UCLA Neurobiologists Identify Brain Cells That Control Breathing
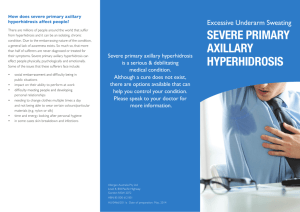
advertisement

UCLA Neurobiologists Identify Brain Cells That Control Breathing For the first time, UCLA scientists have identified the small group of brain cells believed to originate breathing in mammals. Reported in the September issue of Nature Neuroscience, their discovery could lead researchers to new approaches to addressing serious health problems, such as sleep apnea and sudden infant death syndrome. In a previous study, the UCLA team had pinpointed a specific region of brain tissue called the preBotzinger Complex as the command post for controlling breathing in mammals. Now, within the region, they distinguished a small group of neurons responsible for issuing the commands that generate breathing. "We hypothesized that if these neurons were important, something unusual would happen to breathing if we destroyed them," said Dr. Jack Feldman, Edith Agnes Plum Professor, UCLA neurobiology chair and principal investigator. "As it turned out, we were right." Using a rat model, the UCLA team zeroed in on the roughly 600 neurons less than one millionth of one percent of the total neurons in an adult rat's brain. The researchers stained a unique marker on the cells' surfaces to identify and count them. Then they administered a toxin that targeted the marker to kill just these cells. The results proved striking in animals that lost more than 80 percent of their neurons. "These rats' breathing dissolved from a regular, rhythmic pattern into a highly irregular pattern of breathing frequency and depth," said Dr. Paul Gray, UCLA neurobiologist and first author. "Equally important, the rats' brains stopped controlling the amounts of oxygen and carbon dioxide in the bloodstream the whole point of breathing," he said. While the findings prove the necessary role of these neurons in normal breathing, UCLA researchers are equally excited by the study's implications for the future. "Our findings suggest that these neurons may hold the underlying causes of breathing disorders and offer an excellent target for drugs treating these disorders," Feldman said. Because mammals' brains are organized in similar ways, Feldman believes that the same portion of the human brain will likely control breathing as that of rats. The UCLA team's next step will be to locate the same set of neurons in a human brainstem and then compare their physiology and function with the neurons of people with breathing disorders. If his hypothesis proves correct, Feldman may find fewer or dysfunctional neurons in the brains of people with breathing disorders. Human Kidney Protein Found That Regulates Heart Contraction And Blood Pressure New Haven, Conn. — Researchers at Yale School of Medicine and the VA Connecticut Healthcare System in West Haven identified a novel human kidney protein called renalase that regulates both heart contraction and blood pressure; it is a strong candidate for easily administered treatment of advanced kidney and cardiovascular disease. Over eight million people in the U.S. have kidney impairment and 500,000 have end-stage kidney disease (ESRD), for which treatment is often limited to dialysis. Elevated blood pressure and cardiovascular disease are commonly associated problems. Renalase is secreted by the kidneys and circulates freely in the bloodstream. Patients with kidney disease have very low levels of renalase, suggesting that its absence may lead to the cardiovascular complications found in ESRD. “This is one of the most exciting findings of kidney metabolism in recent years,” said Jianchao Xu, M.D., associate research scientist, attending physician and lead author. “It has immediate implications for therapy.” Like erythropoietin the human renalase protein could be injected to replace what is lost in kidney disease. While the kidneys remove waste and extra water from the body and control the balance of certain chemicals in the blood like sodium, phosphorus and potassium, by regulating the body water volume, they also have another function. They secrete hormones, like rennin and erythropoietin, into the blood to regulate blood pressure and red cell production. Neurosurgical Technique Relieves Excessive Sweating CHICAGO --- Forget that adage about how men sweat but women perspire. We all sweat, and it's a good thing we do. Sweating controls body temperature. As our temperature rises, the sympathetic nervous system stimulates certain glands in the body, the exocrine sweat glands, to secrete water to the skin surface, where it cools the body by evaporation. There are about five million exocrine glands in the human body -- 2 million in the hands alone, where they also assist grip. Emotional stress also stimulates sweating, particularly on the palms and forehead and in the armpits. But some people -- about 1 percent of the population -- sweat copiously following mild stimulation or none at all. They suffer from a disorder called hyperhidrosis, or excessive sweating. Hyperhidrosis can be an embarrassing and often occupationally debilitating condition that seems to be more common in people of Asian descent and in some cases may be hereditary. Its cause is unknown. Northwestern neurosurgeon Jeffrey S. Schweitzer, M.D., has treated patients with hyperhidrosis so severe that their palms literally dripped sweat. "For these patients, it can be impossible to hold a pen, to pick up a sheet of paper without soaking it or to touch other people," Schweitzer said. "Imagine how upsetting it is to shake hands with someone and see that person wipe his hands after touching yours. This is a daily event for patients with hyperhidrosis." Schweitzer, assistant professor of surgery at Northwestern University Medical School and a neurosurgeon at Northwestern Memorial Hospital, treats hyperhidrosis by performing endoscopic surgery to remove the nerves that stimulate the sweat glands in the palms. The procedure is done through an endoscope inserted through a small opening in the chest wall. The patient is usually kept overnight in the hospital. "The risks associated with this surgery are low, and the effect on the patient's self-image and ability to interact socially can be very gratifying," Schweitzer said. The procedure is also highly effective, Schweitzer said, with well over 80 percent of patients showing significant improvement in sweating on the palms. Fatty Foods Fight Inflammation "Take two cheeseburgers and call me in the morning," may sound like far-fetched medical advice. After all, high fat foods can worsen blockages in blood vessels. But a new study in the October 17 issue of The Journal of Experimental Medicine shows that high fat foods can, at least in the gut, soothe inflammation. This action may stop immune cells from attacking food as a foreign invader. Eating -- particularly eating fat-rich foods -- causes cells in the small intestine to produce a hormone called cholecystokinin, or CCK.CCK stimulates digestion and gut peristalsis (the motion that propels food along the digestive tract), and also triggers satiation – the full feeling that prompts you to stop eating. The study by Luyer and colleagues shows that fat-induced CCK can also dampen inflammation in the gut, as rats fed a high-fat diet were protected against lethal bacteriainduced shock whereas those fed a low-fat diet were not. CCK sent signals to the brain through the vagus nerve, the nerve that provides the electrical regulation for many internal organs, including the gut and the heart. In response to CCK, vagus nerve endings in the gut released a neurotransmitter called acetylcholine. Acetylcholine then bound to proteins on immune cells and turned the cells off. The authors think this pathway might explain why the immune system doesn't react to food proteins and normal gut bacteria as if they were foreign invaders. They also suggest that triggering this fat-driven chain of events in patients might provide a way to reduce inflammatory complications after surgery.