:100.000 Plasma dilution Since the 1:1000 conjugate dilution developed too fast, a 1:5000 conjugate dilution was chosen for all further experiments. 17 | P a g e 18 THE POTENTIAL ROLE OF GLUTEN IN EQUINE INFLAMMATORY SMALL BOWEL DISEASE Because the substrate TMB has shown too much staining too fast, OPD was chosen as an alternative substrate. Pearson’s correlation between TMB and OPD is r= 0,999, with a ρ-value of < 0,0001. So, changing the substrate from TMB to OPD will not influence the overall results. ELISA: IgA antibodies against E.coli To exclude IgA deficiency in the study group all horses were tested for IgA antibodies against E. coli. As shown in Fig. 5 all horses included in this study tested positive for IgA antibodies against E. coli. As suspected, since no solitary IgA deficiency disorder has been described in horses and E. coli is such a common pathogen. It also shows that specific IgA is easily and repeatable detectable in all horses. And that anti-IgA antibodies could be used in further ELISA testing in this study. The range in antibody concentration is shown in fig. 5. n=12 for group 1, n=22 for group 2 and n=25 for group 3. (See also: annex 2) Fig. 5: Multiple comparison (dot and box) graph showing the E. coli antibodies in AU/ml per group. Overview E.coli antibody (IgA) concentrations in arbitrary units (AU) per milliliter per group. 140 P = 0.0015 120 P = 0.5840 P = 0.0001 for group 1+2 vs. 3 P = 0.0004 100 meidan = 93.85 median = 87.00 80 E. coli 60 [ 40 median = 24.10 20 0 1 2 3 group (1=patients, 2=gluten-rich controls, 3=gluten-free controls) Using the Mann-Whitney test for independent samples the following results were found: The ρ-value (P) for group 1 and 2 = 0.5840, since this exceeds the 0.05 = α there is no significant difference measured between E.coli IgA antibody concentrations in horses with ISBD and horses without ISDB on a gluten-rich diet. There is however a significant difference between group 1 and 3 and group 2 and 3, with ρ-values being respectively 0.0015 and 0.0004, both being <0.05. Accordingly, the IgA concentrations against E.coli are significantly higher in horses with ISBD and in the gluten-rich controls than in the gluten-free, wild controls. This implies that the wild living, gluten-free horses have lesser antibodies against E. coli then group 1 and 2, with the lowest concentration being 5.4 AU/ml. In human diagnostics a concentration of 3.0 U/ml is considered weak positive. 18 | P a g e 19 THE POTENTIAL ROLE OF GLUTEN IN EQUINE INFLAMMATORY SMALL BOWEL DISEASE ELISA: Antibodies against recombinant human and guinea pig tissue-transglutaminase (TGA) The TGA concentration is quantitatively determined based on the TGA binding to either rh-tTG or to purified guinea pig tTG. The results of the recombinant human tissue transglutaminase antibody ELISA of horses with ISBD were compared with those of clinically normal horses, both gluten-rich and gluten-free. Results are shown in fig. 6. n=12 for group 1, n=22 for group 2 and n=25 for group 3. (See also: annex 2) Fig. 7 shows the staining of a 96-well microtitre plate after the enzyme-substrate reaction with OPD was stopped using H2SO4. Fig. 6: Multiple comparison (dot and box) graph showing the rh-tTG antibodies in AU/ml per group. Overview rh-tTGA concentrations in arbitrary units (AU) per milliliter per group. 100 patient no. 7 P < 0.0001 for group 1+2 vs. 3 80 60 P = 0.0001 P = 0.2343 40 P = 0.0004 20 median = 12.05 median = 8.40 median = 3.70 0 1 2 3 group (group 1= patients, group 2= gluten-rich controls, group 3= gluten-free controls Using the Mann-Whitney test for independent samples the following results were found: The ρ-value for group 1 and 2 = 0.2343, since this exceeds the 0.05 = α there is no significant difference measured between the rh-tTGA concentration in horses with ISBD and clinically healthy horses kept on a gluten-rich diet. There is however a significant difference between group 1 and 3 and group 2 and 3, with ρ-values being respectively 0.0001 and 0.0004 both being <0.05. Thus the rh-TGA concentrations are significantly higher in horses with ISBD and in the gluten-rich controls than in the gluten-free controls. Remarkable is the, in contrast to other ISBD patients and the gluten-rich controls, repeatable high recorded rh-TGA concentration of patient no. 7: 100 AU/ml. 19 | P a g e 20 THE POTENTIAL ROLE OF GLUTEN IN EQUINE INFLAMMATORY SMALL BOWEL DISEASE Fig. 7: ELISA 96-well microtitre plate showing positive staining. Using a Log transformation, shown in Fig. 8, the differences between groups 1 and 3 and 2 and 3 become even clearer. It shows that ISBD patients do not have an overall higher rh-tTGA concentration than the clinically healthy controls on a gluten-rich diet. Note the clear separation in concentration in the gluten-free population, group 3, with some of them having almost no detectable antibodies at all. Fig. 8: Multiple comparison (dot and box) graph showing the rh-tTG antibodies in AU/ml per group in Log transformation. rh-tTGA concentrations in AU/ml per group (in Log transformation) 100 patient no. 7 10 1 Horizontal reference line. Value = 2,50 0.1 GR no. 35 +42 0.01 1 2 3 group (group 1=patients, group 2= gluten-rich controls, group 3= gluten-free controls) 20 | P a g e 21 THE POTENTIAL ROLE OF GLUTEN IN EQUINE INFLAMMATORY SMALL BOWEL DISEASE The results of the guinea pig tissue transglutaminase antibody ELISA from the horses with ISBD were compared with those of clinically healthy horses, both gluten-rich and gluten-free. n=12 for group 1, n=22 for group 2 and n=24 for group 3. Gluten-free control no. 61 was not determined. Results are shown in fig. 9. (See also: annex 2) Fig. 9: Multiple comparison (dot and box) graph showing the gp-tTG antibodies in AU/ml per group. Overview gp-tTGA concentrations in arbitrary units (AU) per milliliter per group. 100 Patient no. 7 P = 0.9559 for group 1+2 vs. 3 GR controls no. 26 & 32 80 P = 0.3305 P = 0.2343 60 P = 0.4748 40 median = 22.20 median = 19.40 20 median = 15.50 0 1 2 3 group (group 1= patients, group 2= gluten-rich controls, group 3= gluten-free controls) Using the Mann-Whitney test for independent samples the following results were found: The ρ-value for group 1 and 2 = 0.2343, since this exceeds the 0.05 = α there is no significant difference between the gp-tTGA concentration in horses with ISBD and horses without ISDB, kept on a gluten-rich diet. There was also no significant difference found between group 1 and 3 and group 2 and 3, with ρ-values being respectively 0.3305 and 0.4748 both being > 0.05. Summarized: the overall gp-tTGA concentrations are not significantly higher in horses with ISBD and in the gluten-rich controls than in the gluten-free controls so there is no clear relation between gp-tTGA and the use of gluten in horses. Remarkable is the patients median of group 3, m=19.40, being higher than that of group 2, m=15.50. And patient no. 7 that shows to be strongly positive, as are the gluten-rich controls no. 26 and 32. 21 | P a g e [GA] in AU/ml 22 THE POTENTIAL ROLE OF GLUTEN IN EQUINE INFLAMMATORY SMALL BOWEL DISEASE ELISA: Antibodies against gliadin To determine whether significant differences could be found in gliadin antibody concentration between the three study groups an in-house ELISA for gliadin antibodies was performed. The results of the antigliadin antibody (GA) ELISA from the horses with ISBD were compared with those of clinically normal horses, both gluten-rich and gluten-free. n=12 for group 1, n=22 for group 2 and n=25 for group 3. Results are shown in fig. 10. (See also: annex 2) Fig. 10: Multiple comparison (dot and box plot) graph showing the GA in AU/ml per group . Overview GA concentrations in arbitrary units (AU) per milliliter per group. 140 GR no. 32 P = 0.9572 for group 1+2 vs. 3 120 GR no. 28 100 GF no. 54 P = 0.7827 80 P = 0.7981 P = 0.7731 60 40 median = 24.50 median = 23.75 median = 19.95 20 0 1 2 3 group (group 1= patients, group 2= gluten-rich controls, group 3= gluten-free controls) Using the Mann-Whitney test for independent samples the following results were found: The ρ-values are: ρ = 07731 for 1 and 2, ρ = 0.7827 for 1 and 3 and ρ = 0.7981 for 2 and 3. Since none of these are < 0.05, no significant between-group differences could be stated. And there is no clear relation between GA and the use of gluten in horses. Remarkable however are the 2 clinically healthy gluten-rich controls, no. 28 and 32 that are strongly positive for GA and also the gluten-free controls no. 54 and two others who have a high concentration of GA. Patient no. 7 also shows to be strongly positive. 22 | P a g e 23 THE POTENTIAL ROLE OF GLUTEN IN EQUINE INFLAMMATORY SMALL BOWEL DISEASE ELISA: Deamidated gliadin antibodies The results of the deamidated gliadin (DGP) antibody ELISA from the horses with ISBD were compared with those of clinically healthy horses, both gluten-rich and gluten-free. n=12 for group 1, n=19 for group 2 (gluten-rich controls 34, 35 and 42 were left out) and n=19 for group 3 (glutenfree controls 70-75 were left out). Results are shown in Fig. 11 and 12. (See also: annex 2) Fig. 11: Multiple comparison (dot and box plot) graph showing the DGP antibody concentration in AU/ml per group . Overview DGP antibody concentrations in arbitrary units (AU) per milliliter per group. 100 GF no. 59 P = 0.0341 for group 1+2 vs. 3 GR no. 22 + 24 80 60 P = 0.0244 40 P = 0.4410 P = 0.1403 20 median = 5.60 median = 2.60 median = 1.90 0 1 2 3 group (group 1= patients, group 2= gluten-rich controls, group 3= gluten-free controls) Using the Mann-Whitney test for independent samples the following results were found: The ρ-value for group 1 and 2 = 0.4410, since this exceeds the 0.05 = α there is no significant difference measured between the DGP antibody concentrations in horses with ISBD and horses without ISDB, kept on a gluten-rich diet. There has also no significant difference been found between group 2 and 3, ρ-values= 0.1403 > 0.05. There is however a significant difference between group 1 and 3, since ρ = 0.0244 < 0.05. Therefore horses with ISBD have a significantly higher concentration of DGP antibodies than the gluten-free control group. Striking are the high concentrations of the two horses (No. 22 and 24) in group 2 and the one (No. 59) in group 3. Patient no. 7 also shows to be strongly positive. 23 | P a g e 24 THE POTENTIAL ROLE OF GLUTEN IN EQUINE INFLAMMATORY SMALL BOWEL DISEASE Using a Log transformation, seen in Fig. 12, the differences between the groups become clearer. Fig. 12: Multiple comparison (dot and box plot) graph showing the GA in AU/ml per group, in Log transformation. DGP antibodies in arbitrary units (AU) per milliliter per group (in Log transformation). 100 10 1 Horizontal reference line value = 1,0 AU/ml 0.1 1 2 3 group (group 1= patients, group 2= gluten-rich controls, group 3= gluten-free controls) IFT: Anti-endomysium antibodies This test was performed to see if there were any IgA antibodies against endomysium. There were no anti-endomysium antibodies (EmA) found in patients No. 1,2,7 and 8, when using monkey oesophageal tissue as a substrate. Also controls 21-24 were found to be negative. Because of the lack of staining the remaining patients and controls were not tested for EmA in monkey oesophagus. It is surprising that patient No. 7 does not show any staining since it does have high rh-TGA. For some horses, however, the smooth muscle cells stained positive, including No. 7. 24 | P a g e 25 THE POTENTIAL ROLE OF GLUTEN IN EQUINE INFLAMMATORY SMALL BOWEL DISEASE 3.2 Comparative histology A human pathologist performed re-examination of histopathological biopsies, from some of the equine ISBD patients. The sections were stained with HE and examined under a light microscope. The histological findings are summarised in table 6. Table 6: Findings upon histological examination of equines suspected from ISBD. P. No 2 3 5 7 IEL count* <30/100 At most a <30/100 <30/100 minor increase. Crypt hyperplasia Villous Somewhat Mild atrophy short. Lamina Lamina PreLamina Lamina propria propria looks infiltrative propria looks propria looks somewhat (normal). somewhat somewhat fibrous, fibrous. fibrous, pour amount pour amount of cells. of cells. 8 <30/100 9 <30/100 - - Mild? - Lamina propria looks somewhat fibrous. Lamina propria looks somewhat fibrous, only in the villi. Deeper mucosa is infiltrated normally. IEL’s = intraepithelial lymphocytes The histological findings, in biopsies taken from the proximal duodenum, show no major abnormalities in the horses with ISBD. None of the horses show a clear IEL increase and only some show some villous blunting. Most remarkable is the reduced amount of cells in the lamina propria in almost all patients, compared to that of the human duodenum. 25 | P a g e 26 THE POTENTIAL ROLE OF GLUTEN IN EQUINE INFLAMMATORY SMALL BOWEL DISEASE 3.5 Clinical trial/case study: measuring the effects of a gluten-free diet The owner of patient no. 7, a horse known to suffer from ISBD and with an exceptional high tTGA concentration, was asked to adjust their horse’s diet to a gluten-free one (Annex 4). Patient no. 7 was diagnosed with ISBD, based on abnormal findings during rectal examination, a lowered glucose tolerance test and histopathological examination of a (proximal duodenal) biopsy by a pathologist. After a dieting period of 6-7 months another plasma sample was collected, from peripheral venous blood using lithium-heparin tubes. This sample was, again, subject of all ELISA tests. Results are illustrated in fig. 13 and summarized in table 7. Fig. 13: The effect of a gluten-free diet on the IgA antibodies against E. coli, rh-tTG, gp-tTG, gliadin and deamidated gliadin. In particular the decrease in rh-tTGA from 100 AU/ml to 32,5 AU/ml, after adjustment to a gluten-free diet, is remarkable. The other parameters show a lesser amount of decrease. As suspected the IgA antibody concentration against E. coli exposes no changes. Table 7. IgA antibodies against E. coli, recombinant human tissue-transglutaminase, guinea pig tissuetransglutaminse, gliadin and deamidated gliadin.before and after a gluten-free diet (GFD) [E.coli antibody] in AU/ml [rh-TGA]in AU/ml [gp-TGA]in AU/ml [Gliadin antibody] in AU/ml [DGP antibody] in AU/ml Patient No. 7 100, +++ 100 100 61,2 25 Patient No. 7 GFD 100, +++ 32,5 95,1 53,1 18.75 26 | P a g e 27 THE POTENTIAL ROLE OF GLUTEN IN EQUINE INFLAMMATORY SMALL BOWEL DISEASE Other blood parameters measured in patient No. 7 show the following changes: Table 8. Blood parameters before and after a gluten-free diet (GFD) ID No Breed Sex Age (yea Clinical presentation rs) 7 KWPN 7* KWPN stallion stallion 14 15 Weight loss, reduced performance - Ht Lymphoc ytes Albumin ( x*10^9/L) Total protein ( g/L) (L/L) (g/L) Percutaneous ultrasound / rectal exam (+) Glucose tolerance test 0,41 2,4 66 35 + 40% 0,40 - 69 37 ND ND Sampling date 080610 060111 Due to the athletic obligations of the horse a second glucose tolerance test and biopsy have not yet been performed. 27 | P a g e 28 THE POTENTIAL ROLE OF GLUTEN IN EQUINE INFLAMMATORY SMALL BOWEL DISEASE PART 4: DISCUSSION To answer the question if gluten play a role in the aetiology of equine ISBD we’ve subjected three groups of horses to six different human coeliac disease diagnostic tests; to compare the results of the ISBD patients, two different control groups without ISBD have been tested: one group being on a gluten-rich diet, the other on a gluten-free diet. 3.1 animals and sampling Animal selection Inflammatory (small) bowel disease represents a poorly characterized group of conditions in the horse that may present with a dull hair coat, weight loss, colic and at times soft faeces, oedema and lethargy.22 The ISBD patients used in this study were diagnosed based on their history, clinical examination and blood work. During rectal examination thickening of the small intestine was palpated in 9 out of 12 cases and was noted on abdominal ultrasonography in 2 patients. Combining the results of anthelmintic history and faecal flotation, involvement of parasites was excluded. A glucose tolerance test was performed in 7 patients and was found to be below standard in 5/7 patients. The results of the glucose tolerance test do not seem to correlate with serum albumin or the degree of intestinal inflammation in these patients. In only 6 cases a gastroduodenoscopyassisted biopsy of the duodenum was taken. According to a veterinary pathologist all of these biopsies showed mild enteritis, mostly with infiltration of IEL’s and plasma cells. The clinical relevance of these findings was taken into question, because none of the biopsies showed signs of severe enteritis. To make a definitive diagnosis of inflammatory small bowel disease and confirm the subtype, histopathological examination of affected intestine is necessary. Preferably using full thickness surgical biopsies. These were however taken in none of the patients, since they were mainly high performing dressage horses. So diagnoses are more tentative then confirmed. Also, the age range (8 till 18) and breeds of the included patients are not consistent with what today’s literature is stating. Most of the horses included in the study are Dutch warmblood horses, being the main horse breed in the Netherlands, but shouldn’t we look at the 2-4 year old Thoroughbred horses and Standardbreds, as literature reports these horses as being most susceptible to inflammatory small bowel disease subtypes eosinophilic and granulomatous enteritis? Only the lymphocyticplasmacytic subtype of ISBD shows no clear age relation.7 The suspected gluten-free population used in this study is housed year round in a nature reserve park in the Netherlands. They are part of a group consisting of about a hundred Shetland ponies, ranging in age from 1 till 27 years, all being mares. Their job is to preserve and develop the dune area with its associated succession stages: open, local dusty dune, pioneer vegetation, dune grasses and dune valleys, by grazing. As known, the grains such as barley, wheat and ray, which contain gluten, are part of the grass family. They are however production cereals and it is thought that most wild grass species don’t contain gluten or contain gluten in far less extent than found in concentrated feeds. Since the nature reserve park is open to public we cannot, unfortunately, rule out that horses are fed bread or any other kind of gluten containing feeds. 3.2 Development of a standardized ELISA test The goat anti horse IgA: horseradish peroxidase testing illustrated that the goat anti horse IgA:HRP works. All tests were performed using a 1:5000 conjugate dilution, and using OPD as a substrate for HRP. ELISA: Antibodies against E. coli In this study, all horses showed detectable IgA antibodies against E. coli, using a 1:20 serum dilution. The test was performed to rule out any IgA deficiency, which in humans has a known prevalence of 28 | P a g e 29 THE POTENTIAL ROLE OF GLUTEN IN EQUINE INFLAMMATORY SMALL BOWEL DISEASE about 1:400 and is even more common in patients with coeliac disease.17, 20 In horses, unlike selective immunoglobulin M deficiency, no selective immunoglobulin A deficiency has ever been described.16 Since all horses tested positive this remains this way. So, IgA could be used for further ELISA testing. The IgA antibody concentrations against E. coli are however significantly higher in horses with ISBD and in the gluten-rich controls than in the gluten-free, wild controls. Some of them showing remarkable low antibody titers. For the IgA testing the E. coli strain EB1 was used. EB1 is known to be a human pathogenic strain of E. coli. It could be hypothesized that since the gluten-free horses have lesser human contact they are also exposed less to this strain of E. coli resulting in a lesser serum IgA antibody concentration. ELISA: Antibodies against recombinant human tissue-transglutaminase (rh-tTG) The rh-tTGA concentrations were found to be significantly higher in horses with ISBD and in the gluten-rich control group then in the gluten-free control group. There was no significant difference found between the patients and the gluten-rich controls. As mentioned before, tTG in man is the enzyme that, by deamidation, makes gliadin peptides negatively charged and raises the immunostimulatory effect of gluten. Expression and activity of tTG are raised in the mucosa of patients with CD. And tTG is thought to be the main target autoantigen. 4 The results in this study suggest a relation between gluten-uptake and the rh-tTGA concentration in horses but show no clear relation between clinical signs of ISBD and rh-tTGA concentration. A. Tursi et al. (2003) showed that, in humans, anti-tTG prevalence and their mean serum value was higher in coeliacs with severe enteropathy (Marsh IIIb-c lesions) than in those showing slight enteropathy (Marsh I-IIIa). So, serologic tests without histological evaluation may underestimate the real prevalence of CD. 21 The correlation between degree of intestinal damage and positivity to rh-tTGA in horses remains undetermined. Given that tTG antibodies are antibodies that are directed against the complex of gliadin attached to tissue transglutaminase all wild controls were expected to be negative for TGA. As shown above some wild, gluten-free controls do possess some levels of rh-tTGA. This suggests a gluten uptake. Since the ‘gluten-free’ controls are housed in an ‘open to public’ nature reserve park it is thought they are in all probability fed bread. ELISA: Antibodies against guinea pig tissue-transglutaminase (gp-tTG) No significant relations between group gp-tTGA differences were found during this study. So there is no clear relation between a gluten containing diet, either with or without clinical signs of ISBD, and gp-tTGA in horses. Strangely the correlation coefficient r for both TGA tests (rh-tTGA and gp-tTGA) is 0,7005 (p<0,0001), suggesting a linear dependence between both variables. (Annex 3) Patient no. 7, which shows to be strongly positive in both tests, might illustrate this relation. ELISA: Antibodies against gliadin No significant relations between group GA differences were found during this study. Thus there is no clear relation between a gluten containing diet, either with or without clinical signs of ISBD, and GA in horses. In human medicine antigliadin antibodies are no longer considered sensitive enough or specific enough to be used for the detection of coeliac disease. Mainly the sensitivity for the IgA based test is thought to be poorly and highly variable. Resulting in a higher number of false negatives. Because of the variable and generally lower sensitivity and specificity associated with the GA, it is stated that these tests are less suitable for screening purposes.20, 24 ELISA: Antibodies against deamidated gliadin Unlike the GA concentrations, the DGP antibody concentrations were found to be significantly higher in horses with ISBD then in the gluten-free control group. Also, when combining the two gluten-rich groups (both clinically healthy and ISBD horses) a significant difference compared to the gluten-free group was found. So there seems to be a relation between gluten intake and the DGP antibody concentration in horses. DGP antibody testing is a relatively new ELISA used in human coeliac disease 29 | P a g e 30 THE POTENTIAL ROLE OF GLUTEN IN EQUINE INFLAMMATORY SMALL BOWEL DISEASE diagnostics, and although tTG display a higher predictive value then DGP and is still considered the best CD serological test, DGP antibody testing comes relatively close, showing high sensitivity and specificity. Volta et al. showed that sensitivities for DGP and tTG antibodies were 87.8% (95% CI: 85.6-89.9) and 93% (95% CI: 91.2-94.5), respectively, and the specificities were 94.1% (95%CI: 92.595.5) and 96.5% (95% CI: 95.2-97.5), respectively. 25 IFT: Anti-endomysium antibodies In human coeliac disease diagnostics the endomysium IgA antibody IFT is thought to be a highly specific marker, approaching 100% accuracy. Since it is recognized that tTG is the auto-antigen for the development of endomysium antibodies it raises the question why staining did not occur in any of the tested horses, that in some case did show a high rh-tTGA concentration.20 It could be that equine antibodies don’t recognize the monkey tissue transglutaminase. To rule this out another IFT needs to be performed, presumably on equine tissue. 3.2 Comparative histology Definitive diagnosis of the inflammatory small bowel disease subtype necessitates histopathological examination of the affected intestine. The histological findings in the horses with ISBD show no major abnormalities. According to a human pathologist, none of the horses show a clear IEL increase (or any other inflammatory cell infiltrate) and only some show some villous blunting. The latter may be due to the fact that the biopsies were probably taken from the duodenal bulb area, just after passing the pylorus, using a 2.2-meter endoscope. Collecting of intestinal biopsies from the duodenal mucosa is minimally invasive but, intuitively, the diagnostic usefulness of full thickness surgical biopsies is likely to be greater. Gastroduodenoscopy-assisted biopsy of the (proximal) duodenum could miss focal small intestinal infiltrative diseases, such as focal eosinophilic enteritis although lymphocyticplasmacytic enteritis has a more diffuse aspect such that abnormalities would be expected on the duodenal biopsy specimen. Performing a laparotomy to obtain the intestinal biopsy can be expensive, may occasionally result in peritonitis or incision infection and may delay introduction of immunosuppressive therapy until the incision sites are healed in otherwise well performing horses. 3,22,23 Reports by Packer et al. (2005) and Rotting et al. describe correspondingly the amount of immune cells in the jejunal mucosa and the mucosal distribution of eosinophilic granulocytes in the gastrointestinal tract in horses that were euthanized for reasons other that gastro-intestinal disease. Distribution of immune cells in the villous lamina propria and intercryptal lamina propria is reported, in mean ± SD cells/9000μm2, for plasma cells (18 ± 10.8, 35 ± 10.2), CD3+ T cells (50 ± 15.2, 50 ± 11.0), CD79a+ B cells (3 ± 3.4, 12 ± 7.6), neutrophils (0 ± 0.3, 0 ± 0.0) and macrophages (5 ± 2.8, 5 ± 3.5). Eosinophils are reported in highest numbers in the cecum (488 ± 285 cells/mm2) and the ascending and transverse colon, and the lowest are in the stomach (18 ± 22.4 cells/mm2), the duodenum (100 ± 93 cells/mm2) and the descending colon (83 ± 99 cells/mm2). Plasma cells and B cells have a higher density in the intercryptal than in the villous regions of lamina propria. The distribution of eosinophils within the mucosal lamina propria also follows a consistent pattern. In all sections of the gastrointestinal tract most eosinophils are located in the basilar half of the mucosa.11, 12 Normal distribution of immune cells, other than eosinophils, in the lamina propria of the horses duodenum remains however unclear. 3.3 Clinical trial/case study: measuring the effects of a gluten-free diet Since only one patient has been followed shifting from a concentrated, gluten-containing diet to a gluten-free diet, no statistical significant data are available. Nevertheless, all measured parameters show a positive decrease, predominantly the serological parameter: rh-tTGA, expect for the IgA antibodies agains E. coli, which as suspected remained strongly positive. Taking the assumption that gluten plays a role in the etiology of ISBD, it would seem plausible that plasma rh-tTGA could be used as a serological marker for gluten intolerance. A challenge study to measure possible relapse 30 | P a g e 31 THE POTENTIAL ROLE OF GLUTEN IN EQUINE INFLAMMATORY SMALL BOWEL DISEASE after a subsequent gluten intake would be a rational next step. From an ethical and welfare perspective, this is however unlikely to happen. PART 5: CONCLUSION This is the first study to investigate the potential role of gluten in the aetiology of equine inflammatory small bowel disease. Although some facts in the patient group and gluten-free control group are questionable and so as researchers we have to be a little sceptic, it is a start in enfolding the effects of gluten on the equine intestine and its immune system. IgA deficiency was excluded in all participating horses. The results in this study suggest a relation between gluten-uptake and the rh-tTGA concentration in horses but show no clear relation between clinical signs of ISBD and rh-tTGA concentration. Also, there seems to be a relation between gluten intake and the DGP antibody concentration. The DGP antibody concentrations were found to be significantly higher in horses with ISBD then in the gluten-free control group. And, in addition, when combining the two gluten-rich groups, a significant difference compared to the gluten-free group was found. In human medicine both the rh-tTGA and the DGP antibody ELISA are thought to be highly sensitive and specific for diagnosing coeliac disease. On the other hand no clear relation was found between the use of gluten, signs of ISBD and the amount of gp-tTGA and GA. Furthermore, the endomysium IgA antibody IFT on monkey oesophagus was inconclusive, showing no specific staining. Thus, on the basis of this data it is not possible to draw any clear conclusions about the role of gluten in equine inflammatory small bowel disease yet. But, the notion that rh-tTGA and DGP antibody concentrations are raised in horses fed a gluten rich diet suggest an immunostimulatory effect of gluten, that could play a role in the aetiology of ISBD. One case, showing both clinically as well as serological improvement after a gluten-free diet supports this possibility. However, further research is needed to clarify the specifics. 31 | P a g e 32 THE POTENTIAL ROLE OF GLUTEN IN EQUINE INFLAMMATORY SMALL BOWEL DISEASE ACKNOWLEDGEMENTS As mentioned before, this study was performed in joint venture with the VUmc Research Institute for Cancer and Immunology and the Department of Gastroenterology and Hepatology at the VUmc in Amsterdam. I would like to thank both departments and within these especially dr. B.M.E. von Blomberg, Rubi, Martine, Jolien, dr. N.C.T. van Grieken and prof. dr. C.J.J. Mulder for their ideas, patience, persistence, support and the many practical work hours they put into this research. This research project was carried out within the study of Veterinary Medicine at the Utrecht University and was initiated and supervised by dr. J.H. van der Kolk and supported by dr. G.C.M. Grinwis. The study could not have been performed without the consent of the horses’ owners and the cooperation of the veterinary clinics Oisterwijk and Hattem-Wapenveld and the environmental public organization Staatsbosbeheer. 32 | P a g e 33 THE POTENTIAL ROLE OF GLUTEN IN EQUINE INFLAMMATORY SMALL BOWEL DISEASE REFERENCES 1. Schumacher, J., Edwards, J. F., & Cohen, N. D. (2000). Chronic idiopathic inflammatory bowel diseases of the horse. J Vet Intern Med , 14 (3), 258-265. 2. Kemper, D. L., Perkins, G. A., Schumacher, J., Edwards, J. F., Valentine, B. A., Divers, T. J. , et al. (2000). Equine lymphocytic-plasmacytic enterocolitis: a retrospective study of 14 cases. Equine Vet J Suppl. , 32, 108-112. 3. Archer, D. C., Edwards, B. G., Kelly, D. F., French, N. P., & Proudman, C. J. (2006). Obstruction of equine small intestine associated with focal idiopathic eosinophilic enteritis: An emerging disease? The Veterinary Journal , 171, 504-512. 4. Di Sabatino, A., & Corazza, G. R. (2009). Coeliac disease. The Lancet , 373, 1480-1493. 5. Dansen, O., & Van Rutten, J. (2008). The secret of inflammatory small bowel disease. Utrecht University, Faculty of Veterinary Medicine, Department of Equine Sciences, Internal Medicine, Utrecht. 6. Roberts, M. C. (2003). Proliferative and inflammatory intestinal diseases associated with malabsorption and maldigestion. In S. M. Reed, W. M. Bayly, & D. C. Sellon, Equine Internal Medicine (2 ed.). St. Louis, Missouri, USA: Saunders Elsevier. 7. Kalck, K. A. (2009). Inflammatory bowel disease. Vet Clin North Am Equine Pract , 25, 303-315. 8. Barr, B. S. (2006). Infiltrative intestinal disease. Vet Clin North Am Equine Pract , 22, 1-7. 9. Ettinger, S. J., & Feldman, E. C. The gastrointestinal system. In S. J. Ettinger, & E. C. Feldman, Textbook of veterinary internal medicine (4 ed., Vol. 2). St. Louis, Missouri, USA: Saunders Elsevier. 10. Wieser, H. (2007). Chemistry of gluten proteins. Food microbiology , 24, 115-119. 11. Packer, M., Patterson-Kane, J. C., Smith, K. C., & Durham, A. E. (2005). Quantification of immune cell populations in the lamina propria of equinejejunal biopsy specimens. J Comp Pathol , 132 (1), 90-95. 12. Rottinger, A. K., Freeman, D. E., Constable, P. D., Eurell, J. A., & Wallig, M. A. (2008). Mucosal distribution of eosinophilic granulocytes within the gastrointestinal tract of horses. Am J Vet Res , 69 (7), 874-879. 13. Fogarty, U., Perl, D., Ensley, S., Seawright, A., & Noonan, J. (1998). A cluster of equine granulomatous enteritis cases: the link with aluminium. Vet Human Toxicol , 40 (5), 297-305. 14. Kagnoff, M. F. (2007). Celiac disease: pathogenesis of a model immunogenetic disease. J Clin Invest , 117 (1), 41–49. 15. Daminet, S. C. (1996). Gluten-sensitive enteropathy in a family of irish setters. Can Vet J , 37, 745-746. 16. Crisman, M. V., & Kent Scarratt, W. (2008). Immunodificiency disorders in horses. Vet Clin Equine , 24, 299-310. 17. Cunningham-Rundles, C., Brandeis, W. E., Pudifin, D. J., Day, N. K., & Good, R. A. (1981). Autoimmunity in selective IgA deficiency: relationship to anti-bovine protein antibodies, circulating immune complexes and clinical disease. Clin Exp Immunol , 45, 299-304. 18. Greco, L. (1997). From the neolithic revolution to gluten intolerance: benefits and problems associated with the cultivation of wheat. J Pediatr Gastroenterology Nutr , 24 (5), 14-17. 19. Dickson, B. C., Streutker, C. J., & Chetty, R. (2006). Coeliac disease: an update for pathologists. J Clin Pathol , 59 (10), 1008-1016. 20. Green, P. H., & Cellier, C. (2007). Celiac Disease. N Engl J Med , 357, 1731-43. 21. Tursi, A., Brandimarte, G., & Giorgetti, G. M. (2003). Prevalence of Antitissue Transglutaminase Antibodies in Different Degrees of Intestinal Damage in Celiac Disease. J Clin Gastroenterol , 36 (3), 219-221. 22. Durham, A. E., & Rendle, D. (2010). Inflammatory bowel disease as a cause of colic: diagnosis and treatment. 49th BEVA Congress (pp. 198-199). Newmarket: Equine Veterinary Journal Ltd. 33 | P a g e 34 THE POTENTIAL ROLE OF GLUTEN IN EQUINE INFLAMMATORY SMALL BOWEL DISEASE 23. Divers, T. J., Pelligrini-Masini, A., & McDonough, S. (2006). Diagnosis of inflammatory bowel disease in a Hackney pony by gastroduodenal endoscopy and biopsy and succesfull treatment with corticosteroids. Equine vet. Educ. , 18 (6), 284-287. 24. Hill, I. D. (2005). What Are the Sensitivity and Specificity of Serologic Tests for Celiac Disease? Do Sensitivity and Specificity Vary in Different Populations? Gastroenterology, 128, S25S32. 25. Volta, U., Fabbri, A., Parisi, C., Piscaglia, M., Caio, G., Tovoli, F., et al. (2010). Old and new serological tests for celiac disease screening. Expert Rev Gastroenterol Hepatol. , 4 (1), 31-35. 26. Brown, I., Mino-Kenudson, M., Deshpande, V., Lauwers, G.Y. (2006) Intraepithelial lymphocytosis in architecturally preserved proximal small intestinal mucosa: an increasing diagnostic problem with a wide differential diagnosis. Arch Pathol Lab Med, 130, 1020–1025 ABBREVIATIONS AGA AU BSA CD DGP E. coli EDTA ELISA FACS FITC GA GFD gp-tTG gp-tTGA GRD HLA HRP IEL’s IFT Ig IBD ISBD KWPN LE LPE MHC Nd OPD rh-tTG rh-tTGA TGA tTG anti-gliadin antibodies arbitrary unit bovine serum albumin coeliac disease deamidated gliadin Escherichia coli ethylenediaminetetraacetic acid enzyme linked immunosorbent assay fluorescence-activated cell sorting fluorescein isothiocyanate isomer 1 gliadin antibodies gluten-free diet guinea pig tissue transglutaminase tissue transglutaminase antibodies (guinea pig) gluten-rich diet human leukocyte antigen horseradish peroxidase intraepithelial lymphocytes immunofluorescence test immunoglobulin inflammatory bowel disease inflammatory small bowel disease Dutch Warmblood horse lymphocytic enteritis lymphocytic-plasmacytic enteritis major histocompatibility complex not determined o-phenylenediamine dihydrochloride recombinant human tissue transglutaminase tissue transglutaminase antibodies (recombinant human) tissue transglutaminase antibodies tissue transglutaminase 34 | P a g e 35 THE POTENTIAL ROLE OF GLUTEN IN EQUINE INFLAMMATORY SMALL BOWEL DISEASE ANNEX 1 Overview of the research group, including patients (ISBD), controls (gluten-rich, not known to have ISBD) and wild (gluten-free) horses. group ID No breed age sex sampling patient 1 KWPN 18 gelding 160210 patient 2 KWPN 5 gelding 040210 patient 3 KWPN 7 mare 020210 patient 4 Frisian 11 mare 160210 patient 5 KWPN 8 gelding 040210 patient 6 KWPN 9 mare 180610 patient 7 KWPN 14 stallion 080610 patient 8 KWPN 11 gelding 060610 patient 9 KWPN 14 mare 150410 patient 10 KWPN 14 gelding 200810 patient 11 KWPN 9 gelding 101210 patient 12 KWPN 10 mare 060111 Patient* GFD 7* KWPN* 15 Stallion 060111 *All patients were referred to the Department of Equine Sciences, Section of Internal Medicine, Utrecht University in the years 2010 and 2011. *GFD= gluten-free diet group ID No breed age sex sampling control 21 KWPN 11 mare 050310 control 22 KWPN 15 mare 050310 control 23 KWPN 7 mare 050310 control 24 KWPN 14 mare 050310 control 25 KWPN 12 mare 050310 control 26 KWPN 6 mare 050310 control 27 KWPN 8 mare 050310 control 28 KWPN 8 mare 050310 control 29 KWPN 11 mare 050310 control 30 KWPN 8 mare 050310 control 31 KWPN 18 mare 050111 control 32 KWPN 16 mare 050111 control 33 KWPN 12 mare 050111 control 34 KWPN 6 mare 050111 control 35 KWPN 4 mare 050111 control 36 KWPN 18 mare 050111 control 37 KWPN * mare 050111 control 38 KWPN 4 mare 050111 control 39 standardbred * gelding 050111 control 40 KWPN 11 mare 050111 control 41 shetland pony 12 gelding 050111 control 42 shetland pony 17 gelding 050111 * All gluten-rich controls are housed at the Department of Equine Sciences, Utrecht University for educational and research purposes. group control ID No 43 breed KWPN age 2 sex stallion sampling 200410 35 | P a g e 36 THE POTENTIAL ROLE OF GLUTEN IN EQUINE INFLAMMATORY SMALL BOWEL DISEASE group ID No breed age sex sampling wild 51 shetland pony * mare 061010 wild 52 shetland pony * mare 061010 wild 53 shetland pony * mare 061010 wild 54 shetland pony * mare 061010 wild 55 shetland pony * mare 061010 wild 56 shetland pony * mare 061010 wild 57 shetland pony * mare 061010 wild 58 shetland pony * mare 061010 wild 59 shetland pony * mare 061010 wild 60 shetland pony * mare 061010 wild 61 shetland pony * mare 061010 wild 62 shetland pony * mare 061010 wild 63 shetland pony * mare 061010 wild 64 shetland pony * mare 061010 wild 65 shetland pony * mare 061010 wild 66 shetland pony * mare 261010 wild 67 shetland pony * mare 261010 wild 68 shetland pony * mare 261010 wild 69 shetland pony * mare 261010 wild 70 shetland pony * mare 261010 wild 71 shetland pony * mare 261010 wild 72 shetland pony * mare 261010 wild 73 shetland pony * mare 261010 wild 74 shetland pony * mare 261010 wild 75 shetland pony * mare 261010 * All “ wild” Shetland ponies are housed in a reserve in Zeeland (in the southwest of the Netherlands) and belong to Nature Reserves. Their diet consist of grasses and herbs and is considered to be gluten-free. Other materials used: A duodenal section in formalin, from control No. 43. Used for comparative histology. 2 x 1ml peripheral venous blood, collected in lithium-heparin tubes (sampling 27-10-’10), from controls No. 24 & 27. The blood was used for trial FACS analysis. 2x 50ml peripheral venous blood, collected in lithium-heparin tubes (sampling 20-01’11), from controls No. 24 & 27. The blood was used for HLA-DQ2/DQ8 typing. 2x 50ml peripheral venous blood, collected in lithium-heparin tubes (sampling 20-01’11), from patients No. 7* & 11 The blood was used for HLA-DQ2/DQ8 typing. 36 | P a g e 37 THE POTENTIAL ROLE OF GLUTEN IN EQUINE INFLAMMATORY SMALL BOWEL DISEASE ANNEX 2 Results ELISA’s in AU/ml. Group 1 1 1 1 1 1 1 1 1 1 1 1 4 Group 2 2 2 2 2 2 2 2 2 2 2 2 2 2 2 2 2 2 2 2 2 2 Group 3 3 3 3 3 3 3 3 3 3 3 3 3 3 3 3 3 3 3 3 3 3 3 3 3 ID No. 1 2 3 4 5 6 7 8 9 10 11 12 7*GFD rhTGA (AU/ml) 33.9 10.1 5.4 6.8 5.3 8.6 100.0 27.7 14.0 31.6 6.8 16.3 32.5 GA (AU/ml) 34.0 19.8 15.3 26.8 10.5 8.8 61.2 28.0 15.3 46.3 20.7 44.7 53.1 e.coli (AU/ml)121.8 73.7 53.9 101.7 46.6 33.1 125.9 92.2 36.2 100 106.7 95.5 125.4 e.coli +/++/+++ +++ ++ + +++ + + +++ ++ + +++ +++ ++ +++ gpTGA(AU/ml) 42.1 12.5 14.1 21.0 12.3 20.1 100.0 62.8 11.0 30.8 23.4 23.8 95.1 DGP(AU/ml) 12.6 1.3 2.6 2.0 9.2 1.0 25.0 11.9 2.1 11.7 8.0 3.2 ND 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 9.2 21.8 11.4 20.1 6.3 28.0 15.3 21.5 14.0 35.5 5.4 18.9 7.6 3.9 0.03 9.6 7.3 6.9 4.7 6.2 4.9 0.03 30.2 51.8 9.3 53.3 17.5 22.0 17.2 100 22.9 17.9 14.8 135.5 34.3 9.2 13.6 55.8 14.0 29.3 14.1 15.1 22.3 7.4 54.1 92.5 85.4 106.5 96.6 111.2 39.8 41.8 118.4 50.0 72.85 138.9 88.6 41.8 25.0 105.7 65.7 97.6 39.05 90.8 42.1 64.9 + ++ ++ +++ ++ +++ + + +++ + ++ +++ ++ + + +++ ++ ++ + ++ + ++ 13.6 25.7 13.1 32.5 9.5 77.0 8.2 13.2 13.4 17.0 15.8 74.0 36.9 17.4 9.2 21.1 20.9 20.8 14.7 12.4 15.2 11.1 9.3 88.1 2.1 >100 1.0 1.3 0.8 1.5 1.6 1.4 2.6 10.6 17.1 ND ND 2.5 3.1 2.7 1.5 4.2 3.4 ND 51 52 53 54 55 56 57 58 59 60 61 62 63 64 65 66 67 68 69 70 71 72 73 74 75 11.5 3.9 0.03 8.4 5.4 0.03 0.03 0.03 3.2 0.03 0.03 0.03 0.03 0.03 0.03 17.2 4.5 4.3 0.03 7.3 10.2 5.3 5.1 6.2 3.7 24.5 24.1 28.8 89.1 21.5 9.9 9.7 24.6 10.1 17.8 10.1 56.4 11.0 28.1 10.2 63.0 29.4 20.4 28.0 26.5 20.0 26.3 24.5 39.3 15.3 109.4 106.9 96.1 117.2 94.8 13.3 9.0 10.6 21.4 9.7 24.1 12.1 14.0 14.4 5.4 90.2 27.0 22.4 9.5 31.4 59.2 34.8 19.2 35.3 26.4 +++ +++ ++ +++ ++ + + + + + + + + + + ++ + + + + + + + + + 22.3 20.2 9.0 21.9 22.5 21.5 33.5 8.6 15.8 8.2 ND 34.1 16.3 7.8 17.2 40.1 14.4 18.6 31.5 37.8 26.7 9.5 17.5 35.8 9.7 2.7 3.4 1.9 1.8 1.9 0.9 3.9 0.7 >100 1.4 0.6 2 0.8 3.3 0.8 10.8 1.5 1.9 1.2 ND ND ND ND ND ND 37 | P a g e 38 THE POTENTIAL ROLE OF GLUTEN IN EQUINE INFLAMMATORY SMALL BOWEL DISEASE ANNEX 3 Correlation statistics using Medcalc. Scatter diagram showing the correlation between the rh-tTGA and the E.coli antibody test. 100 80 60 [ E.coli 40 20 r= 0.4560 P= 0.0003 0 0 20 40 60 [rh-TGA] in AU/ml 80 100 Scatter diagram showing the correlation between the rh-tTGA and the gp-tTGA test. 100 80 60 40 20 r= 0.7005 P<0.0001 0 0 20 40 60 [rh-TGA] in AU/ml 80 100 38 | P a g e 39 THE POTENTIAL ROLE OF GLUTEN IN EQUINE INFLAMMATORY SMALL BOWEL DISEASE Scatter diagram showing the correlation between the rh-tTGA and the GA test. 140 r=0.3822 P=0.0026 120 [GA] in AU/ml 100 80 60 40 20 0 0 20 40 60 [rh-TGA] in AU/ml 80 100 Scatter diagram showing the correlation between the rh-tTGA and the DGP antibody test. 100 r=0.1970 P=0.1704 80 60 40 20 0 0 20 40 60 [rh-TGA] in AU/ml 80 100 39 | P a g e 40 THE POTENTIAL ROLE OF GLUTEN IN EQUINE INFLAMMATORY SMALL BOWEL DISEASE Scatter diagram showing the correlation between the GA and the DGP antibody test. 100 r=0.1450 P=0.3150 80 60 40 20 0 0 20 40 60 80 [GA] in AU/ml 100 120 140 ANNEX 4 The gluten-free diet of “case study” and patient No. 7. hour of the day 08.00 sort of feed Supplements GF- Concentrate Roughage 11.30 GF-Concentrate 14.00 16.30 GF-Concentrate 22.00 GF-Concentrate Roughage kilograms 30 grams 50 grams 340 grams 960 grams (480 in rest) 490 grams 3 kilograms 340 grams 960 grams 490 grams 1 kilogram 340 grams 960 grams (480 in rest) 490 grams 250 grams 3 kilograms Type of feed Equistro megabase Equitop myoplast Hartog Lucerne Black crushed oats Cavalor Strucomix Hartog compact grasses Hartog Lucerne Black crushed oats Cavalor Strucomix Carrots Hartog Lucerne Black crushed oats Cavalor Strucomix Cavalor Strucomix Hartog compact grasses 40 | P a g e