NIGERIA The Making it Happen Programme The aim of the Making it
advertisement
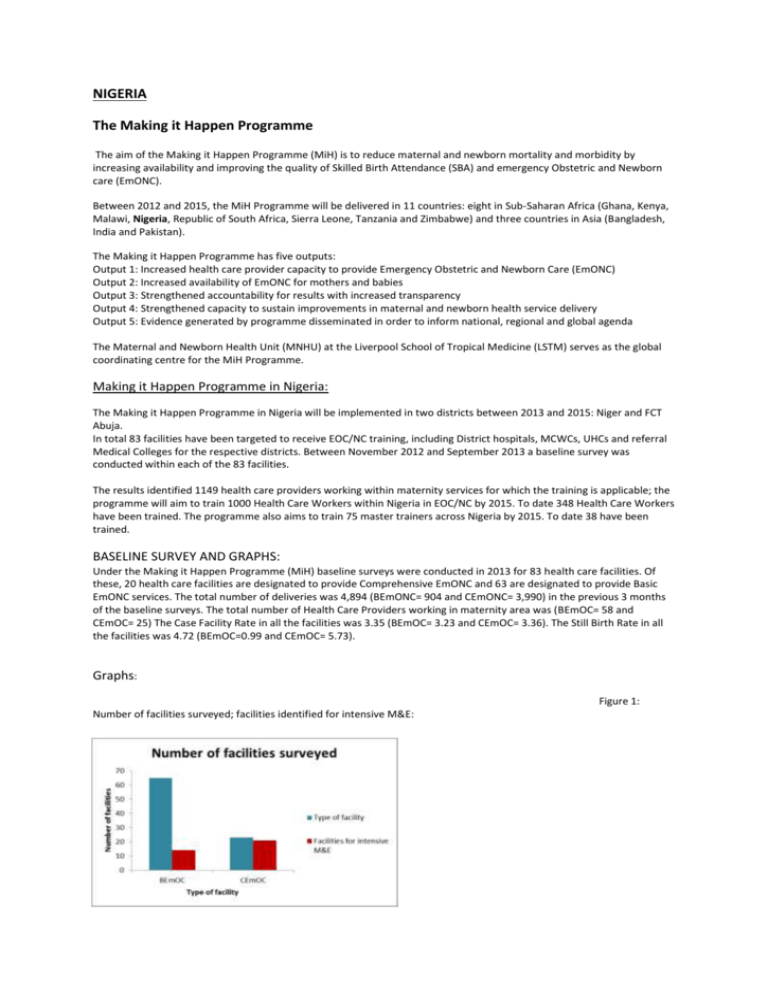
NIGERIA The Making it Happen Programme The aim of the Making it Happen Programme (MiH) is to reduce maternal and newborn mortality and morbidity by increasing availability and improving the quality of Skilled Birth Attendance (SBA) and emergency Obstetric and Newborn care (EmONC). Between 2012 and 2015, the MiH Programme will be delivered in 11 countries: eight in Sub-Saharan Africa (Ghana, Kenya, Malawi, Nigeria, Republic of South Africa, Sierra Leone, Tanzania and Zimbabwe) and three countries in Asia (Bangladesh, India and Pakistan). The Making it Happen Programme has five outputs: Output 1: Increased health care provider capacity to provide Emergency Obstetric and Newborn Care (EmONC) Output 2: Increased availability of EmONC for mothers and babies Output 3: Strengthened accountability for results with increased transparency Output 4: Strengthened capacity to sustain improvements in maternal and newborn health service delivery Output 5: Evidence generated by programme disseminated in order to inform national, regional and global agenda The Maternal and Newborn Health Unit (MNHU) at the Liverpool School of Tropical Medicine (LSTM) serves as the global coordinating centre for the MiH Programme. Making it Happen Programme in Nigeria: The Making it Happen Programme in Nigeria will be implemented in two districts between 2013 and 2015: Niger and FCT Abuja. In total 83 facilities have been targeted to receive EOC/NC training, including District hospitals, MCWCs, UHCs and referral Medical Colleges for the respective districts. Between November 2012 and September 2013 a baseline survey was conducted within each of the 83 facilities. The results identified 1149 health care providers working within maternity services for which the training is applicable; the programme will aim to train 1000 Health Care Workers within Nigeria in EOC/NC by 2015. To date 348 Health Care Workers have been trained. The programme also aims to train 75 master trainers across Nigeria by 2015. To date 38 have been trained. BASELINE SURVEY AND GRAPHS: Under the Making it Happen Programme (MiH) baseline surveys were conducted in 2013 for 83 health care facilities. Of these, 20 health care facilities are designated to provide Comprehensive EmONC and 63 are designated to provide Basic EmONC services. The total number of deliveries was 4,894 (BEmONC= 904 and CEmONC= 3,990) in the previous 3 months of the baseline surveys. The total number of Health Care Providers working in maternity area was (BEmOC= 58 and CEmOC= 25) The Case Facility Rate in all the facilities was 3.35 (BEmOC= 3.23 and CEmOC= 3.36). The Still Birth Rate in all the facilities was 4.72 (BEmOC=0.99 and CEmOC= 5.73). Graphs: Figure 1: Number of facilities surveyed; facilities identified for intensive M&E: Figure 2: Number of deliveries in the facilities: Figure 2: Number of deliveries in the facilities: Country Information Nigeria is located in West Africa sharing the border with Benin in the west, Cameroon and Chad in the east, Niger in the north and the south by the Atlantic Ocean. With a population of about 162 million it is the most populous African country. The country comprises of 36 states and a Federal Capital Territory, Abuja. Nigeria has abundance of natural resources, particularly oil and natural gas. Half of the population lives in rural areas. The life expectancy at birth is 54 years for women and 53 years for men (NDHS, 2008)1. 1 National Population Commission (NPC) [Nigeria] and ICF Macro. 2009. Nigeria Demographic and Health Survey 2008. Abuja, Nigeria: National Population Commission and ICF Macro. Key MNH Indicators Maternal Mortality Ratio: 630/100,000 live births (2010) *2 % Skilled Birth Attendance: 34 (2010) **2 % Contraceptive Prevalence Rate: 14 (2011) +2 Total fertility Rate: 5.7 (2011) Ante-Natal Care (at least one visit): 53 (2010) **2 *: WHO statistics, 2013 http://apps.who.int/gho/data/kenya: Trends in Maternal Mortality: 1990 to 2010. WHO, UNICEF, UNFPA and the World Bank. Geneva, World Health Organization, 2012 (http://whqlibdoc.who.int/publications/2012/9789241503631_eng.pdf). **: WHO global database on maternal health indicators, 2013 update. Geneva, World Health Organization (http://www.who.int/gho). +: World Contraceptive Use 2012. United Nations, of Economic and SocialAffairs, Population Division, 2012. WHO regional, Source: MDGDepartment global database (http://mdgs.un.org/unsd/mdg/Data.aspx) income-group and global aggregates refer to 2010. The methodology for the aggregates is available in World ContraceptiveUse 2012 and in the technical paper: Alkema, et al. National, regional and global levels and trends in contraceptive prevalence and unmet need for family planning between 1990 and 2015: a systematic and comprehensive analysis (forthcoming). ++: World Population Prospects: the 2010 Revision. New York, Population Division, Department of Economic and Social Affairs, United Nations Secretariat, 2011. Map of Nigeria illustrating target regions and distribution of health care facilities for MiH Organization of Health Care Delivery Health care is delivered at primary, secondary and tertiary levels, which are respectively managed by Local, State and Federal Government structures. Public health facilities have the following types of health care facilities: teaching hospitals, federal medical centres, state general hospitals, primary health care units, health centres and dispensaries. The number and functionality of each of these types of facilities varies considerably across the different geographical regions and states. Human Resource for Health The Health workforce in Nigeria is considered one of the largest on the continent. In 2007, there were 52,408 physicians with a ratio of 3.7 doctors per 1,000 population. In the nursing/midwifery category there were 219,407 practitioners of whom 128,918 were Registered Nurses and 90,489 were Registered Midwives. The ratio per 1,000 population for this category of staff was 9.1 for Registered Nurses and 6.4 for Registered Midwives (AHWO, 2008)2. Despite these seemingly acceptable ratios there is marked regional variation in the ratio of health worker to population with a concentration of health workers in urban areas and dearth of health workers in rural parts where half of the population is resident. In an effort to fast track the reduction of maternal, newborn and child mortality and morbidity in the country, the National Primary Health Care Development Agency (NPHCDA), was formed. The scheme mobilises midwives on a one year mandatory community midwifery that involves unemployed and retired midwives and deploys them to selected primary health care facilities in rural communities so as to increase SBA coverage. The scheme has successfully recorded increase in antenatal visits, delivery with a skilled birth attendant and uptake on family planning services. The National Youth Service Corps scheme (NYSC) is another initiative aimed at obligating university graduates from various professions to serve a year in the public service. This includes both midwives and medical doctors. These skilled birth attendants should be able to provide emergency obstetric care in parts of the country with very few SBAs. Maternal Mortality Ratio (MMR) and Under-five Mortality Rate Nigeria has shown an improvement in its Maternal Mortality Ratio (MMR) over the two decades from 1990 to 2010. In 1990 it was estimated that the MMR was 1,100 per 100,000 live births, in 2010 it had gone down to 630 per 100,000 live births (WHO, 2012)3. Official figures from the Nigeria Demographic and Health Survey report 2008 (NDHS 2008) 1 are even lower 545 per 100,000 live births. The target for 2015 in terms of MMR is 250 per 100,000 live births. Under-five mortality has been estimated as 124 per 1,000 live births. Over the 21 years from 1990 to 2011, the Infant Mortality Rate (IMR) has similarly shown a decline from 127 to 78 per 1,000 live births. The goal set forth in terms of MDG4 is an IMR of 30.3/1,000 live births by 2015. Maternal and Newborn Health Situation The Total Fertility Rate (TFR) is estimated to be 5.7, with an average annual reduction rate between 1990 and 2011 of 1% per annum. Total Fertility rates vary between urban and rural areas, 4.7 and 6.3 respectively. The contraceptive prevalence for women in Nigeria is 70% with women knowing at least one modern method of contraception. However nearly all (95%) of unmarried women know a modern method of contraception compared to 68% of married women. 5 Haemorrhage and eclampsia remain the leading causes of maternal deaths being responsible for more than half of all maternal deaths. Post-partum deaths account for a higher proportion of maternal deaths (73%), a rise of 6% since 2001. Therefore efforts need to continue to strengthen access to treatment, improve referral systems and improve care at the referral level. Data from the (NDHS, 2008), shows that the number of children dying before their first birthday has decreased from 99 per 1000 (2003) to 75 per 1000 births and with 1 in 6 children dying before the age of 5. Childhood mortality rates also drop depending on area of residence with under 5’s mortality rates 10 years prior to (NDHS, 2008) 5 being 121 per 1000 in urban areas compared to 191 per 1000 in rural areas 5. Mother’s education also plays a role in infant mortality with an infant 3 times more likely to die in the care of a mother with no education compared to that of those mothers with secondary education (NDHS, 2008)5. Skilled Birth Attendance and Emergency Obstetric and Newborn Care In Nigeria, 58% of women receive some antenatal care(ANC) from a skilled provider, most commonly from a nurse or midwife (30%) or a doctor (23%).The percentage of births attended by a SBA was reported in 2008 is 39% by NDHS and 34% by WHO in 2012. All MDG5 indicators are significantly worse in the north compared to the southern part of the 3 Africa Health Workforce Observatory (2008), Human Resources for Health Country Profile Nigeria, http://www.unfpa.org/sowmy/resources/docs/library/R050_AHWO_2008_Nigeria_HRHProfile.pdf (Accessed June 2013). 4 WHO, UNICEF, UNFPA and the World Bank (2012), Trends in Maternal Mortality: 1990 to 2010, http://www.who.int/reproductivehealth/publications/monitoring/9789241503631/en/index.html (Accessed June 2013). 5 National Population Commission (NPC) and ICF Macro. 2009. Nigeria Demographic and Health Survey 2008: Key Findings. Calverton, Maryland, USA: NPC and ICF Macro. country. Well coordinated interventions are required to improve the health indicators of the country as a whole as there are significant regional disparities in health status, service delivery and availability of resources (WHO Stats, 2013)2.