Asthma
advertisement

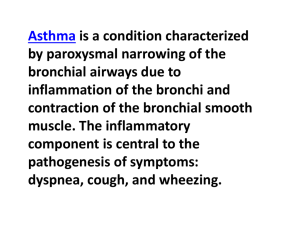
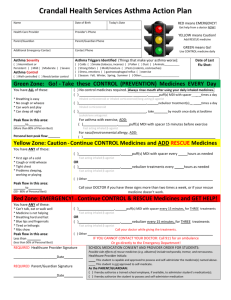
Asthma Definition of Asthma: 1. Chronic airway inflammatory disorder 2. Recurrent episodes of wheezing, chest tightness, shortness of breath, and coughing at night or in the early morning 3. Reversible airway limitation Diagnosis of Asthma[5] 1. History:: cough worse at night, recurrent wheezing/chest tightness recurrent difficult breathing 2. Symptoms occur or worsen at night, awakening the patient 3. Physical examination: wheezing, silent chest when severe asthma 4. Lung function test ( FEV1 and PEFR ) - PEFR increases > 15% after inhalation of short-acting β2 –agonists 15~20 mins - PEFR varies > 20% from morning to 12 hours later - PEFR decreases > 15% after 6 mins of exercise 5. Risk factors: - Allergic IgE-mediated diseases, allergic rhinitis, atopic dermatitis, and eczema - Familial members with asthma - exacerbation associated with weather change, foods, drugs… 1 Classification of Asthma Severity [5] Classification STEP 1: Intermittent STEP 2: Mild persistent Clinical Features Before Treatment Days Symptoms Night-time Lung Function Test Symptoms < 2 times/month -FEV1 or PEF > = 80% < 1 times/week predicted -PEF variability < 20% > 1 times /week, but < 1/day > 2 /month -FEV1 or PEF > = 80% predicted -PEF variability 20-30% STEP 3: Daily symptoms Moderate persistent > 1 /week -FEV1 or PEF in 60%~80% predicted -PEF variability > 30% STEP 4: Severe persistent Frequent -FEV1 or PEF < 60% predicted -PEF variability > 30% Continual symptoms Stepwise Approach for Managing Asthma in Adult [5] Quick Relief All Patients Classification STEP 1: Intermittent STEP 2: Mild persistent - Short-acting bronchodilator with inhaled β2 -agonists as needed for symptoms. - Intensity of treatment will depend on severity of exacerbation. - Use of bronchodilator > 1/week over a 3 months period in intermittent asthma may indicate the need to “step-up” therapy Daily Control Medicines Other Treatment Options - No daily medication - Anti-inflammatory: inhaled corticosteroid (low doses) - Sustained-release theophylline to serum concentration of 5-15 μg/mL 2 STEP 3: Moderate persistent - Low~mideum-dose of inhaled corticosteroid + long-acting inhaled β2 –agonist - Cromone or - Leukotriene modifier - Medium-dose of inhaled corticosteroid + sustained-release theophylline, or - Medium-dose of inhaled corticosteroid + long-acting oral β2 –agonist, or - High-dose inhaled corticosteroid, or - Medium-dose of inhaled corticosteroid + leukotriene modifier STEP 4: - Inhaled corticosteroid (high Severe persistent dose) + long-acting inhaled β2 –agonist + if needed: • sustained-release theophylline • leukotriene modifier • long-acting inhaled β2 –agonist • oral glucocorticosteroid * Step down: Review treatment every 1 to 6 months. If control is sustained for at least 3 months, a gradual stepwise reduction in treatment may be possible. * Step up: If control is not achieved, consider step up. Inadequate control is indicated by increased use of short-acting β2-agonists and in: - step 1 when patient uses a short-acting β2-agonist more than two times a week; - steps 2 and 3 when patient uses short-acting β2-agonist on a daily basis OR more than three to four times a day. - But before stepping up: review patient inhaler technique, compliance, and environmental control (avoidance of allergens or other precipitant factors). Criteria for Hospitalization [1-2] 1.Any symptoms of asthma with a FEV1 or peak-expiratory flow rate (PEFR) < 50% of predicted value 3 2.PaCO2 ↑ 3.Prolonged attack of asthma of > 24 hours duration 4.Age > 40 years 5.Poor response after 4 hours of bronchodilator therapy 6.Recent or multiple emergency department or hospitalizations for treatment of asthma that occurred within the last year 7.History of ET intubation for asthma 8.Poor access to medical follow-up 9.Psychiatric conditions that are interfering with medical compliance The initially quick assessment of ASTHMA in admission [2,5] Examination finding Mild Level of Severity Moderate Severe Conscious State Normal Normal Altered Speaking Ability Sentences Phrases Words Respiratory rate (b/min) ABGs: PaO2 PaCO2 SaO2 <20 20 – 30 >30 Normal < 45 mmHg > 95% > 60 mmHg < 45 mmHg 91 – 95% < 60 mmHg, cyanosis > 45 mmHg <90% Good Moderate Poor may have silent chest Air Entry Recommendations regarding initial treatment of an acute episode [2] 1. Oxygen therapy at a minimum of 6 L/min via face mask to achieve SaO2 > 95%. (Grade B) 2. Administration of high-dose inhaled bronchodilator (salbutamol 5mg via nebuliser, q15 minutes up to a maximum of 20mg). (Grade A) 3. Corticosteroids should be given within 1 hour of presentation. (Grade A) 4. Antibiotics are not required unless there is radiological evidence of pneumonia or proven or suspected bacterial bronchitis. (Grade B) 4 Quick Reference Guide - In Hospital Management of Asthma [2] Initial Assessment -Clinical Signs: Pulse Rate, Respiratory Rate, PEF, SaO2, level of fatigue -Action: taking further ABGs, other blood tests and Chest X-ray. Ward Treatment 1. Start short-acting bronchodilator with: • Inhaled β2 –agonists ( nebulization preferred ): 1 dose q20 mins X 1 hour • Salbutamol: MDI (+ spacer if needed) Usually 2 - 4 puffs prn but dosage is patient response dependent. 2. Oxygen therapy continued until SaO2 > 92% 3. Systemic Corticosteroids: prednisolone of 40-50 mg daily or parenteral hydrocortisone 100mg Q6H 4. Sedation is contraindicated in the treatment of exacerbation 5. Repeat assessment of good, incomplete, or poor response after pharmaco-therapy. 6. Commence discharge planning on admission Discharge Planning 1. Patient Education • Cause of exacerbation ( trigger factors) • Review inhaler device technique (台北總院 2F 氣喘衛教室) • Write a self-management plan 1. Activities of Daily Living and Social Support Assessed 3. Medications at Discharge • Keep therapy with inhaled β2 –agonists • Tapering of oral corticosteroid therapy • Review home medication and adjust as required 4. Discharge Details Faxed Include: • Discharge summary • Best and worst PEF • Asthma Management Plan • Clear arrangements for clinical review within 7 days. Poor Response • Exhaustion, drowsiness • Rising arterial PaCO2>45 • Unable to maintain adequate PaO2 > 60 Transfer to ICU for further managements Discharge when status: No nocturnal symptoms • PEF > 70% pred. or patient’s usual best • SaO2 > 90% • Able to complete activities of daily living • Clinical 5 References: 1. Status asthmaticus and hospital management of asthma, Spagnolo SV Immunol Allergy Clin North Am - Aug; 21(3); 503-533, 2001 2. Guidelines for the Hospital Management of Acute Asthma, Evidence Based Guidelines in Royal Melbourne Hospital, Review date: October 2000 3. Acute Asthma in Adults-A Review, CHEST 125:1081–1102, 2004 4. BTS/SIGN. British guideline on the management of asthma. Thorax; 58 (Supple I ):i1–94. 2003 5. Global Initiative for Asthma: Guideline for Asthma Management and Prevention - updated November, 2003. 6