Case Report
advertisement
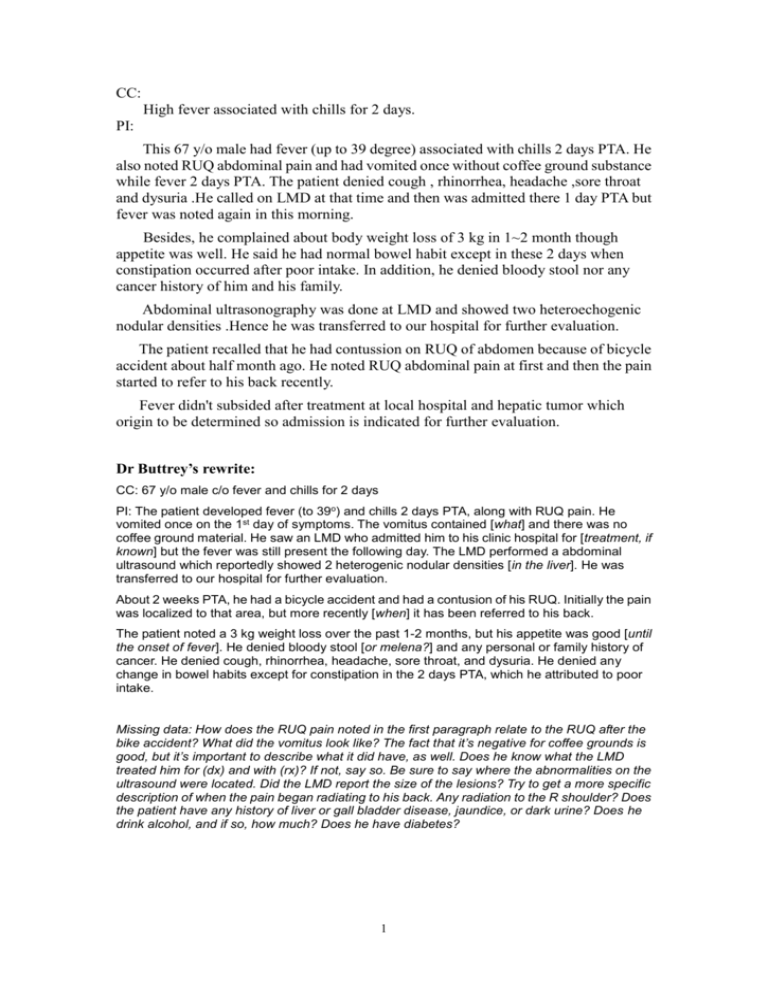
CC: High fever associated with chills for 2 days. PI: This 67 y/o male had fever (up to 39 degree) associated with chills 2 days PTA. He also noted RUQ abdominal pain and had vomited once without coffee ground substance while fever 2 days PTA. The patient denied cough , rhinorrhea, headache ,sore throat and dysuria .He called on LMD at that time and then was admitted there 1 day PTA but fever was noted again in this morning. Besides, he complained about body weight loss of 3 kg in 1~2 month though appetite was well. He said he had normal bowel habit except in these 2 days when constipation occurred after poor intake. In addition, he denied bloody stool nor any cancer history of him and his family. Abdominal ultrasonography was done at LMD and showed two heteroechogenic nodular densities .Hence he was transferred to our hospital for further evaluation. The patient recalled that he had contussion on RUQ of abdomen because of bicycle accident about half month ago. He noted RUQ abdominal pain at first and then the pain started to refer to his back recently. Fever didn't subsided after treatment at local hospital and hepatic tumor which origin to be determined so admission is indicated for further evaluation. Dr Buttrey’s rewrite: CC: 67 y/o male c/o fever and chills for 2 days PI: The patient developed fever (to 39o) and chills 2 days PTA, along with RUQ pain. He vomited once on the 1st day of symptoms. The vomitus contained [what] and there was no coffee ground material. He saw an LMD who admitted him to his clinic hospital for [treatment, if known] but the fever was still present the following day. The LMD performed a abdominal ultrasound which reportedly showed 2 heterogenic nodular densities [in the liver]. He was transferred to our hospital for further evaluation. About 2 weeks PTA, he had a bicycle accident and had a contusion of his RUQ. Initially the pain was localized to that area, but more recently [when] it has been referred to his back. The patient noted a 3 kg weight loss over the past 1-2 months, but his appetite was good [until the onset of fever]. He denied bloody stool [or melena?] and any personal or family history of cancer. He denied cough, rhinorrhea, headache, sore throat, and dysuria. He denied any change in bowel habits except for constipation in the 2 days PTA, which he attributed to poor intake. Missing data: How does the RUQ pain noted in the first paragraph relate to the RUQ after the bike accident? What did the vomitus look like? The fact that it’s negative for coffee grounds is good, but it’s important to describe what it did have, as well. Does he know what the LMD treated him for (dx) and with (rx)? If not, say so. Be sure to say where the abnormalities on the ultrasound were located. Did the LMD report the size of the lesions? Try to get a more specific description of when the pain began radiating to his back. Any radiation to the R shoulder? Does the patient have any history of liver or gall bladder disease, jaundice, or dark urine? Does he drink alcohol, and if so, how much? Does he have diabetes? 1 Comments Content: The history sounds most consistent with liver abscesses, probably related to the trauma several weeks previously. However, the history of prior weight loss is a little worrisome, and hepatoma or possibly liver metastases need to be considered. Either one would be less likely to present with fever and chills, but it is possible. If liver cancer is being considered, then risk factors for it should be noted, positive or negative. It would be worthwhile to state in the PI whether he has otherwise been healthy. Diabetics seem to be at higher risk for liver abscess, so this would be something to note as either positive or negative. If he is diabetic, I wouldn’t describe here. I would just state that he has it and then write “(see PMH)” where the details should be written. The history is well written. I changed the order somewhat in my rewrite, but there is nothing wrong with the original order. The HPI tells a story, and each story-writer relates things in a slightly different way. You made good use of a number of important negative findings which help us to focus in on the liver as the most likely source of his illness. English: called on LMD: We usually write “saw” or “went to.” “Called” (without the “on”) would be used if he phoned him to ask for advice. I doubt if that’s a common practice in Taiwan. Also, you need an article or pronoun before LMD (“an LMD” or “his LMD”). Besides, he complained about...: This is a Chinese sentence pattern. 而且他也.... Although we sometimes say this colloquially, it is not equivalent to 而且 and should not be used in this way. Alternatives are: “He also c/o...,” “In addition, he c/o...,” “In addition to the fever, he also c/o....” Or, don’t add anything extra. Just state the complaint. (See the sentence as I wrote it in the 3rd paragraph.) body weight: This is not incorrect, but we usually don’t bother with the word “body.” It’s obvious from the context that that’s what you are talking about. This is again the influence of Chinese, where you must say 體溫 , not just 溫. That’s not necessary in English. appetite was well: The appetite was “good.” “Well” is an adverb that should only be used to modify a verb, e.g., he was eating well. An exception is its use in describing one’s general health. “How are you?” “I’m well, thank you.” 2