Blood Transfusion in ICU
advertisement

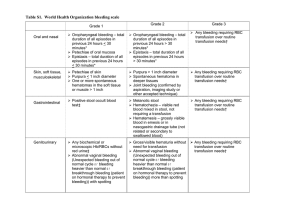
Blood Transfusion in ICU 8/2/11 PY Mindmaps SP Notes - anaemia common in ICU - tendency to more restrictive strategy c/o increased morbidity associated with transfusion - general attempts to minimize the requirement for blood transfusion should be pursued: -> -> -> -> -> -> -> -> -> stopping bleeding early stop unnecessary anticoagulation minimising venesection treat hypothermia and acidosis GI prophylaxis Fe2+ nutrition consideration of EPO therapy use of FVIIA - transfusion triggers are dependent on many variables: 1. 2. 3. 4. evidence of bleeding and stability to patient reason for admission (trauma, GIH) patient wishes (Jehovah’s witness) co-morbid conditions (such as ischaemic heart disease) BLEEDING - lower threshold to transfuse - adults: aim to keep Hb > 80 g/L until bleeding controlled - trauma patient: -> haemostatic resuscitation: early products in a 1:1:1 ratio (RBC:platelets:plasma) -> permissive hypotension -> damage control surgery -> avoid hypothermia, acidosis and coagulopathy NON-BLEEDING - controversial TRICC trial (NEJM, 1999) - critically ill, normovolaemic, non-bleeding MRCT n = 838 restrictive (70g/L) vs liberal groups (100g/L) as transfusion thresholds no difference in mortality increased complications in liberal strategy group (APO, ARDS) under powered prior to leukodepletion Jeremy Fernando (2011) TRACS trial (JAMA, 2010) - post cardiac surgical patients RCT n = 502 HCT 30% vs HCT > 24% no difference in mortality and severe morbidity large separation between groups not achieved high base line event rate number of RBC’s transfused was an independent risk factor for clinical complications CONTROVERSIAL ISSUES Storage lesion - increased peri-operative complications organ failure sepsis mortality VTE Old vs New blood - decreased deformability -> impedes microvascular flow - depletion of 2, 3 DPG -> left shifted oxy-Hb dissociation curve -> reduces O2 delivery - increased adhesiveness and aggregability - reduced concentration of NO - reduced ATP -> reduced ability to maintain biconcave shape - accumulation of proinflammatory bioactive substances - haemolysis over time - progressive increase in K+ concentration (20mmol/L @ day 28) -> despite this hyperkalaemia uncommon complication - progressive acidaemia (pH 6.7 @ day 28) - hypomagnasaemia - citrate exposure -> hypocalcaemia Leucodepletion - decreases risk of TRALI - reduction in non-haemolytic transfusion reactions - reduction in CMV transmission - improved chance of finding an organ transplant match if required - reduction in storage lesion effect - reduction in graft vs host disease - reduction in mortality after universal leukodepletion in cardiac surgical, orthopaedic and trauma populations (Hebert, JAMA, 2003) EPO - decreases transfusion requirements - increased thrombotic complications - being investigated in trauma and traumatic brain injury Jeremy Fernando (2011) FVIIa - stops bleeding but increased risk of thrombosis and embolic disease Undefined threshold for IHD patients MY APPROACH - minimise transfusion requirements using other means - if bleeding: transfuse aggressively until bleeding controlled (avoid hypothermia, acidosis and coagulopathy). - if not bleeding: restrictive strategy in those who can tolerate it and more liberal in those that have evidence of ischaemic end-organ dysfunction. - ideally use new, leucodepleted blood Jeremy Fernando (2011)