Student Handout
advertisement

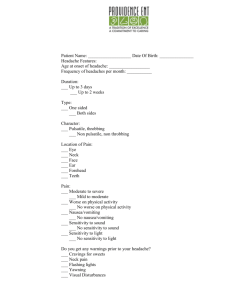
MODULE 2 Describing Pain Asking about Symptoms Picture compliments of Microsoft clipart Module Description and Content Goals: Given topics on pain history taking as well as signs and symptoms reporting; texts that are varied and of a specialized and medical nature, which include information presented from dialogues and other sources (e.g. photographs, drawings, reference text /research information), the participant will use English with 70 % accuracy to: 1. Use such words describing the concept of pain as: PAIN (noun), PAINFUL (adjective), ACHE (verb), ACHE (noun), HURT (verb), SORE (adjective) and SORE (noun). (Words and Expressions) 2. Identify and use adjectives describing the intensity, character and duration of pain. (Words and Expressions) 3. Listen for main ideas and details. (Listening) 4. Ask appropriate questions about signs and symptoms. (Listening, Speaking, Writing) 5. Identify three primary types of headaches and obtain information from tables. (Reading) 6. Form indirect questions. (Grammar and Speaking) 7. Conduct an interview between a patient and a doctor while taking a history of pain. (Speaking) 8. Record patients’ symptoms and write a history of pain (Writing) 9. Identify the Doorknob Syndrome and the techniques on how to get a patient to open up earlier in the exam. (Communication Tip, Reading). Module 2 STUDENT HANDOUT H2:1 A. WORDS & EXPRESSIONS TO KNOW. There are many words that Americans use to describe the concept of pain. Some of them are: PAIN (noun), PAINFUL (adjective), ACHE (noun), ACHE (verb), HURT (verb), SORE (noun), SORE (adjective) In addition to understanding the meaning of these words, it is necessary to know how to use them correctly in a phrase or sentence. Not all words go together. For example, do you we have an earache or ear pain, a chest ache or chest pain? Do we hurt all over or do we ache all over? Do people have a sore throat or a painful throat? Below are the common collocations that are used with each word. Study them and then do the exercise that follows. PAIN (noun) - the feeling you have when part of your body hurts to cause pain/ to give pain to be in pain/to have pain/to suffer from pain/ to feel pain The following expressions are antonyms (opposites): to increase pain/to make it worse pain intensifies/ increases/ grows stronger ≠ ≠ to alleviate/to ease/to kill/to relieve/to stop pain pain wears off / stops/ disappears PAINFUL (adjective) - that causes pain (can be both physical and emotional) The patient was complaining of painful, swollen knee joints. It is still painful for him to talk about the divorce. ACHE (noun) – pain that lasts for a long time; usually used in compound nouns I have a headache/ stomachache/ toothache/ earache/backache/heartache (often emotional; a strong feeling of sadness) He suffered from all kinds of pains and aches – many small pains which he felt at the same time, but no real health problems ACHE (verb) - to feel a continuous pain I ached all over. /My back ached badly. /My feet really ached. HURT (verb) - to feel pain/to cause pain in a part of your body She fell and hurt her leg slightly/quite badly. My ankle still hurts me slightly/quite badly. It hurts my knees to run. I have to sit down because my legs are hurting me. HURT can mean not only physical pain but also emotional His remarks hurt me deeply. /I didn’t mean to hurt you. SORE (noun) - a painful, often red place on your body caused by a wound or infection The patient developed a bedsore. / Cold sores are also called fever blisters. SORE (adjective) – painful as a result of a wound, infection or too much exercise I have a sore throat. / My foot is sore. B. PAIN, PAINFUL, ACHE, HURT or SORE? Fill in the blanks choosing the best word: 1. He is suffering from chronic _________________________ . 2. He completed the marathon and his body _________________________ all over. 3. I made an appointment with the dentist because I couldn’t put up with my ______________________ any longer. 4. A wasp sting can be very____________________________. 5. He was badly ___________________________ in the accident. 6. Gardening and biking aggravates my ____________________________. 7. That spot is very __________________________, doctor. Don’t press it. 8. After I took the analgesic, the _______________________ wore off. 9. I can’t walk. My ankle __________________________. 10. Old people usually suffer from a lot of __________________________ and _____________________________. 11. He is ________________________ because of all that exercise. 12. Despite all the chiropractic adjustments, my back still __________________________ me. C. acute nagging gnawing cutting cramping Your patients may use the following adjectives to describe their pain: burning shooting gripping piercing splitting sudden persistent receding searing recurring chronic stabbing slight radiating heavy blunt throbbing agonizing subtle pounding sharp constant intense sporadic debilitating deep colicky aching tender pulsating intermittent excruciating unbearable uncomfortable incapacitating manageable subsiding stinging dull jabbing It is important to understand these terms as they may indicate the type and the source of the pain. Use patient’s own words to record the subjective data; restating in other words what client says may change its original meaning. D. Classify the words in Part C according to pain intensity, duration and character. Record them in the correct column. Some adjectives belong to more than one column. Use your English-English dictionary if you need it. Follow the example. INTENSITY OF PAIN SEVERE acute sharp CHARACTER OF PAIN MILD nagging DURATION OF PAIN E. Rate the pain on a scale from 1 to 10. 1 signifies the least pain; 10 means the worst pain possible. The first one is done for you. Answers may slightly vary as this rating is highly subjective. debilitating gripping aching mild 1 mild 2 _______________________ 3 _______________________ 4 _______________________ 5 _______________________ 6 _______________________ 7 _______________________ 8 _______________________ 9 _______________________ 10 _______________________ agonizing manageable dull gnawing tender throbbing Module 2 STUDENT HANDOUT H2:2 LISTENING: A. Listening for Main Ideas. Pain is one of the most common symptoms patients complain about. The best judge of the severity and character of pain is the patient, so Dr. Howell is trying to get as much information from Ms. Sandler as possible. Listen to the second part of their interview. Then answer the following questions: 1. Ms. Sandler describes her pain as A. stabbing and excruciating B. severe and throbbing C. dull and nagging 2. Ms. Sandler’s headache usually lasts 2 days. True False 3. When Ms. Sandler has an episode of pain, it usually occurs A. on one side of the head B. on the left and on the right 4. It hurts the least A. in the morning B. in the evening C. at the front and at the back of the head C. when she goes to bed 5. Ms. Sandler has a well-balanced diet. True False 6. Which wasn’t one of the pain triggers Ms. Sandler mentioned: A. Chocolate B. Her son C. Skipping meals 7. Ms. Sandler is embarrassed to talk about her headaches. True False D. Depression E. Her business B. In order to be able to assess pain and help the patient, it is necessary to collect as much information about it as possible. Listen to this interview again. This time, pay close attention to the questions the physician uses to gather information about the pain. Write them down in the spaces provided. Dr. Howell: So, Ms. Sandler, we have several things going on here, but let’s talk about your headaches first. __________________________________________________________________________________________ Ms. Sandler: Usually it’s a severe, throbbing pain. Last week it was so bad that I had to take a couple days off, and I can’t do it right now, being the only owner of the restaurant. Dr. Howell: You said it’s severe and throbbing. _____________________________________________________________ ___________________________________________________________________________________________________ ___________________________________________________________________________________________________ Ms. Sandler: It can be anywhere from 4 to 10, although last week I experienced the worst pain ever. If I had to use the same scale, I would rate it 11! It was excruciating. Dr. Howell: ________________________________________________________________________________________ Ms. Sandler: Well, it seems to vary. It usually lasts a day and it wears off in the second half of the day. But last week I was down with it for 2 days. Dr. Howell: OK. _____________________________________________________________________________________ Ms. Sandler: Well, the pain is usually on the left or on the right. It never occurs on both sides. Dr. Howell: ________________________________________________________________________________________ Ms. Sandler: I don’t think so… Let’s see... What do you mean by”radiate”? Dr. Howell: ________________________________________________________________________________________ Ms. Sandler: No, I don’t think so, although it’s often in my cheeks and around my eyes. Dr. Howell: So, let’s see if I got it right. Only one side of your head is affected, left or right, and it is around your eye and your cheek on that side. Can you show me exactly where it hurts? Ms. Sandler: Right here, doctor… and right over here … on the side. Dr. Howell: Got it. So, the pain is mainly at the front of your head and it involves a forehead, temple, eye and cheek. Does it ever hurt at the back of your head? Ms. Sandler: No, only at the front. Dr. Howell: OK. ____________________________________________________________________________________ Ms. Sandler: It’s especially bad in the mornings. It’s so unbearable that I can’t get up. It completely immobilizes me. Dr. Howell: _______________________________________________________________________________________ Ms. Sandler: I feel nauseated, sometimes even after the headache is gone. Dr. Howell: __________________________________________________________________________________________ Ms. Sandler: I wish I knew it, doctor. I think it’s stress that’s causing it. It’s not easy to run the restaurant by myself. I get so busy at times that I don’t have a minute to relax or eat. Then in the evening I will have a big meal and the headache will come on. Or when things go wrong at work, I can be so nervous that I would eat the whole bar of chocolate. Chocolate always aggravates it. And then, of course, I have another aggravating factor in my life. It’s my son. He is my biggest headache. I don’t know when he will grow up. Dr. Howell: You mentioned chocolate. ____________________________________________________________________ Ms. Sandler: Precipitate pain? Sorry, I am not sure I understand what you’re asking about? Dr. Howell: Well, I would like to know if there are any other foods that you think may bring on or cause the headaches. Ms. Sandler: Oh, foods that cause it… Well, I don’t know… It’s lack of food, if anything. I eat only one sit-down meal a day, and it’s usually late at night. I sometimes wonder if that’s what causes my malaise and morning sickness. Dr. Howell: __________________________________________________________________________________________ Ms. Sandler: I haven’t found any cures yet. Even the pain killers don’t always work. I was hoping that you would help me find the magic bullet. I really need my energy back. I can’t live like this any longer. Dr. Howell: __________________________________________________________________________________________ Ms. Sandler: I used to get some headaches, but I don’t remember them being so unbearable. Dr. Howell: _________________________________________________________________________________________ Ms. Sandler: No, not that I know of... Do you have any idea of what’s going on with me? Dr. Howell: Well, Ms. Sandler. I have some thoughts, but first I would like to run some tests and see if your blood work is OK. My notes indicate that you haven’t had a routine physical checkup for 3 years. Ms. Sandler: There’s just one more thing I wanted to share with you, Dr. Howell… I am embarrassed to tell you, but, you know, I’ve been feeling a bit depressed lately. Dr. Howell: OK, Ms. Sandler. Tell me more about it… When did you start to feel down? C. Compare your notes with a partner. Listen to the conversation again. During each pause, repeat the sentence or phrase you just heard. Then read it with your partner using proper pronunciation and intonation. Module 2 STUDENT HANDOUT H2:3 A. In the interview you have just heard, the physician tried to establish the following features about pain: character, intensity, onset, location, duration, timing, precipitating and alleviating factors, associated features, previous occurrences and family history. What is the typical question asked about every feature? Read the dialogue again and find those questions. Then record them in the right column of the table. Follow the example. Character: Intensity: Onset : Location: Duration: Timing Precipitating factors: Alleviating factors: Associated features: Previous occurrences: Family history: Please describe the pain. How does it feel? B. There are three primary types of headache: tension headaches, cluster headaches, and migraines. These three primary types account for about 90% of all headaches. Migraine Tension Cluster Severity of pain at least moderate in severity mild to moderate in severity very severe Characteristics of pain Precipitating factors deep, throbbing and pulsating dull, aching and pressure-like intense and stabbing bright lights; loud noises; strong odors; physical or emotional stress; changes in sleep patterns; exposure to smoke; skipping meals; hormones; certain foods (cheese, chocolate, peanuts, etc). long onset; may have prodromal stage (visual disturbances, vertigo, tinnitus, numbness or tingling of fingers or toes) One or both sides of the head; located around eyes, temples, cheeks, or forehead emotional stress, anxiety, hidden depression may be provoked by alcohol, tobacco, napping, or selected drugs like histamine or nitroglycerin sudden onset absent Pain develops gradually, fluctuates in severity and then can remain for several days More generalized pain on both sides of the head; with areas of more intense pain in the scalp, forehead, temples or the back of the neck. absent typical rare rare common more in females rare more common in females not common more in young males Onset Location of pain Runny nose and red, watery eye Sensitivity to light or sound Nausea or vomiting Sex predominance deep, stabbing pain around the temple or the eye; on one side of the head present Study the characteristics of each type of headache in the chart above. Based on the symptoms Ms. Sandler reported, which type of headache does she have? ________________________________ The two most prevalent types of migraine are migraine with aura (also referred to as classic migraine) and migraine without aura (referred to as common migraine). An "aura" is a physiological warning sign that a migraine is about to begin. An aura can occur one hour before the attack of pain and can last from 15 to 60 minutes. The symptoms usually include: bright flashing lights; temporary vision loss; wavy or jagged lines; vertigo, tinnitus (ringing in ears), numbness; tingling of fingers or toes; smelling strange odors, etc. Based on what Ms. Sandler has reported, what type of migraine does she have? ___________________________________________________ ___________________________________________________ Module 2 STUDENT HANDOUT H2:4 A. GRAMMAR NOTE. Indirect questions from WH-questions. Study the questions in the grammar box below and try to identify the difference between direct questions with BE, DO and DID and indirect questions with Can/Could you tell me…?, I would like to know if ..., Do you remember…?, I am asking if… Questions with BE How bad is your pain? Are there any other foods that precipitate the pain? Indirect questions Could you please tell me how bad the pain is? I would like to know if there are any other foods that precipitate the pain. Questions with DO or DID? Does the pain radiate anywhere? How often do you take pain-relievers? When did the problem begin? Indirect questions I am asking if the pain radiates anywhere. Can you please tell me how often you take pain-killers? Do you remember when the problem began? 1. In indirect questions with BE, the word order changes: BE occurs after the noun. How bad is your pain? Could you please tell me how bad the pain is? NOT Could you please tell me how bad is the pain? 2. In indirect questions with DO, DO/DOES/DID is omitted. How often do you take pain-relievers? Can you please tell me how often you take pain-killers? NOT Can you please tell me how often do you take pain-killers? When did the problem begin? Do you remember when the problem began? NOT Do you remember when did the problem begin? B. WRITING. Write indirect questions using these direct questions. Then compare them with a partner. 1. How long does the headache usually last? _______________________________________________________________________________________________________ 2. Are there any other symptoms that occur with this pain? _______________________________________________________________________________________________________ 3. What were you doing when your pain first started? _______________________________________________________________________________________________________ 4. How does your pain interfere with your work? _______________________________________________________________________________________________________ 5. Are you on any therapy to manage your pain? _______________________________________________________________________________________________________ 6. Is there a history of migraine headaches in your family? _______________________________________________________________________________________________________ 7. Did any family members in your home smoke when you were growing up? _______________________________________________________________________________________________________ 8. When did you begin to menstruate? _______________________________________________________________________________________________________ C. SPEAKING. With your partner, take turns asking the questions you wrote in Part B. Give your own information when answering. Follow the example: A: Could you tell me if there are any other symptoms that occur with this pain?B: Just before my headache starts, I usually see flashes of light. My mouth and hands are numb, my eyes are sensitive to light and my neck is feeling very tender. Module 2 STUDENT HANDOUT H2:5 SPEAKING: Role-play taking a history of pain using the following cases. Use the questions from the dialogue or from Chart D in H2:2 to gather the information about the pain in each case. Be prepared to improvise and add your own details as these case summaries contain only the basic information. CASE 1 Ms. Velasquez is a 22 -year-old female student. She has been suffering from migraine headaches since childhood. Her migraines have become worse once she began menstruating. They come most often at her period every month. They are also exacerbated during her exam sessions at school. She reports that a day before the onset of a headache she is very moody, forgetful and sensitive to light. When the headaches occur, she feels tired, lethargic and has problems with speech. She tried taking the birth control pill, but it only worsened her headaches and moods, so she discontinued it. She reports that painkillers provide very little relief, too. During an acute episode of migraine headache, the only thing that can slightly alleviate her pain is if she lies down in a darkened, quiet room and tries to sleep. Another thing that gives her a little comfort is a cold pack on her head. CASE 2 Ms. Stevenson is a 34-year old office-manager. She gets an intense burning pain on the outside of her foot when she walks. The pain usually goes away after a few minutes, but then there is a warm feeling in the foot that lasts for a few hours. Sometimes she doesn’t have any attacks for weeks and then she can have three in a day. The only thing that makes it better is to rub the foot and just wait for the pain to stop. She has noticed that her toes are numb during the attacks. She has had to stop wearing her tight, pointed high-heel shoes because she gets more attacks when she wears these. CASE 3 Ms. Howard, a 36-year-old female, has been suffering from neck pain and headaches since she had an auto accident 15 years ago. Her neck frequently "pinches" and causes headaches. After the accident, she was given muscles relaxants and physical therapy for four months with no results. Finally, she was prescribed cortisone shots in her neck and back, which also provided little relief. She discovered the activities that aggravate her neck and she tries to avoid those activities as often as possible. Some of them are: carrying her sons, holding the phone to her ear, lifting overhead, or certain exercises. In addition, she suffers from chronic unexplained knee pain in her left knee. She used to enjoy jogging on a daily basis but was forced to stop exercising due to excruciating pain. WRITING: Describe an instance when you or one of your family members were in a lot of pain. Indicate all the features of the pain (character, intensity, onset, duration, precipitating, aggravating and alleviating factors, associated features, previous occurrences and family history). Use the words and expressions from this module and follow the examples above. _______________________________________________________________________________________________________ _______________________________________________________________________________________________________ _______________________________________________________________________________________________________ _______________________________________________________________________________________________________ _______________________________________________________________________________________________________ _______________________________________________________________________________________________________ _______________________________________________________________________________________________________ _______________________________________________________________________________________________________ Module 2 STUDENT HANDOUT H2:6 COMMUNICATION TIP - The article below may help you improve your communication with patients. Read it carefully. Then answer the questions that follow. Treating the "Doorknob Syndrome" in Office Visits By Susan Davis http://www.allbusiness.com/4057870-1.html Picture this: You're 30 minutes behind on your appointments. You're just getting ready to leave an exam room when the patient says, "Can I ask you one more thing?" Begrudgingly, you say yes, hoping it's an easy question about vitamins or, perhaps, the art in the waiting room. Instead, the patient's face crumples and he says, "Is it normal for this mole to turn red and start to bleed?" Sound familiar? Such late-breaking questions are so common they have their own name: the "doorknob phenomenon," sometimes called the "doorknob syndrome" or "doorknob effect." And while some time-management experts might want you to make the patient come back another time, that's not the best way to practice medicine. Instead, here's how to get your patient to open up earlier in the exam. 1. Have some compassion. A lot of doorknob conversations come up because the patient was too embarrassed about the troubling symptoms to volunteer them during the actual exam. Sound silly? Put yourself in the patient's shoes. If you had a skin growth, erectile difficulty, or sudden bouts of depression, would you feel comfortable talking about it? 2. Work on your communication skills. Some doorknob conversations are the result of the doctor's demeanor. That is, a doctor who seems rushed or impatient can make a patient feel guilty about taking up time. Ask your family and staff about how you come across: Are you brusque? Rushed? Even slightly condescending? Such characteristics make it hard for patients to open and they will tend to hold their concern until the very end. 3. Let your patient talk. A study from the 1980s found that physicians start interrupting their patients after 18 seconds in the exam room. Such a steamrolling "I'm-the-expert-here" approach may seem like the best way to cut to the chase, but in the end, it can be self-defeating. Why? A patient who can't get a word in edgewise during the formal exam may stick it in just as she's reaching the door. And if it's urgent, you're duty bound to deal with it, even if it throws your schedule off. 4. Let your patient talk some more. Once he's told you what his first issue is, ask, "Is there anything else?" in a pleasant tone of voice. That simple question may give your patient just the entry he needs to get to his underlying concern. 5. Encourage your patients to write. Some physicians hand out forms on which patients can write their three most pressing questions for the day before going in to the appointment. This can help patients focus their thoughts. It also may be easier for some patients to write "lump on neck" than it is to ask what may feel like a silly (or terrifying) question. 6. Draw boundaries when necessary. Obviously, a patient who has suicidal thoughts or has a troubling lump needs to be dealt with compassionately, no matter when in the interview the subject comes up. But some patients may try to get an extra issue addressed to avoid making another appointment (an understandable tactic given everyone's busy schedules). For cases in which you think the patient is trying to economize on appointments, have some stock answers ready, such as: "That's an important topic. Let's make another appointment so that I can give it my full attention." That lets your patient know you care, even if you can't address the issue that very day. Post-reading Questions: 1. Have you ever experienced this “syndrome” as a patient or as a professional? _________________________________________________________________________________________________ _________________________________________________________________________________________________ 2. What is the cause of the syndrome? ________________________________________________________________________________________________________ __________________________________________________________________________________________ 3. Why is this phenomenon a problem for both patients and doctors? _________________________________________________________________________________________________ _________________________________________________________________________________________________ 4. Does it apply to doctors only or is it applicable to other health care professionals? _________________________________________________________________________________________________ _________________________________________________________________________________________________ 5. How would you address this problem in your practice? _________________________________________________________________________________________________ _________________________________________________________________________________________________