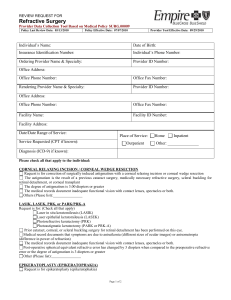
Refractive Surgery
advertisement

Refractive Surgery The History of Refractive Surgery Forerunners to Modern Refractive Surgery o Leonardo da Vinci- Early 16th C Italian scientist, philosopher, artist Contemplated the possible source of visual disturbances. o Johannes Purkinje o Hermann Snellen- 1869 Dutch Ophthalmologist Proposed using incisions across the steep meridian of the cornea to flatten it. Also hypothesized the concept of astigmatism. o Hjamar Schiotz- 1885 Norwegian Ophthalmologist First to make “Limbal Relaxing Incisions” in a patient who underwent cataract surgery, altering the shape of the human eye. Incisions made in the steep corneal meridian flattened it. Early Non-Surgical “Techniques” o Eye cup with a spring-powered mallet designed to flatten the cornea (early ortho-K?) o Firm rubber bands to flatten the cornea. Lans- 1898 o Dutch Physician o First to think of changing the shape and power of the cornea by making incisions on the anterior corneal surface. This defined the principles of “keratotomy” surgery to correct refractive errors. Tsutoma Sato and the early 1930s o Japanese Ophthalmologist. o In 1939, he observed that the spontaneous breaks in Descemet’s membrane in keratoconus patients produced a flattening of the cornea. He also observed that the flattening of the cornea due to injury to Descemet’s membrane was greater than that caused by injury to Bowman’s layer. This lead Sato to conclude that surgery on the posterior cornea would be more effective than surgery on the anterior cornea. He became the first to perform surgeries on the cornea (refractive keratotomy) to help correct myopia. o In the early 1950s, Japanese patients would receive as many as 80 incisions on the anterior and posterior cornea to correct myopia and astigmatism. The role of the corneal endothelium to maintain corneal thickness and clarity was not fully understood in Sato’s time. Many patients eventually suffered severe corneal edema requiring corneal transplantation. Jose Barraquer- 1940s o Columbian Ophthalmologist, One of the fathers of lamellar surgery. o Barraquer performed a procedure called keratomileusis in which he removed a section of the anterior cornea, similar to today’s flap, via an instrument that he invented called a microkeratome. This was handcranked. He then froze it, reshaped it with a cryolathe, and then sutured it back onto the patient for improved vision. Luis Ruiz- 1987 o Columbian Ophthalmologist. Protégé of Barraquer that modified his technique. o He used an automated microkeratome without the freezing of the cornea. This was called “Automated Lamellar Keratoplasty,” ALK, or the Ruiz technique, and it was used to treat high amounts of astigmatism using transverse corneal incisions. Svyatoslav Fyodorov- 1972 o Russian Ophthalmologist o Fyodorov studied these surgical techniques and laid ground rules on how a surgery will be successful. He said that the correction of refractive error would result from a certain depth and length of the incisions, as well as their distance from the limbus. Fyodorov also varied the amount of uncut clear zones between incisions. He determined that most of the “RK” flattening effect was achieved in 16 or fewer incisions on only the anterior cornea. This preserves the corneal endothelium, thereby avoiding the problems that Sato’s patients suffered. This new technique triggered a stampede of surgeons traveling to Moscow to learn about RK, making Fyodor the modern day father of RK. Dr. Leo Bores- 1980s. o Dr. Bores, an ophthalmologist in Arizona, finally brought these surgical procedures to the US. o NIH sponsored the PERK study (Prospective Evaluation of RK) in 1980. Drs John Taboada and Steve Trokel- 1981 and 1983 o American Ophthalmologists o These doctors were amongst the first to propose the use of the excimer laser for RK, ablating large areas of tissue. Dr. Margeurite McDonald- 1987 o Louisiana Ophthalmologist o First to perform PRK on a sighted human eye. This patient is reported to still be 20/20 today. Drs. Ionnis Pallikaris and Lucio Buratto- 1990 and 1991 o Greek and Italian Ophthalmologists o First to combine Barraquer’s Keratomileusis technique with PRK. o Pallikaris coined the term LASIK. Types of Refractive Surgery Definitions Keratoplasty- corneal graft or corneal plastic surgery Keratotomy- surgical incision of the cornea Keratectomy- surgical excision of the cornea Keratomileusis- surgical removal of a thin segment of the cornea Radial Keratotomy (RK) This is an outdated procedure for low myopia in which a surgeon, using a magnification system, makes a series of radial incisions (typically 4-8, up to 16) in a symmetric pattern in the cornea, to reduce its curvature by weakening the peripheral cornea. The depth is up to 90-95% of the corneal thickness at the edge of the optic zone. The number of incision is related to the magnitude of refractive error. This procedure has a longer healing period than LASIK, and is more painful postoperatively. Short-term Complications o Corneal Edema Seen in 93% of patients, the normally mild edema usually spares the optic zone. It occurs in cases in which the cornea has been kept wet or has had excessive irritation of the incisions following surgery. Generally the edema resolves without treatment within 2 weeks. o Monocular Diplopia This is caused by the vertical folds in Descemet’s Membrane within the optic zone. The folds and diplopia usually disappear by 4 months, thus the best management would be reassurance to the patient. o Cataract Formation This is not very common. It can result from direct lens injury during the surgery. o Haloes and Glare These are produced by the corneal scars and are especially noted at night when the pupil dilates, exposing the ends of the incision, making night driving difficult. This is generally self-limiting, beginning to diminish 3-4 months post-op and gone for the most part after one year. It can be treated with anti-reflective coatings, tinted lenses, and a miotic drop if night driving is too problematic. o Over, uncorrection, induced astigmatism Incisions that are too shallow, too few, too short, or made in the wrong axis can result in induced astigmatism. These patients can be managed by referring them back to the surgeon to correct the deficiency. Timing is important for these corrective methods. Other management would be spectacles (wait min of 2 weeks), HCL (wait 6 weeks), SCL (wait 8 weeks), and LASIK. For overcorrection, any hyperopia greater than 1D and lasting more than 6-8 weeks is likely to remain, therefore it can be classified as a long-term issue. The administration of 1% Pred forte qid has been shown to reduce the overcorrection by as much as 1D. In addition, Pilocarpine has also been shown to reduce overcorrection after RK. Longterm Complications o Hyperopic Shift According to the PERK study, the rate of hyperopic progression during the first 2 years was 0.21D per year. From 2-10 years, it declined to 0.06D/year. The shift is only prevalent in about 2% of the operative population. The degree of hyperopic shift was directly proportional to the degree of preoperative myopia. This continual hyperopic drift is desirable in undercorrected patients but can cause problems for the newly emmetropic patient. Because of this issue, some surgeons plan on undercorrecting patients to provide a protective buffer against the hyperopic shift. o Diurnal Fluctuation A diurnal myopic shift of 0.5-1.0D was observed in 33% of operated eyes. This may result from the diurnal change in corneal hydration in unstable wounds. The newly flattened cornea is weaker than the cornea once was. The condition is self-limited, but it may not go away completely for many years. Attempts to fix these patients with HCL had not shown to be successful. The SCL fitting is not recommended before 8 weeks because of the danger of neovascularization of the incisions. RK Enhancements o This type of surgery has become very conservatively performed, due to the fear of overcorrecting the patient. Enhancements can be even more painful than the original surgery. There is an increased morbidity and cost to both the patient and doctor. o Correcting Undercorrection Incisions can be made deeper. The optic zone can be reduced by making the incisions longer. More incisions can be added. o Correcting Overcorrection The incisions can be sutured individually or via a purse-string suture to avoid gaping. ALK is the treatment of choice with a significant overcorrection, and is a valid option after 12 months post-op. o AK Doctors need to be more aggressive with ATR than WTR astigmatism. Topography should be utilized on a cornea that has been stable for a minimum of 4 weeks. o LASIK A year after RK, LASIK can be used to correct for under/overcorrection. It can also reduce corneal haze. Astigmatic Keratotomy (AK) This employs the same technique as RK. Incisions are used to “relax” the corneal tissue and produce a rounder shape. It is frequently combined with the RK procedure. Astigmatism is corrected with the combination of assymetical and tangential incisions. There are infinite variations of this procedure which include differences in depth, length, shape, and number of incisions. Because it is similar to RK, the complications are the same. Photorefractive Keratectomy (PRK), aka Advanced Surface Applanation (ASA) Introduction o Longest track record, safest laser procedure, longest healing period. o Can be used as primary or clean-up. o Used for low to moderate myopia (up to -7.00). History o 1987- First PRK done on a sighted eye. o 1995- First FDA approved procedure in the US o 2005- Renewed interest in the PRK. Advantages o Better visual quality after PRK is for those patients with higher expectations for visual perfection. This is one reason why the military almost exclusively uses PRK. o Certain patients prefer to avoid a “flap.” Recent litigation against LASIK is making patients more cautious. This procedure is also not involved in as much litigation against the surgeons. PRK eliminates the complications that could arise due to the flap. This is good if the patient is involved in contact sports. o Increased understanding of high risk corneas. This includes thin corneas (<500 microns or <30 micron difference between central and peripheral pachs), decentered central pachs possibly due to asymmetric astigmatism, those with irregular topographies (>2D difference between inferior and superior K readings, posterior floats >55D and/or >40 micron elevation, “sagging” or decentered anterior and posterior floats), ABMD, FF Keratoconus. PRK treating on the surface has less chance to destabilize an abnormal cornea and eliminates any risk of microfolds. This causes much less chance of creating post-laser ectasia. o PRK can be used for enhancement over irregular flaps or as a laser treatment over old RK. Patient Counseling o Explain why PRK recommended. o Disadvantages include increased discomfort and delayed vision recovery. o Advantages include No flap complications More residual tissue Navy pilots have same procedure Same vision outcome as LASIK (or better) Pre-Op Considerations o All the same pre-surgery measurements o Topo, orbs, cycloplegic rx, DFE, pupils, wavefront analysis. PRK Pre-Op Meds o Restasis and Artificial Tears o Zymar qid day before. o Ibuprofen 400-600mg qid day before? o Vit C, E o PO Doxycycline, EES ung if blepharitis/meibomitis Procedure o PRK uses an excimer (UV) laser to vaporize the surface of the cornea and “sculpt” a new shape. o First the epithelium needs to be removed. Alcohol Brush/ Manual Scrape Laser LASEK The epithelium is scored with a trephine and loosened with a topical 18-25% dilute colvent (alcohol or methyl cellulose) to soften the top layer of the cornea, then rolled back, preserving it to some extent in one piece. The thought is that this will have less corneal scarring with a cut closer to the surface, but currently there are no lasers FDA approved for this procedure. This is an “off-label procedure” There is a chance of the cornea “falling apart.” Epi-LASIK This uses new epi-keratomes to create a 40-50 micron epiflap for better preservation of the epithelium. No alcohol is used. o The surgeon then photoablates the cornea and folds the epithelium back on the cornea. o Mitomycin C This is an antibiotic/chemotherapeutic agent that inhibits DNA synthesis. The incorporation of Mitomycin C intraoperatively has reduced the incidence of scarring and haze following high risk PRK, including post-incisional keratotomy, high myopia, post-LASIK enhancements, and following Intacs with thin corneas. The surgeon places a sponge soaked in Mitomycin C on the cornea for about 60-120 seconds after the laser is performed. The disadvantage is that it may delay re-epithelialization. o A bandage CL is generally used post-surgery. This speeds recovery. o Painful because it leaves nerves exposed. o Heals in 7-10 days (F/up every other day) Post-Op o Create realistic expectations for recovery. The biggest challenge is managing psychological aspects of decreased comfort and slower visual recovery. Be prepared for more follow-up and hand-holding. o Post-Op Follow-Up Day 1, Day 4-5 to remove the BCL, Week 2-3 if necessary Month 1 and 3 Avoid refractions for one month post-op. o Meds Antibiotic (Zymar) qid for one week. Steroids Pred Forte 1% Qid x 1 week, tid x 1 week, qd x 1 week Pain Management Recently there is increased pain management. Cold compresses or ice packs Acular LS q2h to qid 2-4 days Keep eyes closed/ Sleep Better fitting overnight BCLs PO Ibuprofen PO steroids Comfort drops (2ml diluted tetracaine) prn Hydrocodone (vicodin) q4-6h prn Neurontin (Gabapentin) 1200mg po x3-4 days o Normal Epithelial Healing The epithelium will usually heal within the first 4-5 days. Do not be alarmed if it takes a bit longer. Usually the BCL is removed at day 4-5. If in doubt, leave the BCL in additional 1-2 days. Once the BCL is removed, reassess the epithelium and then replace with a new BCL if necessary. Caution, because this may increase pain and delay healing. o Vision Recovery Day 1 20/40-20/80 Days 2-4 20/40-20/200 Day 4-5 20/30-20/80 VA rapidly improves 2-3 days after removal of BCL removal as the epithelium thickens and smoothes out. Day 5-6 Driving vision (local) Day 7-10 Good vision Weeks 4-6 Excellent vision Complications of PRK o Complications are rare. o Post-PRK Haze Late onset corneal haze and decreased visual acuity can occur from one to several months after surgery. It usually resolves over time, but severe cases may require corneal debridement and treatment with MMC. o o o o Grade 1 Grade 3 Infection Pain Delayed vision recovery Elevated IOP (steroid responder) Grade 2 o Corneal melt o Hemosiderin Post-RK Automated Lamellar Keratoplasty (ALK) Aka keratomileusis in situ, advanced corneal shaping, lamellar keratoplasty. For high amounts of myopia (11-15D), the surface layer of the cornea is separated using a microkeratome. This flap is folded back and a thin disc of corneal tissue is removed by a second pass of the microkeratome. The flap is then returned to its original position. With increased prescriptions, RK would be performed after ALK. Since planar slices are removed from an oblate cornea, it causes the cornea to be irregularly shaped. There is less success with this procedure since it is very imprecise. Myopic Keratomileusis (MKM) A microkeratome is used to resect a thick corneal cap which is frozen, lathed and then sutured back onto the cornea. Epikeratophakia A superficial portion is removed from the eye and replaced with a donor disc. LASIK LASIK is a combination of ASA and ALK. This procedure uses a microkeratome to produce a flap of corneal tissue that is lifted so that an excimer laser can sculpt the corneal shape underneath to achieve the desired topography. This can be used for myopic and hyperopic prescriptions. Advantages o Allows for same-day surgery on both eyes. The actual surgery takes only minutes, about 10 seconds per diopter. o No pain during the surgery and post-op pain is relatively low. o Rapid visual return and return of normal sensation. This allows most patients to return to work the day after. Refraction stabilization is generally obtained within weeks. Off all medication in 4-7 days o Avoids the risk of anterior stromal haze and pain associated with PRK. o Preservation of Bowman’s, optimizing corneal stability. o Reduced infection risk, making bilateral surgery safe. o Less corneal impact than wearing SCL History o 1996- US clinical trials begin o 1999- FDA approves the LASIK procedure Good candidates o Some doctors will perform LASIK on children under certain circumstances when all other corrective methods have failed, i.e., those with ADD, high anisometropia (congenital or trauma induced). o Prescription Up to 11D of myopia Up to 6D of myopic astigmatism Up to 6D of spherical hyperopia Up to 2D of hyperopic astigmatism. o Occupational benefits Law enforcement officers that have to perform under extreme circumstances. Glasses can be knocked off or broken and contact lens wearers have difficulty with tear gas. Firemen- Glasses cannot fit under fireman’s gear and contact lenses are irritated by smoke and debris. Same with forest rangers. Lifeguards save lives in conditions containing sand and salt water. Glasses are not feasible for water rescues and sand and salt are not compatible with contact lenses. Athletes- Glasses slide and fog up from swear and contacts may not stay in the eye during contact sports. Travelers- Contacts and glasses are a hassle to keep clean and spares are hard to keep on hand Pilots- Glasses and contacts can cause safety hazards if dislodged when flying. Airlines set their own policies with respect to LASIK. Airline policies are evolving and more pilots are having it done. o Recreation Water sports including scuba, water skiing, wakeboarding, tubing, jet skiing, wave runners, river rafting, kayaking, etc. Water spray causes droplets on glasses and can wash contacts out of eyes. Sports including football, water polo, swimming, volleyball, gymnastics, etc. Outdoor recreation including camping, mountain biking, hiking, etc. Cleanliness and sanitation are difficult in the outdoors. Contraindications o Uncontrolled DM o Pregnancy o Inability to wear CL o Cataract formation o Both eyes cannot be corrected better than 20/40 o Abnormally thin corneas o High correction and astigmatism o Dry eyes (TBUT <6sec) o Large pupils. Pre-Op o Advice to patients Do not choose a surgeon on price alone. Beware of promises of 20/20 (30% do not achieve this) Does not cure presbyopia Cannot be reversed. Relatively new procedure- long term effects unknown Results may not be lasting. Procedure Overview o An anesthetic is used before a microkeratome (the knife) is used to slice off a very thin layer of the cornea, leaving a hinge on one end. A computer controlled excimer laser is used to remove a precise amount of the corneal stroma. Then the flap is flipped back and allowed to heal. o The only pressure felt is with the vacuum (90mmHg) o Alignment rings made so the flap can go back into place. Creating the Flap o Flap creation is usually at the surgeon’s discretion and preference, and the design of the flap is usually a superior or nasal hinge. o Types Steel Microkeratomes The surgeon affixes the microkeratome to the eye using a suction applicator, and then the foot-controlled, motordriven blade slides over the cornea and creates the thin flap. Waterjet Keratomes Laser Keratomes (Intralase) 1053nm wavelength with brief laser pulses Epikeratomes/ EpiLASIK Creates a flap without a blade and delaminates the corneal epithelium above Bowman’s Membrane without the use of alcohol. A platic separator splits the two layers at their natural junction, causing less trauma to the eye. The Excimer Laser o Designed in the late 1970s, this is a “cool” laser beam (low heat) of unequaled precision. It is high energy, so that it can split the C-C bonds. A mushroom cloud occurs when this happens. o It can removes 39 millionths of an inch of tissue in 12 billionths of a second, producing very sharp edges. 4 pulses/sec, 1/4u/pulse = 1u/sec (12u/D) Laser Systems o Alcon Surgical- LadarVision 4000 o Nidek- EC 2000 and EC 5000 o LaserSight- LaserScan LSX o Bausch & Lomb- Technolas 217c o Visx VSS (Variable Speed Scanning)- Star Smoothscan S3 and S4 o Wavelight Laser Technologie AG- Allegretto Wave o Asclepion- Meditec AG- MEL 70 G-Scan o Schwind GmbD & KG- ESIRIS Machines o Alcon Ladarvision 4000 A flying (scanning) spot with beam size of 0.8mm and optic zone size of 6.5mm with a blend out to 9.0mm. Requires dilated pupil More precise. Important devices Broad beam to narrow beam laser Tracking devices detect movements 100-4000x/sec, allowing surgery to be performed on those with nystagmus. Parameters o Bausch & Lomb 217A Zyoptics Excimer Laser Designed to couple with the most advanced corneal diagnostics. Optic zone size of 7.0mm with a blend out to 9.0mm. “Flying spot” software can create any size/shape of incision. This allows for better peripheral vision due to decreased aberrations and haloes. Pupil dilation is not required. Decreased neosenephrine means less vasoconstriction and less edema, meaning less flap wrinkling. Tracking technology Sampling rate: 120Hz = 8.3msec The laser calculates the center of the pupil which becomes the tracking reference that guides the scanning system. Unmatched VA in FDA studies to date 99.7% 20/40 or better 87.3% 20/20 or better 30.3% 20/15 or better Parameters o Visx Star S4 CustomVue Laser This is used for primary treatments only. Variable Spot Scanning (VSS), variable beam sizes (0.65-6.5), variable repetition rate (VRR), active track 3-D active tracking and active track automatic centering. Optic zone size of 6.0mm with a blend out to 8.0mm. Parameters o Zeiss Meditec Flying spot with beam size of 0.7mm. Extremely fast laser at 250Hz. Video-based tracker. -10.00/ 4D cyl o Allegretto Wavelight Excellent vision quality Good night vision No degradation of vision with astigmatism correction. Decreased enhancement rates <3% overall, <1% in myopes up to 7D Parameters Wavefront History of “Wavefront Technology” or “Adaptive Optics” o Julius Feileib, PhD- 1980-89 o Robert Fugate, PhD started the “Starfire Project” 1982-1991 o David Williams, PhD is a vision scientist from 1991-present o Larry Thibos, PhD- 1992-present o Ray Applegate, OD, PhD- 1995-present Introduction o This applies the principles of adaptive optics, and offers us ways of assessing lower and higher order aberrations of the eye. The optics of the human visual system are far from perfect. Aberrations o Aberrations are errors of the entire eye. Over 65 total aberrations have been identified. There are two types. Lower order aberrations include sphere and cylinder. Higher order aberrations include coma and spherical aberrations. o Causes Low order aberrations are due to the fovea. High order aberrations are due to changes in the corneal curvature. The cornea is prolate. This is normally fixed by the pupil and its diameter. Surgery creates an oblate cornea, meaning that it is flatter. The visual axis must be kept in an aspheric orientation. The crystalline lens also directly affects lower and higher order aberrations. This changes with age, unlike the cornea. It becomes more spherical (oblate). In the earlier years, the lens makes the CLC 0, because it corrects the cornea. Under 20 years of age, the spherical aberration of the cornea is about -0.26. That of the lens is +0.26. Between the ages of 20-30, the spherical aberration of the lens changes to about +0.52, the +0.78 about 30-40 years of age. >40 years, it can increase to about +1.04. o Currently, glasses and contact lenses and conventional excimer laser ablations can only treat lower order aberrations. The problem is that these always induce higher order aberrations. The magnitude of induced spherical aberrations is directly proportional to the pre-op magnitude of myopia. o Why do Conventional Ablations Induce HOAs? Laser ablation algorithms were developed by testing ablation profiles on flat pieces of plastic, but the cornea is a dome. Central spots are round and match the ablation of a piece of plastic. Peripheral spots are oval with larger surface area and therefore lower fluence. Peripheral spots are partially reflected and not completely absorbed. o Lower Order Aberrations (80-83%) Measured by Traditional refraction: Subjective and Objective Automated refraction Computerized refraction Keratometry Corneal topography Here the goal is “20/20.” Types Name Description st 1 Order Tilt (Prism) 2nd Order Defocus (Sphere) and Cylinder o Higher Order Aberrations (17-20%) Measured by wavefront analysis Measures lower and higher order aberrations. This is generally objective with a subjective refinement capability. It measures to 0.05u (0.005D) o 3u = about 0.25D Here, the goal is 20/8 This is dependent on pupil size. For every 2mm increase in pupil size, HOA increases 100%. Avg is about 3.5. Eliminating or decreasing HOAs is “probably” good. Increasing HOAs is “usually” a problem. Changing a person’s HOAs is “always” bad. This is because the brain “learns” vision. Types Types Name Description 3rd Order Coma Overlapping with tail following Trefoil Multiple Tails Primary Causes o Corneal geometry o Corneal remolding o Biomechanical insult o Induced by the keratectomy in the LASIK procedure Effects o Reduces mesopic and scotopic vision 4th Order Spherical Symmetrical Aberration degradation. This is seen as a “starburst,” decreased contrast, and decreased night vision Quadrefoil Primary Causes o Strongest influence on human optics o Media changes o Crystalline lens changes o Diffraction of light o Induced by corneal laser photoablation Effects o Reduced mesopic aand scotopic vision o Glare, halos, starbursts o Reduced contrast sensitivity 5th Order Distortions/ Irregular Astigmatism 6th-11th Increasing levels of irregular astigmatism RMS System (vs. Diopter) and “Marechal’s Criterion” o RMS deviations (Root Mean Square) = √w(r,Ø)2 This is the measurement of aberrations of an optical system (coma, spherical aberrations, distortion, defraction, etc). The lower the RMS, the better the visual acuity. Lowest potential RMS for the eye is about 0.07u, which is Marechal’s Criterion. An RMS of 0.07u can produce a visual acuity of 20/6, which is thus the maximum potential visual acuity of the human eye. This is “Super Vision.” o But…. There are neural and retinal considerations There are 4-7 million cones in the retina. The maximum number of cones in the fovea is about 5 million. Visual acuity resolution threshold for 5 million cones is only about 20/8. This becomes the “Super Vision.” Traditional Refraction o Methods of Measurement Traditional subjective and objective refraction for: Plano (Piston) “0” Order Aberrations Prism (Tilt) 1st Order Aberrations Sphere (Defocus) 2nd Order Aberrations Cylinder (Cylinder) 2nd Order Aberrations Automated objective refraction Computerized subjective and objective refraction Keratometry for corneal cylinder Corneal topography for corneal cylinder, asymmetry, warpage, etc. Refractive Issues o Zernike’s Polynomials (Coefficients) RMS values mathematically converted to 2 dimensional (color maps) and 3 dimensional models describing the shape of a specific aberration. All aberrations are measured in RMS units and a “point spread function” which is an easier way to analyze vision. o Red indicates a positive aberration. Blue is negative. o >0.4 RMS is clinically observable. o A change of >0.2 RMS is clinically observable. Points Spread Function are also used, which is an easier way to analyze vision. o The appearance of a spot of light on a black background, i.e., a star in the sky. o Negative would be black spot (or image) on a white background, i.e., a Snellen chart. Therefore this can be used to measure higher order aberrations. It is referred to as the “Poor man’s aberrometer.” Wavefront Technology o Laser photoablation relative to current refractive measurements Phoropters measure 0.25D levels. Keratometers and topographers measure corneal curvature and elevations in 0.25D steps. In linear measure, one order of magnitude larger about 3 microns equals 0.25D. But, excimer lasers can ablate tissue at as little a rate as 0.25 microns per pulse. o o o o Thus, the level of potential accuracy for correcting refractive errors with an excimer laser (0.25 microns) is 12x greater than our current ability to measure refractive errors. Wavefront Aberrometry Basic Principles Shack Hartmann (3 excimer platforms)- 250 points at once. Ray tracing aberrometry (Tracey)- 120, but one at a time. Tscherning Aberrometry (Subjective) Spatial Skiascopy (Marco 3D Wave) Holographic Imaging (Ophthonix) Fourier Analysis (Visx) o This is the measurement of output vs. a piston. Dynamic Spatial Skiascopy- Scanning This can be corrected with lenslets, and is called Adaptive Optics Aberrometers Alcon Ladarvision (LadarWare) Nidek EC-5000 (OPD-10000) LaserSight LSX (AstraScan) Bausch and Lomb Technolas 217 (Zyoptix) Visx WaveScan (WavePrint) Tracey Visual Function Analyzer (VFA) Complete Ophthalmic Analysis System (COAS) Topcon Aberrometer (KR-9000PW) WaveLight Allegretto (WOSCA System) Laser Photoablation Relative to Wavefront Analysis Measurements Whereas the level of potential accuracy for correcting refractive errors with an excimer laser (0.25microns/pulse) is 12x greater than our traditional methods of measuring refraction (3microns or 0.25D), wavefront analysis can measure refraction down to 0.05 microns (or 0.005D). Thus, wavefront measures 5x more accurately than an excimer laser can correct (0.05 vs. 0.25 microns) and 50x more accurate than standard refractive techniques can measure (0.005 vs. 0.25D). Custom Ablation This decreased higher order aberrations, but physics and corneal healing limit its effects to lower order aberrations only. Cells grow back at different times. Diagnostic Applications of Aberrometry Evaluating all eyes not correctable to 20/20. Assessing static vs. dynamic visual differences. Comparing objective to subjective point spread functions. Differentiating corneal from lens aberrations. Pre and post posterior capsular opacification (PCO) effects Evaluating post-op IOL tilt, decentration, multifocal optics. Assessing cataract patients’ symptoms and “quality” of vision. Assessing contact lens candidates for soft vs. hard lens wear. Contact lens care including Ortho-K. Pre and post-lens fit integrity, quality, and results. Monitor progress and visual effects from varying ocular pathologies and surgeries. Pathologies o Cataracts o Keratoconus o Others Surgeries o Lid and oculoplastic procedures Ptosis and chalazia induce vertical coma o Others Post surgical or medical therapy monitoring of refraction Evaluating corneal aberrations secondary to certain lid and ocular surface pathologies Lids o Blepharo or dermatochalasis o Chalazia and lid tumors Ocular surface o ABMD o Corneal dystrophies and degenerations o Pterygium o Tear-film dysfunction o DES (K. sicca) o Others o Potential diagnostic and treatment implications in measuring lower and higher order “instability.” Vision and refractive problems Contact lenses considerations Ocular surface disorders Quantifying dry eye syndromes Refractive surgery patients Wavefront o Conclusions Wavefront guided ablations minimize the magnitude of HOAs. In patients with significant pre-op HOAs, wavefront guided ablations reduce the HOAs. Wavefront guided ablations are necessary to perform enhancements on refractive surgery patients who are symptomatichalos, glare, ghosting of images, and poor quality of vision. o Readouts Aberrations are represented by a “root mean square” measure. Myopia Hyperopia Mixed Astigmatism Coma Sperhical Aberration o Orbscan o Aberrations above the 6th order are inconsequential. These actually only introduce “noise” from tear film debris and instability, vitreous floaters, and corneal disruptions. o RMS values can vary between blinks, mostly due to tear film dynamics. o A patient whose RMS value is greater than 0.3microns has visually significant higher order aberrations and would benefit from wavefront. o Those that benefit most from wavefront are those with larger pupils, larger prescriptions, astigmatism, and higher RMS values. Most patients with large puils, whatever their refractive error, would probably benefit from wavefront. o In general, this is less likely to induce new aberrations than traditional LASIK. o Problems: Wound healing is unpredictable. Wavefront is dynamic and correction is static. Wavefront changes daily, as well as with age. o Types of Lasers Conventional Wavefront Guided (Custom) Treats both spherocylinder and HOAs Wavefront Optimized (Custom) Designed to treat spherocylinder errors without affecting HOAs, especially spherical aberration. Topography Guided (Custom) Poor predictability. Need to know apex. Rings depend on distance. laser inability to ablate desired shape. Used with asymmetric astigmatism, irregular corneas, and previous corneal surgeries. Waiting for FDA approval. o VISX CustomVue Aberrations in Normal Eyes o o o o o SA- 0.13 +/- 0.07 microns Coma- 0.17 +/- 0.09microns Total HO RMS- 0.31 +/- 0.10 microns Aberrations in normal eyes: Pre-Op Alcon CustomCornea SA- 0.15 +/- 0.07 microns Coma- 0.21 +/- 0.09 microns Other- 0.23 +/- 0.09 microns Total HO RMS- 0.37 +/- 0.10 microns Aberrations in Normal Eyes: Post-Op Alcon CustomCornea SA- 0.25 +/- 0.10 microns Coma- 0.36 +/- 0.11 microns Other- 0.33 +/- 0.10 microns Total HO RMS- 0.58 +/- 0.12 microns Summary of Aberration Change with CustomCornea LASIK SA- +0.11 microns (30% improved) Coma- +0.16 microns (25% improved) Other- +0.11 microns (30% improved) Total HO RMS- +0.21 microns (36% improved) High Order RMS Standard LASIK increases HO RMS Predominantly SA Custom LASIK maintains or decreases HO RMS Facts Increased amounts associated with loss of BCVA Increased amounts associated with loss of contrast sensitivity Reduced amounts associated with better quality of vision. Wavefront Optimized Optimized profile is created by adding more laser spots to the periphery. Compensates for Reflected spots Ovalization (cosine effect) Preserves pre-op asphericity = prolate shape of cornea. WaveLight Allegretto Wave Excimer Laser System utilizes a wavefront optimized ablation in all of its conventional ablations. Advantages o Faster 200 Hz Pulse Rate = ~4.5 sec/D o More predictable Faster treatment means less time for drying, etc. o Very precise 0.95mm Gaussian-shaped beam diameter. o Better optics Wavefront optimized built-in to all treatments. o Safer Fast, pulse to pulse tracking (<6mSec) Wavefront optimized ablations are a good choice for most eyes. Most eyes do not have significant asymmetric higher order aberrations. Of those that do, many have the aberrations in the lens. Lenticular aberrations should not be corrected on the cornea. Can lead to worsened aberrations and will degrade with time. Induced spherical aberration is the major cause of night driving complaints after LASIK. Lasers other than the Alegretto can only minimize induced spherical aberrations with their wavefront guided ablations but not with their conventional ablations. The Allegretto is the only laser to provide this advantage (minimal to no induced spherical aberrations) in all conventional treatments by utilizing wavefront optimized ablations. Treatments do not worsen night vision The FDA studies showed most patients had improved night vision after LASIK with the Allegretto. Most patients do not need to have lengthy custom work-ups. <15% receive custom treatments internationally with the Allegretto. Faster, more comfortable treatments with better optical results. o “Guided” vs. “Optimized” Optimized is a conventional treatment Optimized prolate ablation pattern is based on a population averaged wavefront. Optimized may only address spherical aberration. Optimized = one size fits all. Guided addresses all HOA in a particular patient Existing and induced Symmetrical and asymmetrical. Wavefront guided treatments are not needed in most cases with the Allegretto. It is still needed in laser with non-Wavefront Optimized ablation profiles. All procedures induce aberrations. Need is to minimize induced aberrations or decrease as many of them as possible. o Conclusions Customized ablations are most beneficial for patients with asymmetrical topography and significant HOAs. Speed of ablation and amount of tissue removed per diopter of correction are important factors to be considered. Accuracy of outcome is more important than induced HOAs as long as the amount of induced HOAs is not significant. The ideal laser is fast, accurate, and induces minimal to no HOAs and reduces pre-existing HOAs. Tissue removal Wavefront guided > wavefront optimized > conventional Aberrometers o Bausch & Lomb Orbscan- Zyoptics Anterior segment analysis system Must know this with all pre and post op. Only system that scans the anterior and posterior, as well as pachymetry, recognizing the weakest points, predicting keratoconus. Can estimate VA under low light conditions Zyoptics option Wavefront guided corneal reshaping Minimizes the risk for haloes and glare. If you experience a poor quality vision now with your glasses or contacts. If you have had laser surgery before and wish to consider a refinement. o Zywave II Wavefront Aberrometer Hartmann Shack Technology A narrow laser beam is focused on the retina to generate a single, focused point source. Outcoming light rays are bent by aberrations caused by all refracting media (cornea, lens, vitreous) Light ray bending is detected by an array of lenses. Adaptive optics flattens the wave aberration Technology to eliminate higher order aberrations by evening the cornea From NASA. Who is a candidate? This is a highly sophisticated decision made between an experienced doctor and the patient. It is made on an individual basis based on the probability that we will meet the patients expectations for vision improvement and the activities that the patient most wishes were uncomplicated by eyewear. o Ladar Intralase/ IntraLASIK o This is an improved flap procedure. o Femtosecond Laser This laser contains extremely high power attained at relatively low energy. Each pulse of focused laser light lasts about 10-15 seconds (500-800 femtoseconds). Programmable Parameters Flap thickness, diameter, centration, hinge angle, side cut angle. The laser creates a cleft of water and CO2 via an excimer laser. o Structure of IntraLase Flap Smooth Stromal Bed Precise Flap Thickness Larger standard deviations generally reported for mean LASIK flap thickness with mechnical microkeratomes. o 10-15 microns for intralase (avg 12) o 15-35 microns (avg 24) Uniform Thickness UTZ pachymetry is the current method of measuring flap thickness, but it measures the central point only and does not measure uniformity. Visante OCT measures anterior segment with high precision and resolution, so it can measure the flap thickness and stromal bed. Biomechanically stable. Corneal Biomechanics o The way that the cornea is set up is responsible for its shape with certain loads. There is a structural stability. The lamellar structure of the cornea means that peripheral fibers contribute to strength, as well as deeper fibers. Cutting larger flaps can cause ectasia. Mechanical Microkeratome Flap o A microkeratome cuts deep in the periphery with poor diameter and centration control. This leads to variability in central thickness across different flaps, as well as significant variability regionally within a flap. This confirms earlier studies using regional subtraction pachymetry. IntraLase Flap o An intralase cuts thin planar flaps with precise depth, diameter, and centration control. Minimal variability in central thickness across different flaps, as well as minimal variability regionally within the flap. This confirms earlier studies performed with regional subtraction pachymetry and histology. The angle of the cut also has less chance to epithelial ingrowth. o Clinical Experience 300 lasers installed worldwide. 500,000 LASIK flaps performed. In the US, 20% of LASIK flaps are done with this. o Clinical Results Tran, Sarayba et al. JCRS Jan 2005 Randomized, prospective Contralateral- blade vs. intralase 9 patients, 18 eyes Flap cut only Measured flap-induced HOA Excimer treatment 10 weeks after flap Durrie, Kezirian, JCRS Jan 2005 Randomized, prospective, contralateral eye Blade vs. intralase 102 eyes Noted better visual outcome with intralase. Also less HOA. US Navy Study (Schallhorn, Tanzer) Comparison of visual outcomes with femtosecond and mechanical keratomes for WFG LASIK. Return to flight status sooner. Best technology for flap creation. Methods included hansatome, Amadeus, intralase, and Visx excimer laser in 300 patients Conclusions: o WFG LASIK approach favors intralase Better clinical results Faster visual recovery Improved mesopic low contrast VA o No significant difference in overall HOA based on keratome use. Amadeus induces more spherical aberration Both Amadeus and hansatome induce more horizontal coma compared to intralase. Lindstrom, Davis Blade vs. intralase More IL patients achieve 20/20 Better flap thickness predictability Costs more but patients willing to pay. Biomechanics, Alio JL et al. Compare biomechanical response of ocornea after myopic LASEK, IntraLase LASIK, and blade LASIK. Lower biomechanical response with intralase, followed by LASEk, then blade LASIK. F Price ARVO 2006 Reduced epi ingrowth in retreatment. Significantly less epi ingrowth with LASIK enhancements if the original LASIK was done with intralase compared to mechanical microkeratomes. Why? o Bladed microkeratomes all have a tapered or gradual entry into the cornea. o All FLS cases had either a 65 or 70 degree side cut from the lamellar dissection to the anterior surface of the cornea. o Summary Smooth bed Uniform flap, small hinge Thin, uniform Better VA o o o o o o o o o o o o Better HOA Better biomechanical effect Creates an inflammation A: no keratome This creates the flap through photodisruption and hydrodissection of the stromal tissue. Specifically, it creates thousands of 2-3 micron capitation bubbles within the cornea. This technically destroys tissue and creates a space in which the flap can be separated from the bed. This demonstrated more predictable flap thickness, better astigmatic neutrality, and decreased epithelial injury. Can predictably create flap diameters, hinge location and flap thickness while eliminating the risk for cap perforations. Risks come from the energy and fluid from the IntraLase yield more corneal edema, and patients typically require stronger steroid drops for a longer period. Flap creation with the IntraLase can take 1-2 minutes, depending on the surgeon, vs. less than 30 seconds with the microkeratome. This can lead to increased pain and discomfort. Flap complications such as striae/microfolds, buttonhole flaps, epithelial ingrowth and infection occur at approximately the same rate with either procedure. A newer keratome, the Hansatome Excellus with the Zero Compression Head, creates ultra-thin flaps, but IntraLase does create a flap with a more uniform thickness from edge to edge. IntraLase can also be used to create the lamellar channels for Intacs and for therapeutic anterior lamellar keratoplasty. Inflammation? The FS laser produces greater corneal stromal inflammation than the MM early postoperatively without any increase in apoptosis and stronger flap adhesion late postoperatively. Therefore, it may require stronger anti-inflammatory drugs to be administered. Early post-op inflammation Injury to corneal epithelium. Apoptotic keratocytes and inflammatory cell infiltrations. PMNs are the first cells to migrate into the corneal tissues in response to injury. o Highly differentiated cells. o Found in the limbus and wounded areas within the first 2 days after corneal injuries. With cells on day 1, need to return the next day. o The density of the PMNs start to decline by the third day. Treatment with steroids and irrigation? Flap Adhesion Strength Forces required to detach the flaps at one month: Intralase FS group 126.7g of force. Mechanical microkeratome group 65g of force. Forces required to detach the flaps at 3 months Intralase FS group 191.3g of force. Mechanical microkeratome group 127.5g of force The grams of force needed was significantly higher in the FS group than in the MM group at 3 months. (P<0.05) o HOA Comparison in Fellow Eyes Following LI LASIK with Wavelight Allegretto and CustomCornea LADAR 4000 Systems Conclusions Both laser platforms produced accurate refractive outcomes. Statistically significant difference found for spherical aberration correction at 1M and 3M. No statistically significant differences in Low and high contrast acuity. Patient preference. Further study enrollment is underway. o Complications Flap related complications- 8.3% Includes thin flap (buttonhole, striae), thick flap (ectasia), incomplete flap, decentered flap, small/large flap. Interference by gas bubbles In the anterior chamber o The gas bubbles can get into the anterior chamber via the peripheral cornea and trabecular meshwork. o If the bubble is large enough, it may prevent pupil margin tracking by the laser and inhibit the patient’s ability to focus. o Bubbles absorbs into the aqueous humor in 2-3 hours and treatment may be completed. In the cornea o The bubbles may get into the anterior stroma and are not released upon the lifting of the flap. o Depending on the location of the deep opaque bubble layer, the pupil or iris landmarks may be obscured, preventing either pupil localization for tracking and/or iris landmarked-based iris registration. o These usually resolve in 30-45 minutes. Unliftable Flap Attempts to forcefully open the interface with patulas and blades may lead to torn flaps or rough or irregular surfaces. Etiology is uncertain, but appears to occur bilaterally in individual patients. There iften is some keratocyte activastion and associated interface haze. This is corticosteroid sensitive and resolves with treatment within 3-4 months with no effect on vision. If this occurs, abort the procedure. Allow 1 months for healing and reattempt with a blade keratome set to cut the flap 50 microns deeper than the original femtosecond flap interface. Nondissected Islands Sometimes for various reasons, the laser will skip over a spot, causing the undissected zone to be not seperable. Forceful attempts to delaminate the corneal collagen fibers in this area can result in a tear through to the surface, leaving an isolated “island of undissected tissue similar to the central islands that may occur with blade microkeratome-created flaps. This can occur with thin flaps, through incision such as after RK or PK and through scars such as after previous microbial keratoplasty or CK. Allow it to heal for 6 weeks and then recut the flap with a blade microkeratome at a level of at least 50 microns deeper. Transient Light Sensitivity Patients have reported severe photosensitivity 6-8 weeks after LASIK. This has been called Track-Related Iridiocyclitis and Scleritis (TRISC), Good Acuity Plus Photosensitivity (GAPP), and Transient Light Sensitivity (TLS). It is still unclear as to what causes the syndrome. Treatment with a topical steroir for 1-4 weeks resolves the symptoms. Patients with good vision develop photophobia in the absence of any apparent finding on examination. Corticosteroid drops are prescribed and symptoms improve within 1 week. Sunglasses should also be work for the period. Etiology is unknown, but speculation is around keratocytes activation to laser-induced iritis, scleritis, or neuritis. Seen in about 1% of patients. Keratitis Intrastromal inflammation may be localized around the edge of the flap, which can occur 2-7 days after flap creation. The area appears hazy or white. Photophobia. It is associated with cellular infiltration in the interface and in the superficial cornea in a narrow band along the edge of the flap. Results from microscopic corneal tissue damage caused by the laser photo disruption, perhaps exaggerated by exogenous inflammatory factors in the tear film. Treatment includes frequent topical corticosteroid drops. In rare cases, the inflammation is severe, and scarring may develop in the area of the side cut and haze in the interface. LASIK Surgical/Procedural Complications o Decentered treatment zones, laser-related complications and irregular astigmatism can result from such factors as patient;s excessive eye movement during surgery, loss of eye tracking by the laser, incorrect programming of the treatment computer or improper/inaccurate measurements taken during the presurgical evaluatioin. These can lead to a decreased visual outcome. If possible, retreating the eye is the best management, but glasses or CL correction may be the only option. o Thin Flaps If the microkeratome does not have enough suction, the improper size microtome blade is used, or patients squeeze their eyes excessively during the procedure. This is difficult to replace and position. Treatment is usually delayed until the flap has healed. o Buttonhole Flaps Ring-shaped flaps with a central hole or thin area. Performed without adequate suction or the microkeratome is improperly positioned. This produces a meniscus-shaped flap that is thinner in the center. Replace the flap and allow it to heal before performing any excimer treatment. o Free cap/flap Flap lacks a hinge. Usually results from a loss of suction during the keratome pass and causes shallow engagement of the keratome on the corneal surface. Treatment can proceed if the treatment zone has sufficient ablation area. Replace the flap and cover it with a BCL. Monitor it for the development of irregular astigmatism or epithelial ingrowth. o Full perforation This is rare. Suturing of the cornea is required and no further surgery was usually performed. o Dislodged Flap Can be an early or late complication. Early flap dislocation can result from poor flap placement after surgery or patient induced by squeezing of the eyelids or rubbing. The surgeon should immediately reposition the flap to decrease the chance of DLK, striae, and epithelial ingrowth. Post-Surgical Complications o Dry eyes Affects majority of all LASIK patients, most common. Temporary or longterm. Generally mild. Patients predisposed to dryness before the surgery may have moderate to severe symptoms. Symptoms Redness, excess watering, burning, excess mucous, sandy gritty feeling, blurry vision Causes Severed corneal nerves, damaged goblet cells, deficient tear oil layer, altered cornea elevation, incomplete lid closure/blink. Results from the creation of a temporary neurotrophic cornea from severing the corneal nerves during the creation of the LASIK flap. This leads to decreased corneal sensation and decreased feedback to the lacrimal gland and reduced tear production. Treatment AT, gels, restasis, punctal plugs. o Halos, glare, and starburst Halo effect is an optical effect that is noticed in dim light. Halos are concentric blur circles that surround a point source like a car headlight when viewed at night and occur when the optical treatment zone size is smaller than the mesopic pupil size. Glare is the distortion radiating from light sources at night. Wavefront guided retreatment is the best solution. These are usually self-limiting, beginning to diminish 3-4 months and are gone for the most part within a year. Can be managed with AR lenses, as well as tinted of photochromatic lenses. A mild miotic may be prescribed to help with the patients night activities, especially driving. Causes Dependent on amount of correction being done (larger corrections have higher risk) Larger pupil size have higher risk. Prevalence 1/50 (glare) o Contrast sensitivity Ability to discern images of varying shades from the background is diminished. Symptoms Decreased night or low light vision linked with glare, haloes, or starbursts. These usually subside within 1-3 months. o Reduced VA Improper programming of the excimer laser, incorrect positioning of treatment zone or complications in the healing process such as excess scarring or flap wrinkling. o Sand of Sahara (aka Diffuse Lamellar Keratitis) Inflammatory reaction underneath cornea flap. This is a multifocal and/or diffuse inflammation confined to the flap interface. It generally starts in the periphery and appears 2-6 days after surgery, but it may not be present until as late as 6 months after surgery. Symptoms It may be asymptomatic or accompanied by mild to severe blurring, redness, and discomfort. Photophobia and tearing are also seen. NOT an infection. Causes Unknown. May result from either a build up of bacterial endotoxin in the wet autoclabe reservoir, talc from gloves, meibomian gland secretions, microkeratome oil, or blade debris. Grading 1 o Description 1-10 days post-op Focal white to gray granular material under the LASIK flap. Easily mistaken for SPK, but it is not on the surface rather at the stromal interface. No anterior chamber reaction/ quiet eye. Normal VA o Treatment Topical Pred 1% steroid qh FU 1-2 days with gradual taper. 2 o Description Moderate density of interface material with potential clumping or coalescence Slightly reduced BCVA Quiet eye Often present with temporary hyperopia with astigmatism o Treatment Topical PF 1% qh FU 24 hours If worse, may require lifting flap and irrigating inflammatory cells from interface. 3 o Description Dense accumulation of interface materials Reduced BCVA typically 20/30 – 20/60. Hyperopia with astigmatism Possible slight conjunctival injection but not anterior chamber reaction o Treatment Consider lifting flap and irrigation of interface with saline and steroid Topical PF 1% qh Evaluate in 24 hours. 4 o Description Very dense interface material Reduced BCVA worse than 20/50-20/60 Difficult to get refraction Conjunctival injection with rare anterior chamber reaction May develop striae in the flap o Treatment Lifting flap and irrigation with saline and steroids ASAP Topical PF 1% q30-60min FU 24 hours Resolving Sands with Striae Prevalence 1/500 Treatment If untreated, it may extend into the central cornea and lead to a progressive decrease in VA. Frequent/aggressive use of eye drops (corticosteroids). Q12h Flap lift and irrigation may be required for more severe cases. Severe cases left untreated can cause corneal scarring and ultimately lead to vision loss. o Infection/ Infectious Keratitis. Sterile Infiltrates o o o o This is rare. It is usually acquired intraoperatively and caused bu G+ bacteria, atypical mycobacteria, fungus, or virus. It presents early with isolated infiltrates, corneal inflammation, conjunctival injection, and in severe cases, with an anterior chamber reaction. Treat any suspected infection immediately. Double vision (Monocular Diplopia) Symptoms Secondary image tends to be more opaque Causes Due to irregular astigmatism (hills and valleys in the cornea that bend in strange directions) resulting in multiple images on the retina. Overcorrection/undercorrection/ induced astigmatism Overcorrection occurs when the laser has removed too much tissue. Undercorrection occurs when the laser has not removed an adequate amount of tissue Symptoms Noticeable blur 10% of patients need re-treatment (enhancements) to correct vision after LASIK may need to continue to wear glasses to help correct the vision problem. Over and under response is more commin in higher prescriptions. Refer back to surgeon for enhancement before 3 months so that the flap can be easily reflected and manipulated. Haze Flap Striae These are wrinkles or folds in the flap which usually occur immediately after replacement of the flap or during the initial healing of the flap. Striae appear as vertical lines on a nasal hinge flap and horizontal lines on a superior hinge flap. Treatment involves removing the striae by smoothing the flap which should be performed as soon as possible. 1 Description o Seen early post-op first days. o Very faint lines o More common with high refractive errors o Not associated with reduced acuity. Treatment o Generally not clinically significant and none required. 2 Description o Seen early as distinct lines, single, or in clusters. o Mild reduced acuity and subjective reports of “qualitative problems.” o Retroillumination with dilated pupil is absolute best technique to observe. o Delayed viewing following fluorescein instillation may help seeing grooves. Retro Treatment o Flap needs to be lifted and repositioned within 1-3 days for optimal results. o Striae that affect BCVA do not “go away” or resolve on their own and much better results occur with prompt treatment. o Evaluate patient in 24 hours. o Occasionally BCL are applied to enhance comfort and stability. Description o Seen first few hours post-op or from trauma o Marked striations o May have discomfort due to flap displacement o Gutter of the flap may have gap and increases risk of infection and/or epithelial ingrowth. o Reduced acuity from moderate to severe Treatment o Repositioning and alignment should be done immediately. o Epithelial compromise or other conditions may warrant a BCL along with appropriate antibiotic treatment. o Evaluate patient in 24 hours. o Rarely if striae do not respond to lifting and stretching, appropriate suturing techniques have shown to be beneficial. 3 o Epithelial Defect o Fiber Debris Under the Flap o Debris with inflammation under flap o Epithelial Ingrowth This occurs in up to 20% of LASIK cases. It is related either to contiguous migration of cells from the edge of the flap or direct inflammation of cells in the interface during the LASIK procedure. It can progress to cause irregular astigmatism or to induce melting of the overlying flap. Although a definitive cause is still uncertain, it appears to be associated with epithelial defects at the time of surgery, history of recurrent corneal erosion, hyperopic correction, repeated LASIK treatments, flap instability and/or ABMD. Treat with topical steroids. More severe cases require lifting of the flap and scraping the epithelial cells from the stroma. 1 2 Description o Grey to white fine deposit typically at or near the flap edge. o Only 1-2 cell layers thick appearing as thin haze or may be in small clusters (1-2mm) o Noted early 1-10 days post-op o No subjective complaint or acuity change Treatment o Observation in 5-10 days o No treatment usually required o Typically thin layers of epithelium die and if a fine white line is noted along the leading edge of the ingrowth, it is not likely to progress. Description o Dense opaque accumulation in small clusters of a sheet which extends up to 2-3mm from the flap edge. o May approach pupillary axis if aggressive. o VA affected if central location o Flap edge may appear hazy Treatment o Non-urgent observe closely to prevent progression to edge retraction or flap melt. o If progresses flap is lifted and epithelial cells are cleaned out of interface. 3 Description o Thick opaque accumulation often geographic presentation larger than 2mm o If at the flap edge probably melt and/or retraction of flap, possible discomfort o Vision may be affected if encroaching visual axis o Epithelial defect possible over site of ingrowth if melt occurs. Ingrowth with Flap Melt Retroillumination Treatment o If in visual axis or flap melt occurs, should treat ASAP o Can result in permanent loss of BCVA if not resolved in time. o Loss of BCVA o Corneal Ectasia This is one of the more difficult complications and potentially the most visually devastating. A progressive anterior shift of the cornea associated with central steepening and thinning, myopic shift, and visual symptoms. Severe cases often require a PK. Other cases managed with RGPs or intacts. Possible causes Residual corneal stroma, coreal modulus, corneal flap thickness, IOP, apoptosis of corneal cells. Regression o This is reported more often with high-myopic and hyperopic LASIK. this is caused by post-op epithelial and stromal hyperplasia resulting in corneal steepening. These patients are referred back to the surgeon for LASIK enhancement. Additional ablation requires very precise calculation of the stromal bed thickness because often the underlying stromal bed is too thin to permit additional ablation. Enhancements o 20/ Unhappy Patient Evaluation Careful manifest refraction with BCVA SLE o o o o o R/O TF problems R/O epithelial ingrowth R/O flap microstriae RGP Test R/O Cataracts and macular problems 15% of all surgeries require some form of enhancement. 82% of those only required one operation. Surgical enhancements are usually required if less than optimal outcome has occurred or if previous surgical treatment has regressed to cause a symptomatic refractive error. Initial under correction and epithelial hyperplasia are usually the common causes associated with enhancements. Risks depends on the original rx Myopes around 6% With cyl over 3D about 10% Myopes >9D and hyperpes around 11-15% Pre-op Examination History Uncorrected monocular VA BCMVA Careful manifest dry refraction PreVue Lenses- directly comes from the aberrometers Cycloplegic wet refraction Schirmer test Ant seg examination Pachymetry/ ultrasound Pupillometry (IR) Corneal topography Dilated post. seg examination Wavefront aberrometry Pre-op considerations How soon should we enhance a patient? Rule of thumb: 1 month for every diopter of primary ablation. Must have 2 consecutive similar refractions, corneal topographies, and normal aberrometry (less than 0.50D change) Must have wet rx on all enhancement procedures Corneal thickness Must leave 250-275 microns in bed. If not, it could lead to ectasia. Must leave 400 microns overall. Never go deeper than 50% original thickness. Beware of epithelial hyperplasia o The cornea attempts to “fill-in” the corneal depressions. Associated with abrupt change in corneal curvature. Rule out by performing PIB (Patch In Bed). Pre-op pach – ablation depth > postop pach. Beware of corneal ectasia o Seen first in the posterior cornea. Average depth 18.3 microns/D Depth range: 14.9 – 22.9 microns/D (varies due to wavefront) Deppest part of ablation not necessarily central Retreatment depths as much as 50microns/ D Glare is multifactorial Pupil size Flatness of keratometry Residual refractive error Anterior chamber depth Media opacities Smoothness of media (striae, ingrowth, opacities) High order aberrations o What to Watch out for Keractasia Bent Bow Tie Pellucid o Wavefront Maps High spherical aberrations may be closely associated with LASIK postoperative night vision complaints of glare. High amounts of trefoil are commonly found in patients complaining of starbursts at night. Asymmetric aberrations such as trefoil and quadrafoil may give rise to patient symptoms of monocular diplopia and triplopia. o For post-Custom LASIK patients, recommend Custom LASIK enhancement, especially if there is a loss of BCVA or subjective visual symptoms resolved with phoropter/trial frame correction. You might want to wait for the next generation customized treatments. If there is satisfactory vision, standard LASIK could be performed. Must be careful regarding over-corrections with patients with large amounts of HOA (SA) Adjust treatment +0.25 for every 0.1 microns > 0.20 of symmetrical HOA. o Cap Mgmt Lift or recut? Generally lift flap. There are poorer results with recutting. Timing o A recut has been safely performed as soon as 8 weeks post primary LASIK, but it is recommended to wait 3-9 months. o A lift has been safely performed 27 months after primary LASIK but the recommendation has been to consider a recut after 12 months. Recuts o This used to be more common, because it was thought to be faster with a decreased chance of inducing epithelial ingrowth. Today the technique and instrumentation of flap lifting have both improved. Recutting has the advantage of not involving flap manipulation, especially if the flap is thin or perforated. o Pachymetry Pacymetry – (250bed + old cap160) = residula for ablation after lift E.g., 450 – 410 = 40 microns Pachymetry – (250bed + 200new cap) = residual for ablation after recut (unless at same depth) o o o o E.g., 450 – 450 = 0 microns Interface fibrosis, or after 12 months pre-op If minimal pach, recut at same depth after 12 months Lasik, post RK….one cut per year History of recurrent ingrowth o Correcting Striae This can be corrected with a sequential lift and suture technique. It eliminates the need to fixate the flap with forceps during suturing and increased accuracy of suture placement. o Great for the correction of residual myopia and/or astigmatism, following RK PRK haze, following incisional surgery, has been associated with a 30% chance of loss of 3 lines of BCVA Haze prophylaxis o Mitomycin C- 0.02mg/ml for 2 min o Inhibits haze after primary high PRK o Inhibits haze following PRK after RK o Lower risk than use in glaucoma filtration surgery (0.4% for 2 min) LASIK is the procedure of choice for residual or consecutive refractive errors after incisional surgery (RK)- Ideal. Methods o Previous incision RK, +/- AK o Visually significant refractive error, with BCVA >2 lines over UCVA o No epithelial inclusion cysts in incisions. Inclusions encourage ingrowth o General Rules UCVA 20/40 or 20/unhappy Not zero risk Pachymetry is only one limiting factor Supplemental P/T Spec Rx? Resist small monovision adjustments o Case Studies Decentered Ablation with Induced Vertical Coma 53 yo female presents with complaints of glare, multiplopia, and “smeared vision” in left eye. S/P LASIK for -8D spherical myopia. -1.75 -1.25 x 090 20/25. Topo shows superior decentered ablation. Patient undergoes wavefront-guided enhancement. 3 mo. Post-op pt pleased with quality of vision. MR -0.50DS 20/20. wavefront refraction -0.66 -0.49 x101. Vertical coma -0.48. OZ nearly centered on topo. Poor vision after PRK -6.25 -1.00 x120 OD, -6.75 -1.00 x055 OS. PRK OU 1995 with ablation zone 4.5mm. Post-op complains of poor quality vision and glare- ou. OD: -1.75 -1.50 x165 20/30 OS: -1.00 -1.25 x025 20/30. Scotopic pupils 7mm, Pachymetry 49-/505 Amadeus microkeratome 9.0mm diameter flap with 140 plate to achieve a 120 micron flap. Visx custom ablation OU. Physician adjustment +0.35 OU Poor vision after LASIK -6.25 -1.00 x120, -6.75 -1.00 x055. LASIK 2000. Post-op complains of poor quality vision and glare- OU. Bilateral Striae, flap suturing OD, hyperthermia OS. Residual striae OD (best seen with dilation, and retro on DO). -0.50 -0.50 x114 20/30, -1.00 -1.25 x025 20/20. Scotopic pupils 5.5mm, pachs 480 MO Combined Visx S4 PTK with 6mm ablation zone without blend zone of 50 depth. Scraping of peripheral epithelium to 9mm. wavefront PRK with 7mm optical zone and 9mm ablation zone. Ablation depth 28.5 (6/8 treatment ablation depth 19). Topical mitomycin C 0.02% for 2 min. 38yo white male. CEO large bank. Ocular/systemic history unremarkable. DW soft CL D/C x4 weeks. OD: -7.50 -1.25 x010 20/20, OS: -9.50 -0.50 x008 20/20-. Dry = Wet RX. OD Dom. K: 44.25/45.50 x180- OU. Pupil (scotopic) 7.0mm OU. Pachs 554/551. Normal topos. Bilateral LASIK 03/24/99. Hansatome 160 plate/8.5 ring. Summit apex. Uneventful (double card) surgery. Post-op: UCVA 20/20, 20/70-. BCVA OD plano 20/20, OS +3.25 -3.50 x105 20/30+. Biomicroscopy normal. Patient is “miserable”, nausea, dizzy, vertigo. “I cannot ride in trains or cars without closing eye.” 1st enhancement: Dry = Wet +3.25 -3.50 x105. Alcon Autonomous LADARVision 4000. Recut with Moria LSK 150. Post-Op: UCVA 20/70. BCVA +3.50 -3.50 x105 20/30. No change in rx! Cannot correct with soft toric. RGP 20/20 but cannot tolerate. Suture flap. UCVA 20/20 BCVA plano 20/20. Remove sutures. Within 2 weeks Rx +3.50 -3.50 x105 20/30. WaveScan Rx -1.99 1.66 x024. Repeatable on multiple aberrometers. Repeatable wet or dry. PreVue lens 20/20 clear. Healing o In minutes to hours. Not fully complete until about 2 years. o Fibrin o Physical attraction o Endothelium and negative pump Cost o On the average, the price of LASIK has been decreasing. The average price of LASIK was 1655 per eye in the 1st quarter in 2001. This decrease in price is because of an increase in consumer interest and co-management of laser centers. Currently there is no universal standard regarding price of refractive surgery. This is good when thinking about the amount spent on contacts or glasses every year. o What the fee covers A portion of the purchase price of the laser. Laser maintenance, excimer laser manufacturer fee Surgical devices, gowns, gloves, masks, and other sterile surgical tools. Insurance Running the surgical center: staff salaries, advertisements, rent, and other office equipment Surgeon’s fee Standard pre-op and post-op visits. Maybe touch-ups. o Method of payment There are medical flex plans where you set aside pre-tax dollars from your paycheck for medical expenses. You can earn a federal tax deducation if you itemize your medical and dental expenses, because LASIK surgery is a medical expense. Because LASIK is in high demand, insurance companies are beginning to offer benefits for the procedure. Some insurance companies already offer to pay for a portion of the LASIK surgery and care. Laser Thermal Keratoplasty (LTK) A holmium laser is being evaluated for correction of small amounts of hyperopia. The technique uses a laser to tighten the tissue fibers in the peripheral cornea in an attempt to steepen its curvature. Uses the “Sand Principle” o Produces heat generating spots that coalesce to steepen the cornea. 16 pulses of Holmium: Yag delivered simultaneously to 8 spots on a 6mm and 8 spots on a 7mm optical zone 1.4sec exposure times per ring. Adaptation can take months, so not used as much. Good for hyperopes. Machinery o Sunrise Hyperion LTK System- expensive Conductive Keratoplasty (CK) Uses controlled release of radiofrequency thermal energy (instead of a laser) to heat and shrink the corneal tissue. The energy is applied at points in a circular pattern around the peripheral cornea. The heat creates shrinkage and all point pull together via striae that form. This acts as a ring of tightening that steepens the cornea. The result reduces the need for reading glasses. There is a temporary induction from -1.00 - -2.00D of myopia to improve near vision in the non-dominant eye. The limited range is -1.00 - -2.25D or treatment with 16-24 spots. 86% of patients in this range achieved both uncorrected distance vision of 20/20 or better and near vision of J3 or better. This was originally approved by the FDA in 2002 to treat +0.75 - +3.25D of hyperopia, with up to -0.75D of cyl. In February 2004, it was approved for presbyopia. This does not affect the DVA. The first FDA approved technology for presbyopia. It induces a progressive/aspheric effect (a multifocal cornea effect). The distance vision improves, and the near benefit remains. “Blended vision” The stainless steel handle is 450 microns (corneal needle is 400 microns), so need a 510 micron cornea. It delivers 350 kHz radio frequency energy placed in a series of circumferential spot applications to the mid-peripheral cornea. This causes the corneal collagen to contract like a belt, resulting in the steepening of the central cornea. The effect of CK is determined by the number of spot applications, the number of rings of applications, and the diameter of the application rings. Marks at 6, 7, or 8mm. With +1.00, monovision is sufficient. Do bilateral with high hyperopes. Lower tech, but higher durability Non-laser, in-office, correction of spherical hyperopia. Surgeon-friendly. Deteriorated accommodative ET? Candidates o At least 40 years old o No eye disease o Need “readers” o Realistic goals Less dependent on glasses Read a menu See my watch Mark my golf card See the compuer Features o Treats Farsightedness Astigmatism Presbyopia, even after LASIK correction o Induces permanent change o Utilizes harmless “radio waves” Procedure o Topical anesthesia o Takes about 10 min per eye o The instrument resembles a slit lamp. o AT and sometimes antibiotic and steroid drops are used one week post-op. o Some FBS and fluctuation in vision will occur. o Treatment usually lasts for 1-4 years. Patients can be retreated but outcomes for retreatments are not yet published. Logistics o Are both eyes treated at once? If necessary, and as the patient requests For about 50%, one eye is sufficient o When can I go back to normal activities? Next day o Do I need to take time off of work? If driving or computers require 1-2 days (weekend rest) Benefits o Designed specifically for farsightedness. o FDA proven as an effective vision correction procedure o Excellent safety profile CK does not require cutting or tissue removal. Risks o This is the safest refractive procedure. No infections because the heat spot is self sterilizing. o Fluctuations in vision (only temporary) o Undercorrection (corrected with enhancement) o Overcorrection (rare, may require temporary glasses) o Glare (temporary first month) o Sensitivity to light (temporary during first month_ Off-label o Post-cataract o Astigmatism touch-ups Machinery o Viewpoint CK System Portable Generates radiofrequency waves Common questions o Is it painful? No. Eyes might feel a little “scratchy” o How is CK different than LASIK? None of the lasik risks o Is it an office procedure? Yes o Will I ever need glasses again? Demanding night driving Extended reading The older we are, the more we may need occasional correction. Conclusions- CK may be used to treat blurred vision, without incisions or the removal of corneal tissue. Refracttech.com Intacs (Intracorneal Rings) A small incision is made in the surface of the cornea. 2 microsized tunnels are made in the peripheral cornea. Small curved plastic half-rings are inserted in these tunnels. The result is a flattening effect to the center of the cornea. The size of the intacts are calibrated to the amount of correction needed. Up to 6D internationally (3D in the US) Inserted in 2/3 the depth of the cornea. Bad if the pupil in low illuminations is >7mm, because that is the diameter of the intacts. They are removable without any induced side effects. Can adjust the prescription with age since they are removable. For low to moderate myopes. Can be used alone or in combination o Alone, if simple myopia <3D o With PRK to follow in one month for residual refractive error When sphere is >3D or there is cyl >0.75D. Indications o Any excimer where residual bed <250 Or pach <500, low myopes o Forme Fruste Keratoconus o Frank keratoconus, contact intolerant In keratoconus CL failures to reduce irregular astigmatism, flatten and center the cone to Improve BCVA Improve CL tolerance Avoid corneal transplantation. o Plano presbyopia in a monovision contact o Previously operated corneas with scars of old incisional keratotomy, lasik, etc. o “Flap fear” Pre-op eval o o o o o Simple low spherical myopia <3D Pupils <6.5mm Astigmatism <0.75% Complete the usual lasik pre-op form For keratoconus, if a CL OR is available, it helps select the size of the inserts. Post-op care o Single, 1.2mm radial incision causes a slight FBS for several hours. o Same post-op as lasik Meds qid x1wk Shield at sleep x1wk After keratoconus, can CL fit after 2 weeks. Daily wear for one month. Clear Lens Extraction (CLE) The internal lens of the eye is removed (as in a cataract extraction) and a lens implant of a different power is implanted. Used for patients over 40 with hyperopia. Could also be used for presbyopes. Risks may outweigh the benefits. o Hemorrhage, RD, and endophthalmitis. Patients who may benefit the most from lens extraction are those older than 50 and who have already have some cataract with reduced accommodation. There is a decreased risk for RD once the vitreous is forward. Additionally, some patients may need LASIK after implantation to correct residual refractive error. Phakic Intraocular Lens (PIOL) A lens implant, inside the AC for either myopia or hyperopia. This lens is in effect an internal CL. Types o 3rd Baikoff- A/C 4 point fixation- Chiron o “Nu Vita MB20” o Worst- Fechner- Iris Fixation- Ophthtech o Artisan o Iris Claw Phakic IOL Flexes Can move out of place Not good Endophthalmitis o 5th Feydorov- P/C- Staar “Intraocular Contact Lens- ICL” between the iris and lens can touch the lens, causing cataracts can create papillary block, so perform a PI 1-2 weeks prior to ICL implantation power settings low as possible. Placed at 10 and 2 o’clock 0.8-1.0mm in diameter <90 degrees (3 clock hours) apart Patency verified prior to ICL surgery 1 iridotomy clear after ICL pleacement for myopia or hyperopia advantages Corneal thickness irrelevant Wide range of refractive errors correctable No regression Excellent predictability Preservation of accommodation Small incision- foldable IOL Insertion pearls Minimal viscoelastic Keep cartridge head just inside wound Inject ICL slow and steady Pulsate after 70% injection to unfold Dipple on right leading haptic. Complications IOP >21mmHg (controlled)- 5/46 Glare- 1/46 Pigmentray dispersion- 1/46 Pigmentary Glaucoma- 0 Pupillary block- 0 Decentration- 0 Size adjustments- 0 Cataracts o Mild ASC changes 6/46 eyes o Probably surgery related o All occur in first 2 weeks No changes in BCVA No ICL removal Mean endothelial cell loss 6.1% Touch the lens, get a cataract Intraocular toxicity, endophthalmitis Explant prior to vitreoretinal surgery Decentration Exchange for power adjustment through areas of previous trauma Papillary block/pigmentary glaucoma. Verisyse (AMO) o The FDA approved the first phakic IOL in Sept 2004, the Verisyse. This is a delicate surgery, and it requires a great deal of precision and dexterity by the surgeon. Successfully used in Europe for over 15 years. o It is a PMMA implant that clips onto the mid-peripheral iris (iris fixated). It is manufactured from Perspex CQ-UV PMMA. n = 1.49. The lens has an overall diameter of 8.5mm and is vaulted anteriorly to ensure optical clearance from the anterior lens capsule. The overall height of the lens will not exceed 0.95mm at its highest power. There is both a 5 and 6mm optic zone. 5 mm optic: -5D – 20D, correcting -4.5 to -22D 6mm optic: -5 - -15D o Considerations At least 21 years old -5.00 - -20.00D (0.5D increments) with -2.50D of astigmatism. Stable refraction, in whom satisfactory vision is not achieved with CL or spectacles. Pupil size of 6.0mm of smaller. Patients anterior chamber depth and endothelial cell count will determine whether they are good candidates. A loss of endothelial cells in patients who have undergone the procedure of 1.8% per year. At this rate, a patient will lose 50% of the endothelial cells after 25 years. If too many endothelial cells are lost, the patient will require a corneal transplant. o The “Right” Patient Dissatisfied with quality of vision and functional/ cosmetic limitations with spectacles. Unable to wear CL Progressive corneal problems, inconvenience, and cost. Outside the range of laser refractive surgery, Intacs, CK Risks of refractive lens exchange not acceptable. o The “Wrong” Patient Age- early cataract Inappropriate expectations Expect “perfect” vision Demand immediate results Side effects and complications Unstable personality/ psychological issues Occupational risks (pugilist) The ‘discount’ shopper Astigmatism and enhancements may be an additional fee. Hx of RD, or family history of RD, especially high myopes. Abnormal pupils, irises, shallow AC (<3.2mm) IOP >21 Endothelial cell counts less than 2000 cells/mm2 Age Min. Edothelial Cell Density (cells/mm2) 21-25 3550 26-30 3175 31-35 2825 36-40 2500 41-45 2225 >45 2000 Chronic or recurrent uveitis/iritis, rubeosis irides ARMD, retinopathy o Patient Education Set appropriate expectations Risks Infection, corneal decomposition, iritis, lens dislocation, cataract, edema. High myopia risks- RD Side effects/ cosmesis Halos, glare at night. Lens reflection Physiological changes of aging Presbyopia Cataract Glaucoma o Pre-op Examination Pupil Size o Scotopic pupil size greater than lens optic diameter may cause glare and halos. o Elicit history of meds or other factors that may be influencing pupil size. o Set appropriate post-surgical expectations. Refraction Keratometry Anterior Depth- Biometry Instructions Normal instructions o Procedure Pre-op Meds 20mg Valium Pilocarpine 4% Alphagan-P reduced SCH intraoperatively. Medrol Dose Pack reduces inflammation In Surgical Suite Eye is prepped with providence-iodine solution Topical 2% Lidocaine gel is generously instilled. Paracentesis incisions are performed. An iridectomy is performed Viscoelastic is injected (Healon or CoEase) The insertion incision is made, typically a 6.2mm stepped limbal incision. If the patient has significant astigmatism, the incision is made on the steep axis. The verisyse lens is prepared. The lens is inserted. Sufficient miosis and chamber depth is ensured. The implant is rotated to appropriate position. Enclavation of haptics through paracentesis incisions. The chamber is reformed and checked for leakage, pupil centration is verified, and adequate enclavation is verified. Reposition or reenclavation if necessary. Incision is secured. Viscoelastic is removed. o Post-Op Medication Day Medication Dosage # of times Day of Surgery Diamox 1 capsule At bedtime Week 1 Vigamox 1 drop Qid Nevenac Econopred Week 2 Vigamox 1 drop Bid Nevenac Bid Econopred Tid Week 3 Vigamox 1 drop Qd Nevenac Qd Econopred Bid Week 4 Econopred 1 drop Qd After Surgery to 1 Day Post-op Post-op management is similar to cataract surgery. Larger incision may be prone to leakage for the first 24-48 hours, so check for positive Seidel sign. Appearance o The verisyse lens will be attached (clipped) to the peripheral iris at 2 locations. The orientation of the lens will be based on the entry incision, so the lens will not always be horizontal. The meridian of the entry incision is in the axis of astigmatism as this will help reduce astigmatism when the corneal edema resolves and sutures naturally relax. There will be localized peripheral corneal edema in the location of the entry incision and the paracentesis, which resolves over 1-2 weeks typically. There may be SCH as well. There will be some degree of cells and flare in the AC which resolves over a 2-4 week period. Sometimes the pupil may appear slightly oval which will normalize after a few weeks (there is no adverse visual effects, just a slit lamp finding). Testing o Uncorrected VA, IOP, fluorescein staining to verify Seidel negative, SLE. There may be some retained viscoelastic which can cause a temporary elevated IOP. o An IOP between 21 and 29 does not require intervention, while IOP of 30 or more does require a glaucoma drop for 1 week as retained viscoelastic is naturally cleared. o Patient should be cautioned against bumping, rubbing, or touching the eye for 1 week. o An eye shield should be applied and should be used for sleeping for at least 1 week. o Pain medications can be prescribed as necessary in addition to post-op medication. o Patients unfamiliar with LASIK should be instructed on the intraocular lens recovery process, which may include more discomfort, longer healing time, and slower visual recovery. 1 week post-op Appearance o Corneal edema will be resolving along with cells and flare in the AC. o Patients should notice significant improvement in UCVA. Check for quiet eye, deep AC. Well centered lens should be apparent. o UCVA (D/N), MR, BSCVA, IOP, SLE, Check Meds 4-6 week post-op Appearance o Quiet eye with deep AC and well centered lens. BCVA should be as good or better than pre-op refraction. o If UCVA is poor, determine the cause (inflammation, astigmatism, retinal/macular problems). o If the problem is lens centration or power, consider lens repositioning or replacement. o If poor vision is related to existing or induced astigmatism reassure the patient and consider enhancement surgery at the 3 month visit. o UCVA (D/N), MR, BSCVA (D/N), IOP, SLE, Corneal topo 3 mo post-op Appearance o Vision will stabilize between 1-3 months. Corneal edema and AC cells will be resolved by the 1 month visit in almost all patients. Sutures may become loose at various times and may cause FBS. Fluorescein testing will reveal the elevated suture with fluorescein pooling around the suture. This is an indication for suture removal which can be performed at the slit lamp. If there are no symptoms and sutures are flat, suture can remain in place. Testing o MR may be performed at any time. If patient is having difficulty with vision during healing period, glasses may be prescribed. In some cases, it is expected that glasses or CL will be needed post-op. IOP should be checked at each visit along with slit lamp evaluation. In some cases, LASIK after 6 mo may be an option for residual refractive error is that is desired by the patient. o In addition to seeing you for a 3 month visit, patient should also be seen at the surgery center for endothelial cell count. o Check for secure well-centered lens. o VA should be good or better than pre-op BCVA. If not, consider an enhancement if refraction has stabilized. o UCVA (D/N), MR, BSCVA (D/N), IOP, SLE, Corneal topo, endothelial cell count o o o o o 1 year Punctal plugs (silicone or collagen) should be used liberally which can aid in comfort and lubrication after surgery. Follow patient carefully until vision has stabilized and they are satisfied with VA. UCVA (D/N), MR, BSCVA (D/N), IOP, SLE, DFE Considerations If a patient has eye trauma at any time, the eye should be evaluated for lens disinsertion. If the lens is ever found to not be attached to the iris, it will need to be surgically reattached as soon as possible to avoid trauma to the endothelium from an unstable lens. After the 12 month visit, patients should be evaluated annually. Enhancements Remove sutures and evaluate vision and patient satisfaction. Allow refraction and topography to stabilize. If patient is happy, do nothing and continue to follow up. If patient is not functional or patent is not happy, consider the following based on lifestyle, occupation, and level of refractive error. 3-6 months post-op Residual myopia o Corneal laser refractive surgery Residual hyperopia o Corneal laser refractive surgery Existing or induced astigmatism o LRI or corneal laser refractive surgery. Advantages Contrast sensitivity is preserved and often improved. Rate of retinal detachment was not increased Preservation of the crystalline lens allowed for continued accommodation. Patient Screening Thorough clinical work-up. See visian. Complications Study 1 1.36% had the IOL exchanged due to adequate surgical fixation, improper optic size vs. pupil size or power calculation error. 1.51% had the IOL removed due to inflammation, patient enxiety, optic zone that was too small, postoperative trauma or surgical trauma. 0.60% had to have the IOL reattached. 0.45% required retinal repair. 0.15% experienced surgical trauma that required retinal repair. Study 2 Adverse events o IOL Replacement 0.7% o Repositioning of the lens 0.3% o Removal and cataract implant- 0.3% o Secondary glaucoma- 0.7% Average Cell loss declines over time and levels off to <1% per year. This is related to the individual surgical technique. o Budo et al n = 518 7.0% at 3 years o Landesz et al n = 67 10.9% at 3 years o Phase III n = 536 3.1% at 2 years Complications o Iris atrophy 0.2% o Iris pigment precipitates 0.8% o Non pigment precipitates 1.6% o Lens not centered 1.6% o Mild corneal edema 0.4% o Glare/halos- rings 18.5% o Macular degeneration 0.4% o Incipient cataract formation 3.0% o Diplopia 0.2% o Increased IOP requiring treatment 0.2% Iris Defect Elevated IOP This happens in a few cases. After treatment, it generally reverts to normal values. In 2 cases, Urrets-Zavalia syndrome developed, which can be caused by incomplete removal of visco-elastic. Other causes include o Use of a visco-elastic with an extremely high viscosity. o No iridectomy or iridotomy o Secondary glaucoma Flat AC and Non-Sealed Wound Closure Inadequate closure of the tunnel can lead to an incomplete seal. Without immediate and adequate treatment, corneal edema can arise. Decentered Lens- 1.5% The lens is not optimally centered. This does not have any effect on endothelial cell loss. Dislocated Enclavation Trauma or insufficient iris tissue in haptic. Cataract (unlikely) Iris Atrophy Endophthalmitis Visian ICL o Implanted collamer lens o Preferred refractive alternative Moderate to high myopia Thin corneas Flat corneas Large pupils Fear of failed outcome (permanent procedure) Dry eye patients Patients who want the best vision o Off label Use Keratoconus History of previous ocular surgery Patients under age 21 older than 45 Collagen sensitivity (none reported) o Safer refractive Alternative Inserted through a small self sealing incision No suture required No induced astigmatism. Much faster recovery No contact with moving intraocular structures Avoids potential damage to iris Affords safer removal in future Invisible to the patient and observers Less incidence dysphotopsia due to edge glare. Collamer material is more biocompatible. Thin, flexible, stored in solution Location in the posterior chamber. Resting position far from corneal endothelium o Advantages Maintains normal cornea curvature. No oblate corneal flattening. No tissue removal No regression No induced nighttime distortions (HOAs) o o o o No exacerbation of dry eye cymptoms Results are immediate. Faster than LASIK, because there is no corneal edema. Inserted through a tiny clear cornea microincision that requires no stitches. Lens material is proven safe and nonreactive in the eye. High level of predictability Uncorrected VA better than 20/20 and/or better than with glasses or CLs occurs in more than half of patients. Optical diameter of the ICL is quite large which means effective optical zone at the corneal plane is typically larger that with laser vision correction. The ICL will not scar inside the eye, therefore it is easily removable/ reversible. Better optical quality of vision since it is closer to the nodal point of the eye. Dry eye and halos are not an issue like as in LASIK. Contraindications Glaucoma, including pseudoexfoliation and PDS Cataracts Retinal disease Keratoconus and related corneal conditions Anatomic narrow angle or shallow AC Previous ocular surgery or serious ocular traumas Poor systemic health Pregnant or nursing. Material/ Specifications Collamer 0.3% porcine collagen + HEMA copolymer Current design (V4) is 5th generation Foldable and injected through a 3.0mm incision Footplates rest in ciliary sulcus Four overall lengths ICM 12.1 – 13.7mm ICM central thickness 50 microns Refractive index 1.453 at 35º C UV filter FDA Study Safety and Efficacy Data Acute IOP Rise in 20/526 (3.8%) Majority of cases reported during first 1-2 days post-op. no reports after 21 days post-op. 17 eyes- additional YAG iridotomy or enlargement of existing iridotomy. 3 eyes- AC irrigation for removal of retained viscoelastic. Surgical iridotomy largely avoids this issue. Clinically significant Anterior- Subcapsular Opacities in 2/526 (0.4%) 2 cases progressed to clinically significant opacity required cataract extraction. 1 case inadvertent use of preserved miotic agent (topical Carbachol) in intraocular irrigating solution. BSCVA 20/20 pre-op and post-cataract extraction. 1 case opacity observed 6 months post-op. cataract surgery performed at 16 months. BSCVA 20/40 pre-op and postcataract extraction. o Evolution of the ICL STAAR Surgical Company 5th generation lens over more than 10 years worldwide. Over 75,000 implants performed Procedure based on cataract surgery platform Wide treatment range -3.00 to -15.00 sphere (up to 2.5D cyl) Up to -20.00 for the reduction of myopia. Can do larger, off label. Toric coming soon. 4 sizes available to best fit individual eyes. Stored in a sterile solution, just like soft CLs. o Protocols Screening process Myopic range: -5.00 to -15.00D Less than or equal to 2.5D refracted cylinder Normal anatomy: slit lamp exam, gonioscopy, IOP, retinoscopy Best Candidates 21-50yo Stable refraction (<0.5D change for 1 year preceding implantation) -3.00 - -17.00D Up to 2.50D of refractive astigmatism. Can correct even more cyl with LVC enhancement. Thin corneas by orbscan/pach. Even with keratoconus. Proposed result of LASIK or PRK would leave the cornea “too flat.” Preoperative Visit 1-2 weeks prior to surgery Required measurements o VA o Accurate refraction (manifest and cyclo) Back vertex distance assumed 12.0mm. o Keratometry with axis o SLE dilated and undilated. o IOP o ACD Using Pentacam- direct optical measurement. Need 3.0mm Pachs Gonio Central 1.5mm K Horizontal W-W Endothelial cell count Laser peripheral iridotomies Provide outlet for aqueous flow around the ICL to prevent pupillary block. Facilitates removal of viscoelastic at surgery. 1-2 weeks prior to procedure to decrease inflammation, etc. This procedure can hurt! o PF qid x1 week o Rx for Vigamox/Zymar starting 1 day prior o Consents signed. Interim Essentials Refractive stability visits in your office o Dry refraction o Cycloplegic refraction o Manual keratometry o Back vertex distance (12mm = default) o Surgical Procedure o o o o o o Done in a surgical center under “twilight” A driver is required and should anticipate total time at the center of 1½ hours. Valium 10mg-20mg 30 min prior to surgery. IV heplock or Vered for additional relaxation/sedation. Pupil is widely dilated. Conscious S/R Nurse monitor LRIs for cyl The ICL lens is inserted through a 3mm incision that seals up by itself. A viscous gel is used during the procedure to protect internal structures of the eye. 15 min Virtually painless Immediate results Surgery for fellow eye ideally 2 weeks after initial eye. Bilateral procedures now being performed. Loading the Visian ICL Insert cartridge into injector. Lock into place. Clear corneal incision Temporal, clear corneal incision orients best to iris place. o Post-Op Care 2-4 hours post-surgery Ensure IOP not elevated. Over 25mmHg must be addressed. IOP elevation o Retained viscoelastic- burp and check. o Non-patent iridotomy- back to the laser. SLE o ICL centration o Inflammation o Vault-generally less at this time than will be seen in longer-term follow-up care (less than 1/2x corneal thickness not uncommon) VA Post-Op Day 1, 7 and Beyond VA Refraction (Day 7 and beyond) SLE o ICL Centration, Inflammation, Vault 0.5-2x corneal thickness. IOP Evaluation of crystalline lens Assessing the Vault o Thin optic section with biomicroscope Angle between ocular and light source should be 30-45º Use bright illumination o Alternate focus from corneal thickness (ct) to vault space for comparison. o Under 0.5ct observe for capsular haze. o Over 2.0ct observe fro narrowing angle. Medications Vigamox/Zymar qid Nevenac/Acular LS qid until finished PF qid for 1 month with quick taper. Copsopt for 3 days ATs Biomicroscopy examination and IOP check 1 day, 1 week, 1 month. Along with Vas, Ks, MR ICL Vault o SL beam from lens to crystalline lens. o K = 100% o 50% and up is good. Enhancing laser vision correction procedure can be done 1 month after surgery if needed. o Patient Satisfaction Only procedure that consistently produces UCVA significantly better than BCVA pre-op. Patients routinely comment on this. This is since the nodal point is within the eye, which is the best optical location. Corneal surgery, contacts, and glasses are relatively far from the nodal point. When you bring up to patients, surprising how many patients are comfortable with concept of ICL compared to LASIK. There is less fear. It is viewed as “no maintenance contacts.” Procedures and Protocol Meeting patients expectations o Clearly understand the patient’s goals and limitations o Define the reasonable outcomes and limitations of a procedure o Success = matching goals with reasonable outcomes. Who is a candidate? o Age 18 and older (prefer >30) o Stable refractive status, 0.50D or more change over 12 months and we’re in a holding pattern. l o Myopes are more stable and therefore have a better outcome. Up to -14.00DS with 6D cyl. o o o o o o o +6D and up to 6D cyl Has realistic expectations. Never, “Never want to wear glasses.” Desires good “functional vision CL intolerant Wants less dependency on glasses/CL Not an engineer Good ocular health: no visually significant lens opacity and healthy macula. o Corneal Thickness >470 microns (depending on refractive error) Preserve minimally 150 microns in stromal bed. Average 15 microns per D with 6.5 OZ blended to 9mm. As OZ increases, the amount of tissue removed increases exponentially. o Keratometric Ranges Myopes 35.00D flattest K reading Uses 75% of power to determine change in K. Hyperopes 49.00D steepest K Uses 100% of power to determine change in K. i.e., 45D with +4 → 49D Bad Candidates o Contraindications Active autoimmune disease- Graves, Lupus, RA, MS CA (immunosupressed) Uncontrolled HTN, vascular disease. Uncontrolled DM Type 1- one eye at a time, due to poor healing Type II- OK as long as no DR Keloid former Pregnancy or lactating mothers- cornea swells during lactation so will cause under-correction, pre and post-op meds will be passed to the fetus. (Preg abs) Wait 3 months post lactation Rosacea Pacemaker Active HSV Keratitis, HZO (abs) Caution in patients with a history of this. Should be no activity in 2 years. Treat with oral antivirals and viroptic pre and post-op. No PRK. HIV Active ocular disease- iritis, conjunctivitis, corneal problems (ulcers, scarring, erosions) abs Glaucoma with VF defect or NFL defect (abs) Cornea ectasia (Relative: Form fruste keratoconus; Absolute: Clinical Keratoconus, pellucid) Exposure keratopathy- lagophthalmos, prior blepharoplasty, thyroid orbitopathy Steep corneas Thin corneas- creates keratoconus Dry eyes Meibomitis Lenticular astigmatism ARMD Large pupils- increased aberrations RD RP or other retinal diseases Previous eye surgeries Amblyopia Monocular patients (abs) Ocular allergies Neo, pannus Cataracts Corneal distortion due to CL wear ABMD Endothelial dystrophies <1500mm2 (Fuchs) Progressive myopes. Small orbits (rel) Patients that are pregnant, want to become pregnant, or currently breast feeding. Autoimmune disease (Do PRK, one eye at a time) o Medications Allergies to medications Hormone replacement supplement *Prempro steepens corneal curvature Blood thinners Coumadin (hemorrhages) Antihistamines Claritin, Zyrtec (alter lacrimation, blurred vision, hemorrhages) Antidepressants Zoloft, Paxil (abnormal lacrimation, blurred vision, abnormal accommodation, conjunctivitis) Anti-acne *Accutane (abnormal lacrimation Anti-HTN Norvasc, Zestril, Atenolol (abnormal vision, dry eyes) Lipid lowering agents Lipitor (amblyopia, dry eyes, refraction disorder, hemorrhages, glaucoma) Antiinflammatories Celebrex, Prednisone (blurred vision, conjunctivitis, glaucoma) Hypnotics *Ambien (Abnormal vision, scleritis, corneal ulceration, abnormal lacrimation) Anti-seizures Neurontin (dry eye, conjunctivitis) Migraine treatment *Imitrex (long term ocular side effects) Antiarrhythmic agents *Cordarone (corneal degenerations, corneal microcysts, macular degeneration, dry eyes, optic neuritis) Which Procedure? Pre-op Expectations o Good functional vision 98% see 20/40 or better uncorrected 75% see 20/20 or better uncorrected 15% may need an enhancement the greater the correction, the more likely 0.2% complication rate o Manage these. Why? To avoid unhappy patients To avoid enhancements Increase word of mouth referrals. o Create realistic expectations Surgical outcomes have tolerances. Vision continues to change and stabilize for 6-12 months after surgery. Vision (refractive error) continues to change throughout life. Glasses or contact lenses may be needed after surgery to augment vision. The decision to enhance must be conservative. Presenting Refractive Surgery You need to list it as a treatment option. You must include a lifestyle assessment. Every candidate must have a current PCE What not to say o “Burn the cornea with a laser” o “Slice the cornea with a blade” o “Patient is over-corrected” o “Patient is under-corrected” Risks Infection- 1/5000 Night glare- 2-5% o Eliminated with wavefront Symptomatic aberrations- 1/500 Regression- 5-15% Need touchup Overcorrection- 5% Blindness- 1/1 million Pre-Op Patient medical history for any contraindications o Autoimmune disease, rheumatoid/collagen vascular diseases, cancer, uncontrolled hypertension, uncontrolled diabetes, keloid former, pregnancy, glaucoma, keratoconus, retinal disease, prior disease, infectious diseases such as HIV and hepatitis, pacemakers. Psychological problems. Past ocular history o Previous eye surgeries, corneal ulcers, erosions, keratoconus, or other dystrophies, ocular herpes, glaucoma, cataracts, iritis, dry eyes, amblyopia, diplopia, retinal tears or detachments, or DR. CL History o What type of CL? o If contemplating MV with LASIK, has your patient been a successful wearer of monovision CLs? o If no prior experience with monovision, we strongly recommend a CL trial or a “test drive” before committing to a surgical last procedure. o Contacts removed until stable refraction. CL wearers must be weaned off their lenses SCL wearers need 2-4 weeks of no wear with stable refractions. Min: 1 week RGP wearers need 4-20 weeks off RGPs with stable refractions. 5 weeks off for every decade of wear. Medications o Amiodarone, accutane, imitrex, and any anti-depressants or neurontin. Allergies o To any meds, especially antibiotics. If hayfever, are they using any antihistamines? Note that these are repeated days-weeks apart. Ortho K can take 8 months Complete all pre-op forms. UCVA, BCVA, Spectacle Rx Comprehensive eye exam with manifest and cycloplegic o Perhaps serial refractions, including one cycloplegic. This is especially important in contact lens wearers and in patients who have tear film issues, accommodative issues, or any other ocular conditions that may cause refraction to fluctuate. Repeatable topography, keratometry, and SRx measurements (usually 3 measurements) over a 2-4 week span are a safe bet. Verify that the Rx is in range for the procedure. Peripheral retinal exam with BIO. Any holes, tears, or questionable lattice should be referred to a retinal specialist for an opinion before laser vision correction procedures. If monovision is an option for the patient, you have to mock that up prior to surgery to make sure the adaptation is possible. o Dominant eye must be determined. o Over-glasses may be necessary to balance special tasks Not a cure. It is a modification to increase function. 90% of activities can be done. Lasts about 5 years until a new Srx is needed. Residual Rx: What would you like to target? And for which eyes? Pachymetry o Need 150 microns for the flap o 250-300 microns must be left for the corneal bed o This leaves us with 100 microns to “vaporize” o About 12-14 microns of cornea is removed for each diopter of refractive change. o Beware of pachs <500. Topography o Tells you the anterior corneal surface is too flat, steep, irregular, or abnormal. Poor outcomes can result from abnormalities, which include keratoconus, forme fruste keratoconus, pellucid marginal degeneration, displaced apex syndrome, and CL-induced corneal warpage. Slit Lamp Evaluation o Note any abnormalities in the conjunctiva, lids, and tear film. Normal lid fissures, brow prominence, lid relaxation, deep set eyes. Any unusual vessels in the conjunctiva? o Corneal evaluation Epithelial or stromal scarring, endothelial defects, corneal thinning, ABMD, or vascularization. Pannus ABMD o Lens- cataracts (nuclear sclerosis can lead to lenticular myopia or other cataract changes). Posterior ocular tissue health assessment o Disk anatomy, ARMD, vascular changes, or peripheral retinal thinning or holes. Comment on sunglasses post-DFE/ IOP Tear evaluation o Schirmer’s test, TBUT, and fluorescein corneal staining. Pupil Size in Darkness- predicts the risk of post-op nighttime glare and haloes. o Document anisocoria. Wavefront Aberrometry Show the patient the informed consent video and have them answer the “quiz” and sign the informed consent form. o A thorough review of the actual surgical procedure, the possible benefits, risks and complications, the recovery process, and patients’ expectations and responsibilities. Discuss the fees and that it includes all aspects of care once they arrive at the center through their 1-year follow-up period in your office and any needed enhancement procedure. Prescription for Vigamox 1gt OU qid beginning 1 day prior to surgery and 5-7 days post-op. Patient can also increase the omega-3 intake (minimum 4000 units/day) Recommend AT 1gt OU qid 5-7 days pre-op (Bion Tears or Thera Tears preferred.) Also: restasis, punctal plugs, lid hygiene, EES ung, doxycycline Give the patient pre-op, post-op, and pre-surgical packet Schedule the surgery date and 1-day post-op before the patient leaves. Comments Section o Comment on realistic expectations Reduce dependence on corrective lenses Understands they will need reading glasses (eventually) o Recommendations Intralase vs. hansatome Custom vs. wavefront vs. traditionally VISX vs. Allegretto Surgery Procedure Excimer laser is calibrated and programmed for the specific refractive treatment and tested. Instillation of anesthesia and antibiotics. Position patient on the table. Clean the eyelashes and fornices. Drape the eye and insert a lid speculum. Center the patient’s eye in the operating field and make alignment markings. Create the flap and lifts it. Swab the underneath stroma. Excimer laser ablates the stroma. Swab and rehydrate. Reposition the flap, irrigating it to remove debris. Check the alignment. Smooth the flap with a microsurgical sponge. Instill lubricant, antibiotics, and anti-inflammatory drops. Remove the eyelid speculum. Check the flap. Fees Usually enhancements are covered for 1 year. After that, a fee is charged. Post-Op To ensure proper healing as well as monitor outcome progression, patients are seen (a minimum of) o 1 day, 3 days (PRK), 1 week, 1 month, 3 months, 6 months, 1 year. o Then yearly after that. Be enthusiastic and encouraging! Uncorrected Vas o Distance and near o OU acuity first. Start with the large letters and work your way down. Reassure the patient that they are doing great. Refraction Topography Slit lamp o Normal: SCH, dryness, micro or pseudostriae, meibomian secretions and small FBs, epi ingrowth. Fluoroscein TBUT and tear prism. Flap edge evaluation Refer the patient back immediately for significant straie, dislocated cap, or severe pain. Minimal interface debris is not of concern. Consult with surgeon on DLK for increased steroid dosing. IOP Meds/Instructions Refer the patient back to the surgeon immediately for significant striae, dislocated cap, or severe pain. Consult with the surgeon on DLK for increased steroid dosing. Minimal interface debris is not of concern. Schedule the next appointment. Fax post-op forms to the surgeon. If in doubt, don’t hesitate to call and speak to surgeon. Post-Op Concerns Flap Complications o Folds in the Flap This is the most common. o Dislocation of the Flap o Button-Hole Cut Microkeratome slips and tissue is ripped out of the flap. This means that LASIK cannot be performed. Probably continue with ASA after healing. o Scars from Flap Cuts o Flap was handled and not smoothed. o Flap Dislocation/ Wrinkling Due to problems with repositioning of the flap at end of procedure o Post-op displacement o Deposits in the Interface Causes Nonorganic materials Metal from microkeratome/blade or instruments Particles from the sponge Talc from the gloves Lint from drapes/gauze Dust Organic Materials Endothelial Cells Tear Film Debris These can be left in the cornea. No harm will be done. Treatment o Interface debris rarely interferes with functional recovery, however, if optic quality of the cornea is compromised, then the debris must be removed (flap lifted, debris removed, flap replaced) Epithelial Complications o May occur pre-op Due to Excessive anesthetic Abrasions o May occur during surgery Due to Dry cornea Blade, forceps, or spatula problems Movement of the eye as the speculum is removed Improper sponge use. o Early Sands of Sahara (Diffuse Interlamellar Keratitis) Etiologies o Varied and not entirely understood o Seems to be linked to contaminants in the lamellar interface introduced at the time of the surgery. o An autoimmune response Occurs from day 1 Stromal meltdown by day 5. Signs and Symptoms o Typically noted 2-5 days post-op Patient notices progressive decrease in VA Slit lamp examination reveals diffuse white granular cell infiltrates across the interface. o The next stage shows a granular haze centrally (in the center of the flap). It is a thick white. Refractive status is slightly hyperopic. o Late Otherwise asymptomatic o The next stage results in a dense central infiltrate (dense, white clumped cells)] Decreased Vas Flap may have straie Hyeropic astigmatism is measured. o The end result (if not diagnosed and treated) is stromal melting, permanent scarring, and vision loss. Management/Treatment o Immediate and aggressive treatment must occur before the final stage. o Stage 1 and 2 Steroid drops every hour and ointment at night. 24 hour monitoring Must resolve with this. o Stage 3 Lifting the flap and careful irrigation to remove the inflammatory reaction and steroid treatment over time. Ingrowth Etiology o Poor flap edge adhesion or alignment Buttonhole flap Free cap Epithelial cells left under flap Results in o Reduced VA o Irregular astigmatism o Discomfort o Risk of stromal melting o Debris Sands Ingrowth Over-response (Leaving +) Under-response (Leaving -) Other staining, Flap Distortion Discomfort IOP ** It is extremely important that you carefully follow these instructions and any additional ones that Dr. Dodge has recommended prior to surgery. Pre-Op It is extremely important to follow Dr. Dodge’s instructions regarding when to stop wearing your contact lenses. This is critical to the success of your procedure. o Soft lenses a minimum of 72 hours prior to the procedure. o Soft toric lenses one week prior to the procedure. o RGP (hard lenses) a minimum of 2 weeks prior to the procedure. Let Dr. Dodge know if you are pregnant, nursing, or if you form keloid scars. Let Dr. Dodge know if you are on Accutane or Cordarone. Starting 3 days prior to your procedure, begin eyelid scrubs every evening. (Do not do this after surgery.) Place one drop of baby shampoo on a wet, warm washcloth. With your eyes closed, gently massage your eyelashes with the washcloth for about one minute, and then follow with a thorough rinse of the lids with water before opening your eyes. Make sure that this is done the night before surgery so that the eyelids are free of make-up. Wash your face with soap and water in the morning. You will be given a prescription for an antibiotic eye drop, either Zymar or Vigamox that can be filled at the pharmacy of your choice. Start using the drop four times daily in the operative eye one day prior to your procedure. By the time you arrive at the surgery center, you should have used the drop four times (i.e., if your procedure is scheduled for 5pm on Thursday, you should start using the drops on Wednesday at dinnertime, again at bedtime, and then at breakfast and lunch on Thursday). Do not wear any eye or face make-up, cologne, lotion, or powder on the day of your procedure. You will be asked to remove large earrings necklaces, or chains. The area around your eyelids will be cleansed just prior to the procedure. Wear warm, comfortable clothing the day of your procedure. The temperature is kept very cool in the laser suite. You might want to bring a sweatshirt or sweater. Please arrive at the surgery center on time. You will need to arrange for transportation on the day of your procedure and for your one-day post-op appointment. You will not be allowed to drive yourself home. Please bring your prescribed eyedrops with you on the day of surgery. Financial Arrangements Please have all financial matters completed prior to surgery. Payment for surgery will be requested when you check in for surgery. We accept cash, cashier’s checks, personal checks, Visa, Mastercard, Discover, and American Express. Financing is available. o Generally the application must be filled out and submitted 48-72 hours prior to the surgery date. o Once you have received an approval, please contact our office confirming that you are financing and received an approval. This way we may ensure that we have all the necessary forms in order prior to your treatment. If possible, please contact us within 48 hours. o We will need to make a photocopy of your driver license to submit to CareCredit. Please bring it with you the day of surgery. If you have a co- borrower or if someone is financing the surgery other than yourself, they must be present the day of surgery to sign the form. If this is not possible, they may make arrangements with our office to come in prior to sign the forms. We must also obtain a copy of their driver license to submit to CareCredit. Change in Planned Schedule/ Questions If you have any questions concerning your pre-operative or post-operative instructions, please do not hesitate to call Dr. Dodge. In the event that you need to reschedule, please notify us immediately. A $250 cancellation fee will be charged if you fail to advise us of your cancellation. LASIK Patient Information Your surgery will be performed on ___________________. Check in time is ______. Pre-surgical Instructions There are no restrictions on eating or drinking before your procedure. Please do not consume any alcoholic beverages on the day of surgery. Also refrain from consuming beverages containing excessive amounts of caffeine. If you are normally a coffee drinker, feel free to consume your usual amount. Continue to take your usual medications unless otherwise instructed. Follow your Dr. Dodge’s recommendations regarding the removal of your contact lenses prior to your procedure date. If you would like family or friends to watch your procedure, they may do so from the observation area. The total time spent in the laser facility will be about 1½ - 2 hours. What to Expect on the Day of your Procedure You will be asked to read and sign a consent form, listen to an audiotape, and watch a video. Should you have any questions or concerns, you will have the opportunity to discuss them with the surgeon prior to your procedure. You will be offered a mild sedative to help you relax. Please let the staff and surgeon know if you have allergies to any medications. You will not be asked to change your clothing, however you may be asked to remove large earrings. A scrub will be performed to cleanse your lids and eye area. Please do not wear any make-up to the surgery center. Several eye drops will be used to prepare your eye for the procedure. It is very rare to react adversely to any of these drops, but please tell us if you have ever had a reaction to any eye medications in the past. Your cooperation during the procedure is essential. If you are excessively sedated, it will be more difficult for you to focus on the target light. You must be alert and respond to instructions. When you enter the laser suite: An assistant will help you into a chair that will be slowly reclined until you are flat on your back. Anaesthetic drops will be administered and the eye not being treated will be covered with a shield. After you are positioned under the laser, you will notice a blinking red light in the center of a white ring. This is the light you will need to fixate on throughout the procedure. The surgeon will keep your eye entered if you move slightly, but try to remain as still as possible. An instrument will be placed around the eyelids that will prevent you from blinking. The surgeon will make temporary marks on the surface of the eye that are used when repositioning the flap. Next, a ring will be placed on the eye to stabilize it. You will hear the sound of the vacuum as the ring is secured and your vision will temporarily fade away. Do not be alarmed. The surgeon has complete control of your eye and your vision will return in just a few moments. You will hear the sound of the microkeratome as the surgeon creates the corneal flap. After just a few seconds, the microkeratome will be removed and the suction on the eye reduced. The surgeon will gently fold back the corneal flap. You will hear the sound of the laser as it prepares to treat the eye and you will be instructed to stare at the blinking red light or in the center of the white ring. The laser will make a clicking of snapping sound as it painlessly reshapes the cornea. The excimer laser can be stopped and started precisely within a fraction of a second. If your eye moves, the laser will be stopped. Fixation will then be reestablished and the procedure completed. You may become aware of an unpleasant odor during your treatment. This is the smell of a vapor created by the laser. A vacuum tube will be placed near your eye to minimize the scent. After the laser treatment is complete, the ring will be removed from your eye and the surgeon will carefully reposition the flap. After the corneal flap has settled into position, the surgeon will remove the instrument retaining your eyelids and post-op drops will be administered. You will be helped out of the chair and the surgeon will recheck your eyes before you leave the center. When you check out at the front desk, your post-op instructions will be briefly reviewed and you will be asked to put on eye protection for your trip home. Common Symptoms you may Experience About 30-90 minutes following your procedure, you may experience some discomfort (burning, stinging, and tearing) as the anaesthetic drops begin to wear off. The symptoms may be severe. Please take the medication provided or an over-the-counter pain reliever to reduce discomfort. Other temporary symptoms may include: light sensitivity, watery eyes, runny nose, gritty, foreign body sensation, eye irritation, and eye redness. Frequent use of lubricating drops will help with these minor irritations. Cool compresses may be applied to the eyelids to relieve swelling or sensitivity. Avoid getting water in the eye(s). Vision will usually appear particularly blurry for 4-6 hours, and then begin to improve. For the first few months you may notice visual fluctuations, particularly when driving and using the computer. Glare and halos around lights at night and in low light conditions are normal and will gradually subside over 3-12 months. Your eyes may feel dry for months. Use artifical tears to alleviate this. You may notice red spots in the whites of your eyes. These will disappear with time. Upon Arrival Home: Take it easy for 4 hours. The medications will make you tired. You may resume your normal diet. Keep your eyes closed for at least 3-4 hours except to eat or use the restroom. Activties Allowed: No swimming, hot tubs, or whirlpools for 7 days. Showers and baths are fine, but keep your eyes closed to avoid getting water or shampoo in them. Wait to take a shower until after you have been seen for your first post-op visit. When you take a shower, you may wash your hair and face. Keep your eyes closed while the water is on your face. When drying your eyelids, gently dab them without applying any pressure on the eyes. Do not sleep with your pets in your bed for the first 24 hours after the surgery. Laundered bed linens should be placed on your bed. Avoid a dusty/dirty environment for one week. It is preferable that you do not smoke since it will irritate your eyes. Keep the operative eye(s) closed as much as possible for the first 6-12 hours following your procedure. This will speed healing of the ocular surface and restore your vision faster. Watching television and reading is permitted. Do not drive until you have been authorized to do so by Dr. Dodge. It is best to wait for at least 1-3 days before returning to work to allow your ocular surface tissue to completely heal. You may return to your normal exercise routine after 3 days and once you feel comfortable. However, do not return to high-impact sports, such as boxing, until authorized by Dr. Dodge. Although that it is always recommended that you wear protective eyewear for racquetball and contact sports, you must wear eye protection for these types of activities for 6 months. Wear ultraviolet sunglasses when outdoors. If in doubt about activities you can or cannot do, please call our staff/ Your Recovery: Your vision will be somewhat blurry for 6-12 hours following your procedure. If you choose to have only one eye treated at a time, you may feel a little offbalance after your first eye is treated. Your depth perception may be a little off as well. Be careful performing tasks such as pouring hot coffee, hammering a nail, or driving. It is important to remember that your distance vision will clear first and your reading vision last, unless you are over the age of 40. In patients over 40, reading glasses are usually needed to read small print unless correction for monovision was done. Night glare is also more apparent during the first couple weeks of your recovery. Star-bursting and halos around lights usually occur in patients with more severe degrees of myopia and large pupils. Night glare usually resolves or returns to the pre-procedural level once both eyes have healed. Infection is a possibility, although the risk is minimal if post-operative medications are taken and instructions followed. Symptoms of infection may include increased pain, redness, blurred vision, and discharge. Do not hesitate to contact Dr. Dodge if you feel your eye is not healing correctly. Follow-up Care After your Laser Procedure First Week o Dr. Dodge will give you a schedule for your follow-up appointments. The purpose of these initial follow-ups is to ensure normal healing of your corneal surface and to detect any evidence of infection. First Three Months o Less frequent follow-up appointments will be scheduled to ensure proper healing, to measure visual progress, and to check eye pressure. Eyecare and Medications Do nto rub the eyes for at least 6 months following your surgery. If your eyes itch, notify Dr. Dodge during the post-operative period visit and a medication will be prescribed. Wear the eye shields provided at bedtime (or when lying down) for 1 week. If you sleep on your stomach you will need to wear the goggles for 4 weeks. The shields should rest against the bones of the brow and cheek and not the eyelids. Do not wear eye make-up for 3 days. When resuming the weasring of eye cosmetics (mascara, eyeliner) please purchase new products and discard the old cosmetics used prior to surgery. Whem removing eye make-up in the first 6 months after surgery, do so without placing pressure on the eye. If you need further instruction, please ask a member of the staff. You will receive a post-op bag the day of surgery that will include the following items: Sunglasses, shields, tear samples, and steroid drops. Artificial tears: instill one drop in the treated eye(s) 4 or more times a day or as needed. Prescription eye drops: begin using 1 drop of Zymar and one drop of PF 3 times a day for 4 days in the treated eye(s), or as instructed by Dr. Dodge. A prescription for Zymar will be given to you prior to surgery. Please have the prescription filled at your pharmacy prior to surgery. Please bring the bottle of eye drops with you to the office the day of your surgery. Medications Needed After Your Procedure Zymar/ Vigamox o Dose: One drop, four times a day o Purpose: Infection prevention. Allergic reactions rarely develop. Symptoms include increased redness, itchiness, and swelling. Lotemax o Dose: One drop, four times a day o Purpose: Initially to reduce redness, swelling, and light sensitivity. Promotes normal healing. When Putting in Eye Drops Do not use anything in the treated eye(s) except the above medications, unless otherwise directed. Wash your hands before putting in the drops. Shake all bottles before each use. Pull down your lower lid and place the drop in the pocket of the eyelid, holding the bottle top away from the eye. Wait 1-2 minutes between each drop. The order that the drops are put in does not matter. You may experience a medicinal taste in the back of your throat after putting in drops. This is normal. To avoid contamination of the eye drops, do not touch the tip of the bottle to the eye. Use drops at breakfast, lunch, dinner, and bedtime. Wait at least one minute between drops. Do not stop or change the frequency of any medication unless specifically instructed to do so by Dr. Dodge. Failure top follow directions may influence the outcome of your surgery. Misuse may result in damage to the cornea or a change in your refractive condition. PRK/LASEK Post-Op Regimen Post-op 1, 3-5, 10 day, then every 3-4 weeks to monitor healing/ IOP BSCTL until epithelium closed (usually day 3-5). If falls out day 1-3, the doctor, not the patient should replace it. Zymar 4x/day until epithelium heals PF 4x/day until epithelium heals, then 2x day for 3 months. Increase if regression/ haze, decrease if overcorrected. Acular LS 4x/day for 48 hours, then stop because of epithelial toxicity. Copius preservative-free tears Punctal occlusion may be necessary Advil/ Tylenol for mild pain Vicodin/Lortab for moderate/ severe pain No swimming/dusty environments for 1 week Enhancement, if necessary, month 4-6. Patient Instructions After Laser Vision Correction Immediately After the Laser Treatment: 1. It is very important for you to go home and relax for the day. Try to sleep as much as possible for the first 24 hours after your procedure. If sleep is not possible, please try to keep your eyes closed. Sleep will tremendously speed your recovery. 2. You may eat or drink normally, but do not drink more than one or two glasses of any alcoholic beverage. 3. Take Tylenol, aspirin, or similar medications (unless allergic) for discomfort if needed. 4. Keep glasses, goggles, or clear plastic shields securely taped over your treated eye(s) until seen in the office tomorrow (except to instill drops). Tape shields or goggles when asleep. 5. Apply the following eyedrops as gently as possible during waking hours: a. Zymar or Vigamox (antibiotic), 1 drop 4 times a day b. Pred Forte (steroid), 1 drop 4 times a day (shake the bottle well) c. Artificial Tears every 2 hours d. Acular-PF, 1 drop every 4 hours, as necessary for pain 6. Do not rub your eyes. You may gently pat the eyelids with a clean facial tissue (with the eyes closed). 7. It is normal to experience any of the following: a. Feeling as if something is in your eye causing mild to moderate irritation and discomfort b. Eye watering c. Blurry vision d. Sensitivity to light. 8. Do not shower, take a bath, or wash your face during the first 12-18 hours after treatment (to avoid getting any soap or water in your eye(s)). Your one day follow-up appointment is on ____________________________ . Please bring your eye drops and your instruction sheets to your next visit. You can contact Dr. Dodge at any time on the office number: 818-783-8750. Instructions for the First Week After Laser Treatment 1. Apply the following eye drops during waking hours: a. Zymar or Vigamox (antibiotic), 1 drop 4 times a day for 5-7 days 2. 3. 4. 5. 6. 7. 8. 9. b. Pred Forte (steroid), 1 drop 4 times a day for 5-7 days (shake the bottle) c. Artificial Tears every 2 hours d. Acular-PF, 1 drop every 4 hours, as necessary for pain The clear plastic protective shield(s) or goggles must be used for one week at any time you sleep. Tape them in place when you nap during the day and at bedtime for 1 week. Do not rub your eye(s) for one week. You may gently blot or wipe your eyelids with a clean tissue while the eyes are closed. Do not wear eye make-up for 5 days. If possible, avoid areas with a high concentration of smoke or fumes for one week. No water sports for 1 week. You may resume your regular exercise routine the day after the procedure, however, as a precaution, use a sweatband for the first week. You may do light weights. Do not power lift for the first week. After one week, there are usually no restrictions, but always check with Dr. Dodge. We strongly recommend that you always wear protective goggles when participating in any sport or activity which might result in an injury to your eye. Your one week follow-up appointment is on ____________________________ Please bring your eye drops and your instruction sheets to your next visit. If you require an enhancement for maximal vision, we would typically schedule the procedure 3-4 months after your initial surgery. Nanotechnology Considerations of the various tissues and structures Tissue/ Structure Considerations Tear Film Quality of vision after blink Cornea Clarity, curvature, symmetry Lens Clarity, curvature, changes Media Clarity, Index of refraction Eyeball Potential “Marechal’s Criterion” Fovea Optic Nerve Visual Cortex Perceptual Effects Measurements o One micron is 0.001 Millimeters (One thousandth of a millimeter). The smallest corneal epithelial cell is 5 microns in diameter Epithelium is 40-80 microns and the Stroma is 450-500. o A nanometer is one thousandth of a micron, or about 3-4 atoms wide. This is the size range wherein physics, chemistry, electrical engineering, materials science, and biology converge. Simply stated, nanotechnology is molecular manufacturing. It builds things (anything) one atom or one molecule at a time, by robotics. Crystalline Lens o Current (and developing) refractive laser technologies (at 0.25microns accuracy) are fully capable of correcting higher order aberrations in the human eye and achieving higher order vision correction, but it is the quantum physics and biology of the surface of the human cornea plus other ocular, optical, and surgical limiting factors that make it impossible to achieve higher order correction through corneal refractive surgery. o So, if we cannot achieve higher order aberration correction due to the quantum physics and the biological limits of soft tissue (cornea), what about synthetic materials, i.e. intacs, inlays, onlays (CL)? o What about the crystalline lens? While the cornea remains relatively stable and prolate throughout life (unless, of course, we do something funny to it with corneal refractive surgery). The lens is constantly changing in size and shape from retained epithelial cells throughout life and becoming more spherical (oblate) resulting in increasing spherical aberrations. Beyond 20 years of age, the lens isn’t a real “friend” to the visual system. It adds spherical aberrations, which compromises qualitative vision. Beyond 40ish, prebyopia begins, and then the eventual formation of cataracts. o The modern cataract extraction procedure (Lensectomy) Standard small incision, clear cornea, sutureless, phacoemulsification, ECCE Done bilaterally, about one week apart. Ambulatory surgery with recovery time less than 24 hours. Complication <2% (<0.5% in most refractive practices) Safest surgical procedure in all of health care. Best if >40 years of age. If aspheric, decreases the HOA. o Special considerations in Refractive Lens Exchange vs. Cataract Surgery Biometry with IOL Master (Zeiss) essential Resultant astigmatism goal is 0 Consider only “high volume” cataract surgeons for refractive lens exchange. HICFA considers >400 cases per year high volume <400 a year means 5-10 cataract surgeries a week. The surgeon must be fast and good! o Synonyms for Refractive Lensectomy Refractive lens exchange (RLE) Clear lensectomy Clear lens exchange Presbyopic Lens Exchange (PRELEX) Lens-based refractive surgery o Phakic IOLs Variable materials Plastic Silicone Collagen (Collamer) by Starr in Phase 3 trials Variable designs Anterior Chamber o Acrysof, Alcon o GBR, IOL Tech o Kelman Duet, Tekia o Memory Lens, Ciba o NewLife, IOL Tech o NuVita, B&L o ThinOptX o Vision Membrane o 6H2, Oil Iris Supported o Artisan/Verisyse, Ophtec and AMO Posterior Chamber o PRL, Ciba o ICL, Staar o Beyond phakic IOLs, some interesting new developments in IOL technology are leading to the new concept of Refractive Lens Exchange. This is the removal of the crystalline lens in a clear of cataractous state and its replacement with a specialized intraocular lens to create an optimal refractive condition. Some examples of new developments in IOL technology to support the concept of refractive lens exchange. Perhaps, the most controversial new technologies involve presbyopia. Prebyopic Reduction Procedures o Anterior ciliary sclerotomy o Infrared scleral ablation (OptiVision by SurgiLight) o Scleral expansion bands (SEB or Presby) o “Blended vision” with CK o Accommodating IOLs (12) ACOR IOLs (“Piggybacked” multifocal/monofocal IOLs) AT 45 CrystLens (Bihinged moveable optics by C&C) DualOptics IOL (“Piggyback” system in animal studies) HumanOptics Akkommodative ICU (injected hydrophilic) Light Adjustable IOL (animal studies on molecular lens) Medennium SmartLens (thermodynamic hydrophilic) QuestVision FlexiOptic (haptic contoured to capsule bag) Sarafarazi Elliptical Accommodating IOL (B&L) Tecnis ZM001 IOL (Aspheric multifocal by Pfizer) Visiogen Synchrony IOL (dual anterior/posterior optics) Vivarte Baikoff IOL (Ciba) o Pseudo-accommodating IOLs (15) Array Multifocal Silicone IOL (AMO) +6 - +3-D (in 0.50D steps) Array 2 Silicone IOL (AMO) ReStor IOL (Alcon) Plano - +36D Resume Multifocal Acrylic IOL (AMO) -10 - +30D Tecnis MF (Pfizer, acquired by AMO) Comparing Refractive Corneal Surgery vs. Refractive Lens Exchange o Corneal Surgery Strengths It works Safe and effective Not intraocular surgery Simultaneous surgery Potential of custom ablation Universally accepted The “WOW” factor “Potential” for HOA correction Weaknesses Surgery on a healthy cornea Microkeratome risks Reduction in prolate shape Central corneal “insult” Risk of ectasia Limited correction change Induces higher order aberrations Remodeling and epithelial limits Royalties Capital investment Disruption of surgery schedule Cant treat presbyopia o Lens Surgery Strengths No flap Co central corneal insult Maintains prolate cornea Better results in higher powers Eliminates lens aberrations Correction at the nodal point HOA correction possible Stable (permanent) correction Routine surgery scheduling No royalties No capital investment Can treat presbyopia Weaknesses Intraocular surgery (with risks) Not done simultaneously Trade-offs (aberrations, etc) Risk of PCO Risk of CME Issues with corneal astigmatism Limited IOL technologies Need to take patient to OR ASC or hospital costs “Non-traditional” surgery (CLE) Limited “WOW” factor o Even refractive lens exchange really does not entirely address the limitations of HOA correction created by the cornea. If we cannot achieve higher order correction on the cornea or with refractive lens exchange, what about using synthetic materials? Wavefront programmed, constructed, and controlled “intelligent” spectacles and contact lenses o Photosensitizing methods o Electrochemical methods o Nanotechnology Nanotechnology o Nanotechnology proposes the construction of novel molecular devices possessing extraordinary properties. Anything can be “nanoconstructed.” Examples include synthetic materials, textiles, electronics, pharmaceuticals, nerve tissue, animal tissue, micro (nano) computers, virus (vectors), blood cells, stem cells, genes, anything you can imagine. It is not just refractive surgeries alone that are going to “sculpt” the future of refractive care. It is non-surgical refractive sciences that we are talking about. These are sciences that optometry can and must understand and deliver. Why Comanage? Youre the right doctor for the job. Evidence to your patients that you are a progressive doctor/practice. Clinical interest High immediate profit from professional services containing no material costs or third party o Co-management vs. CL Profits LASIK co-management fee = $1,000 2 week disposable profilts 8 boxes/year at $15/box = $120/year +$40 for eval = $160. $1,000 = 6.25 years. o After surgery, patients over time continue to need examinations, contact lenses, prescription eyewear, plano sunglasses, and further surgery. Referrals Control Why not? o Lack of knowledge o Fear of failure o Fear of success Pearls in LASIK CO-Management Stay ahead of the curve. Select only good solid candidates for the surgery Foster realistic expectations Demonstrate outcomes using contact lenses o Monovision o Distance OU outcome in presbyopic patients. Ex 1: 62yo with -4.00 OU. Never worn CL. Adamantly against MV. “Knows” she will need reading glasses after surgery. Ex 2: 55 yo office worker who anticipates 10 more years on the job. 90% computer and near work. Wears SV glasses ~10%. Goal is to have full distance for golf/bowling. Srx: -1.25/-2.00 o Previously untreated refractive amblyopes Ex 1: 21yo refractive amblyope. Srx -1.50 (20/20)/ -6.25 -2.75 x050 (20/80) o Unstable binocularity o Enhancements Ex1: 60yo MV LASIK 8 years ago. Reversed MV 3 years ago. Wants to be retreated again for MV. Document everything Make yourself available/ accessible Discourage enhancement whenever possible. Top 10 Mistakes in Co-Management Refraction Failure to assure refractive stability Failure to adequately manage dry eyes Failure to diagnose and aggressively treat chronic lid disease o Blepharitis, Meibomian Gland Dysfunction Failure in creating a surgical game plan o Full distance o MV o “Modified MV” o Bilateral “soft” distance o Staggered surgery Failure to anticipate the “downside” of surgery Failure to schedule interim visits when needed Failure to refer back when needed Failure to communicate Failure to be accessible/available How to Build a LASIK Practice Speak regularly to all candidates about their potential and your role in comanagement Speak to all non-candidates about why Mailings (recall), office literature (pamphlets), signage (posters), etc. Attend surgeries Have a LASIK coordinator Help with financing Case presentations Why its in their best interest? You know their eyes the best. You will be their advocate Lifetime commitement You will help choose the best laser. You will help choose the best surgeon Consultation Develop a LASIK Instinct o Patient profile Reasons, expectations Wishes, dreams, and desires Realistic? Acheivable? o Honesty Establish a relationship and rapport Emphasize a team effort between your office and the surgeon for a “total visual experience.”