3. antibiotic prescribing for uti in females
advertisement

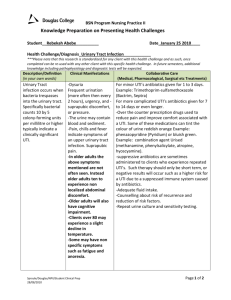
CEPP National Audit – Focus on Antibiotic Prescribing 3. ANTIBIOTIC PRESCRIBING FOR UTI IN FEMALES Background AWMSG NPI: Antibacterial items per 1,000 STAR-PUs The development of antibiotic NPIs supports one of the core elements of the Welsh Antimicrobial Resistance Programme: to inform, support and promote the prudent use of antimicrobials. Information from PHE Management of Infection Guidance for Primary Care for Consultation and Local Adaptation1: Illness Comments Medicine Adult dose Duration of treatment Treat women with severe/or ≥ 3 symptoms nitrofurantoin 100 mg m/r BD Women mild/or ≤ 2 symptoms AND trimethoprim7B+ 200 mg BD Women all ages: 3 a) Urine NOT cloudy 97% negative predictive value days2,12,13A+ pivmecillinam 400 mg STAT then 200 mg TDS (NPV), do not treat unless other risk factors for UTI in adults Men: 7 days1,5C If organism susceptible infection 500 mg TDS (no fever or b) If cloudy urine use dipstick to guide treatment. amoxicillin14B+ flank pain) Nitrite plus blood or leucocytes has 92% positive PHE URINE predictive value; nitrite, leucocytes, blood all Use nitrofurantoin first line as general resistance and community multi-resistant SIGN negative 76% NPV4AExtended-spectrum Beta-lactamase E. coli are increasing. Trimethoprim (if low risk of resistance) CKS women c) Consider a back-up/delayed antibiotic option20A and pivmecillinam are alternative first line agents. CKS men Men: Consider prostatitis and send pre-treatment Risk factors for increased resistance include: care home resident, recurrent UTI, RCGP UTI MSU1,5C OR if symptoms mild/non-specific, use hospitalisation >7d in the last 6 months, unresolving urinary symptoms, recent travel to a country clinical negative dipstick to exclude UTI6C with increased antimicrobial resistance (outside Northern Europe and Australasia) especially module Always safety net. health related, previous known UTI resistant to trimethoprim, cephalosporins or quinolones 19 SAPG UTI 24-5 First line: Nitrofurantoin if GFR over 45 ml/min If increased resistance risk, send culture for susceptibility testing & give safety net advice. If GFR 30–45: only use if resistance and no GFR<45 ml/min or elderly consider pivmecillinam 21-3, 28 or fosfomycin (3 g stat in women15,16B,17A alternative plus 2nd 3 g dose in men 3 days later18) In treatment failure: always perform culture1B Signs and symptoms of a UTI are dysuria, urgency, frequency, polyuria, suprapubic tenderness and haematuria. 1,2A,3C 8B+ 9C 10B+ 11C SIGN 88 states: Do not routinely prescribe antibiotic prophylaxis to prevent symptomatic UTI in patients with catheters2. Consider antibiotic prophylaxis in patients for whom infections are of such frequency or severity that they chronically impinge on function and well-being2. When changing catheters, antibiotic prophylaxis should only be used for people with a history of catheter-associated urinary tract infection following catheter change2. NICE Quality Standard 90 (QS90) published in June 2015 provides the following quality statements on UTIs in adults: Statement 2. Healthcare professionals do not use dipstick testing to diagnose urinary tract infections in adults with urinary catheters. Statement 4. Adults with a urinary tract infection not responding to initial antibiotic treatment have a urine culture. Statement 6. Healthcare professionals do not prescribe antibiotic prophylaxis to adults with long-term indwelling catheters to prevent urinary tract infection unless there is a history of recurrent or severe urinary tract infection3. Page 1 of 5 All Wales Medicines Strategy Group Method There are two options for this audit section: Method 1 identifies women with urinary infection. Method 2 identifies people with indwelling urinary catheters. Start the searches using a 3-month window and extend it if necessary to reach the required number of cases. Following the audit, complete the Review Sheet and ensure that this includes achievement against the NICE Quality Standards. Method 1: Women with urinary tract infection Assess a reasonable sample of records with a diagnosis of UTI (female only) (see section on Sample size). Exclude pregnant females, men, children and patients with acute pyelonephritis. Please note that the advice to record the cloudiness of urine is new (2014) and may not be recorded in consultations for the first cycle of the audit. Search using the following Read Codes: R081 K15 K190 1J4 Page 2 of 5 Dysuria Cystitis Urinary tract infection Suspected UTI CEPP National Audit – Focus on Antibiotic Prescribing Data collection sheet (Method 1) Patient Cloudy urine? (Y/N/not recorded) ≤2 symptoms ? (Y/N) ≥3 symptoms ? (Y/N) Antibiotic given? (Y/N) Where antibiotic given, were there either 3 or more symptoms or a positive urine dip recorded? (Y/N) Trimethoprim or nitrofurantoin ? (Y/N) 90% 95% Other antibiotic (record name and reason, where given) Antibiotic course length (number of days) No fever or flank pain, course length = 3 days (Y/N/Not applicable) If second course of antibiotics for same episode of infection, was a midstream specimen of urine (MSU) sent? (Y/N) If single course of antibiotics given, leave blank Total % Yes Standard Locally defined Page 3 of 5 All Wales Medicines Strategy Group Method 2: People with indwelling urinary catheters Identify a reasonable sample of patients who use indwelling urinary catheters (see section on Sample size). In primary care, methods to identify patients using catheters will vary between practices. Consider: (i) Electronic identification. Search for patients who have had an acute/repeat prescription for catheter items issued in the last 3 months. This report will include catheters issued for intermittent self-catheterisation. Before undertaking the audit, confirm that the patient has an indwelling urinary catheter. These are issued in small numbers unlike intermittent catheters which are normally issued in larger quantities e.g. over 28/month. (ii) Informal enquiry of nursing home and care homes or the district nursing team. Following the audit, complete the Review Sheet. Data collection sheet (Method 2) Patient Antibiotics for urinary infection in the last 12 months: None, Acute (A), Prophylaxis (P)? (A) + (P)? Acute infection Was the latest suspected infection investigated with dipstick testing? (Y/N/no suspected infections) Total Number patients reviewed = None = A= P= Number y/number of patients with suspected acute infections % Yes A + P/number reviewed x 100 Standard Page 4 of 5 0% Other reasons given for prescribing (urinary tract) antibiotics Are these reasonable indications? Prophylaxis? (Y/N) Number y/number of patients reviewed To be agreed locally. Suggest less than 10% Prophylaxis History of frequent & severe urinary infections? Catheter change prophylaxis: history of UTI following catheter change? (Y/N/uncertain) Number y/number of patients on prophylaxis 100% CEPP National Audit – Focus on Antibiotic Prescribing REFERENCES 1 Public Health England. Management of infection guidance for primary care for consultation and local adaptation. 2014. Available at: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/377509/PHE_Primary_Care_guidance_14_11_14.pdf. Accessed Feb 2015. 2 Scottish Intercollegiate Guidelines Network. SIGN 88 Management of suspected bacterial urinary tract infection in adults. 2012. Available at: http://www.sign.ac.uk/pdf/sign88.pdf. Accessed Mar 2015. 3 National Institute for Health and Care Excellence. Quality Standard 90. Urinary tract infections in adults. Jun 2015. Available at: https://www.nice.org.uk/guidance/qs90/resources/guidance-urinary-tract-infections-in-adults-pdf. Accessed Jun 2015. Page 5 of 5