Mental Health Provider Letter

February 1, 2011
Dear Mental Health Provider,
HSCSN is notifying you of two important updates regarding the authorization process and documentation requirements for mental health services:
1.
It has come to our attention that many providers are providing psychotherapy notes in lieu of behavioral health treatment plans/outpatient treatment reports when requesting ongoing mental health services for enrollees. Effective immediately, HSCSN will no longer accept psychotherapy notes and will require the behavioral health treatment plan or an outpatient treatment report be submitted as documentation for continued treatment. A sample report is attached for your reference. This change will ensure compliance with the District of Columbia
Mental Health Information Act of 1978, which limits the disclosure of mental information to 3rd party payors.
2.
In order to improve provider and enrollee satisfaction, HSCSN is simplifying the authorization process for mental health services. Effective immediately, Care Managers will authorize services in the following manner:
Type of service Benefit Initial Authorization Continued Authorization requested
Medication
Management
Plan allows 12 visits/year
Requirements
Initial treatment plan
Requirements
Updated treatment plan or treatment report
- required every 12 months
Individual, Group and Family
Therapy
Plan allows 90 visits/six months
Initial treatment plan Updated treatment plan or treatment report
– required every 6 months
The treatment plan or treatment report must be received by the Care Manager within 30 days of initiating services and every six (6) to twelve (12) months for continued authorization, depending on the authorized service (see table).
Health Services for Children with Special Needs, Inc.
1101 Vermont Avenue, NW, Washington, DC 20005 202-466-8483 , www.hscsn-net.org
The HSC Pediatric Center 1731 Bunker Hill Road, NE, Washington, DC 20017 202-832-4400 , www.hscpediatriccenter.org
The HSC Foundation 1808 Eye Street, NW, Suite 600, Washington, DC 20006 202-454-1220, www.hscfoundation.org
HSC Home Care, LLC 1731 Bunker Hill Road, NE, Washington, DC 20017 202-635-5756, www.hsc-homecare.org
To reach an HSCSN Care Manager for authorization of medication management or psychotherapy services, please phone or fax:
Telephone: (202) 467-2737 Fax Numbers: (202) 721-7190, -7191, -7192 or -7193
If you have questions or concerns, please call your HSCSN Provider Operations Representative at (202) 495-7587.
Sincerely,
Cyd P. Campbell, MD, FAAP
Chief Medical Officer
Health Services for Children with Special Needs, Inc.
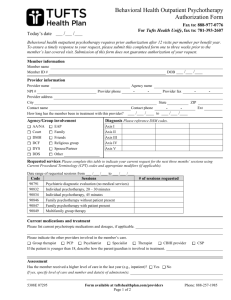
Attachment: Outpatient Treatment Report (SAMPLE)
Enrollee name:
ID#:
Initial Diagnosis
Axis I
Axis II
Axis III
Axis IV
Axis V
Outpatient Treatment Report (SAMPLE)
DOB:
No. of sessions since last review:
Date
Intake date:
Current Diagnosis
Axis I
Axis II
Axis III
Axis IV
Axis V
Purpose of Treatment Review
Change in diagnosis
Estimated length of treatment reached
Significant change in treatment plan
Change in treatment or therapist
Required periodic review
Increased or attempted suicidal concerns
Significant change in functioning level
Other:
Describe any changes in the client’s condition noted above:
__________________________________________________________________________
__________________________________________________________________________
Progress:
__________________________________________________________________________
__________________________________________________________________________
Setbacks/Impairments:
__________________________________________________________________________
__________________________________________________________________________
What actions are needed at this time?
Referral
Transfer
Psychiatric Evaluation
Psychological Evaluation
Physical Evaluation
Group/Individual/Family Therapy
Describe needed services:
3
Adapted from The Clinical Documentation Sourcebook
– The Complete Paperwork Resource for Your Mental Health Practice 4 th
Ed.
2009
Treatment Plan Review Refer to previous Treatment Plan or Treatment Review.
Current Goal 1
Describe current progress toward objectives:
Met yet?
Y N
Target date if not met yet
Current Goal 2
Describe current progress toward objectives:
Current Goal 3
Describe current progress toward objectives:
Current Goal 4
Describe current progress toward objectives:
Met yet?
Y N
Target date if not met yet
Met yet?
Y N
Target date if not met yet
Met yet?
Y N
Target date if not met yet
New Goal 1
Problem area:
Objectives:
Treatment:
Services (and frequency) needed:
Target date:
4
Adapted from The Clinical Documentation Sourcebook
– The Complete Paperwork Resource for Your Mental Health Practice 4 th
Ed.
2009
New Goal 2
Problem area:
Objectives:
Treatment:
Services (and frequency) needed:
Target date:
Therapist: Date: /
Address: ____________________________________________________________________
Phone Number: ______________________________
Fax Number: ______________________________
/
5
Adapted from The Clinical Documentation Sourcebook
– The Complete Paperwork Resource for Your Mental Health Practice 4 th
Ed.
2009