Behavioral - Paramedic and Nursing Study
advertisement

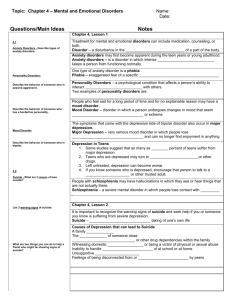
Behavioral and Psychiatric Emergencies Agitation - Excessive restlessness associated with mental illness. Psychomotor Activity - Psychological processes associated with muscle movement. Binging - Lack of control over eating. Hallucination - A sensory perception not based in reality. Delusion - A fixed, false belief despite evidence to the contrary. Bereavement - Intense suffering after a tragic loss. Cognition - Mental activities pertaining to learning, memory, and thinking. Affect - An external display of internal feelings. Insight - An understanding of the motives and reasons behind one’s own actions. Psychosis - Dysfunction of thought and behavior. Each year around 4.3 to 7.4 million people receive treatment in an emergency department for mental health-related conditions. Moreover, around 1/3 of mental health patients use an ambulance to access the ED.1,2 Therefore, a considerable number of the emergencies to which you respond may involve a patient with a behavioral or psychiatric condition. Patients suffering from mental health disorders can have a variety of presentations, and these disorders can be caused by many different conditions. Accordingly, the assessment and management of these patients can be one of the most challenging tasks you will have to perform as a member of the emergency medical services. However, it can also be one of the most rewarding, as you have the opportunity to prevent many unnecessary deaths, as well as to help patients receive the psychiatric care that they need. The following course will begin by identifying definitions related to behavioral and psychiatric conditions. After that, the basic epidemiology of behavioral and psychiatric disorders will be listed. Next, the psychopathology of mental health disorders will be presented. This will be followed by a description of the main types of behavioral and psychiatric conditions. After that, essential elements of the assessment and management of patients suffering from mental health emergencies will be identified. The course will conclude with a brief discussion of the medico-legal aspects of the care of mental health patients. Basic Definitions: -Abnormal Behavior: Is a behavior that deviates from society’s norms and expectations. -Behavior: Is any observable activity of a person, whether mental activity or motor activity. -Behavioral Emergency: Is a condition characterized by behavior that is unacceptable, intolerable, or dangerous to the patient and or others, and that requires intervention. Behavioral emergencies can be precipitated by extremes of emotion, or they can be due to a psychological or physical condition. -Mental Status: Is the state of a person’s mental function, based on his or her attention span, memory, orientation, speech, and judgment. -Open-Ended Question: Is a question that cannot be answered with a simple yes or no. -Posture: Is the position of the limbs or body as a whole. Definitions Pertaining to Emotions: -Anger: Is a feeling of hostility or rage. -Anxiety: Is a feeling of dread or impending doom that is not realistically based or well defined. -Confusion: Is an emotional state characterized by inappropriate reactions to environmental stimuli due to disorientation of the affected individual. -Depression: Is a mental state characterized by feelings of sadness or worthlessness accompanied by objective signs, such as appetite changes, fatigue, and sleep disturbances. -Fear: Is a feeling of dread, apprehension, or alarm caused by an identifiable stimulus. Definitions of Mood and Affect: -Mood: Is a pervasive, internal emotional state. -A mood is like a season. For example, in winter, the pervasive state is that of cold. -Affect: Is an external display of internal feelings. -Affect is like the weather that is displayed at any point in time during a particular season. For example, in winter, it can be raining, snowing, or dry. Definitions Pertaining to Thoughts: -Delusion: Is a fixed, false belief despite evidence to the contrary. -Hallucination: Is a sensory perception not based in reality. General Epidemiology: -Around 20% of people suffer from a mental illness each year.3,4 -One in seven people will require treatment for a behavioral or emotional disturbance. -Mental health disorders are some of the most incapacitating health problems.4 The Epidemiology of ED Visits: -There are 4.3 to 7.4 million mental health/psychiatric related ED visits per year. -This accounts for 5.4% to 6.4% of all ED visits. -1/3 of mental health patients use an ambulance to access the ED. -Patients with substance abuse or suicide-related emergencies utilize ambulances more frequently than those presenting for other disorders. -Substance abuse accounts for 27% of patient presentations. -Neuroses account for 26% of patient presentations. -Psychoses account for 21% of patient presentations. -Psychiatric-related ED visits increased 15% between 1992 and 2000.1,2 The Epidemiology of Suicide: -Each day, over 1500 people attempt suicide and around 86 succeed. -The attempted to completed suicide ratio is around 8:1. -Over a period of study from 1997-2001, there were approximately 412,000 ED visits annually for attempted suicide and self-inflicted injury. -Attempted suicides account for 0.4% of all ED visits. -The most common method of self-injury in a study by Doshi et al. (2005) was poisoning (at 68%), followed by cutting or piercing (at 20%). Hanging and firearms were each responsible for less than 1% of ED visits for attempted suicide. -Poisoning by unspecified drugs or medicinal substances was most common (at 28%), followed by tranquilizers and psychotropic agents (at 27%), and then by analgesics, antirheumatics, and antipyretics (at 25%). -One third of attempted suicide/self-inflicted injury visits resulted in direct hospitalization in the Doshi et al. study.5 Introduction: Behavioral changes are brought about by a number of factors, including: emotional stress, psychiatric problems, medical illness, and substance abuse. Organic (or Biologic) Causes of Mental Health Emergencies Include: -Hypoxemia. -Hypoglycemia. -Hypothyroidism and hyperthyroidism. -Head trauma. -Substance ingestion, such as alcohol, depressants, narcotics, psychedelic agents, or stimulants. -Severe fluctuations in temperature. -Post-seizure behavior changes. -Central nervous system diseases, such as: -Infections of the brain (known as encephalitis), and the membranes lining the brain (known as meningitis). -Tumors. -Degenerative nervous system disease (such as Parkinson’s disease). ****NOTE: Features suggestive of an organic cause include: rapid onset, late age of first onset, absence of history of a psychiatric illness, medication non-compliance, initiation of a new medication regimen, and intoxication. Psychosocial Causes of Mental Health Emergencies Include: -Childhood trauma. -Dysfunctional family. -Abusive parents. -Parental deprivation. -Unstable living conditions. -Inability to cope with loss. Socio-Cultural Causes of Mental Health Emergencies Include: -Acts of violence, such as war, riots, rape, and assault. -Death of a loved one. -Prejudice and discrimination. -Deviation from cultural norms. -Economic and unemployment problems. Misconception 1: They are shameful and embarrassing. Reality: These are common conditions that affect one’s health. Misconception 2: They are never curable. Reality: There are many treatments available for these conditions. Misconception 3: All mental patients are dangerous and unstable. Reality: Most patients function normally on a daily basis.18 ****NOTE: A common reason for EMS intervention is for a psychiatric patient that forgot to take his or her medications. When assessing a patient suffering from a behavioral or psychiatric disorder, your first priorities should be to determine if the patient is suffering from a life threatening medical or traumatic condition and to determine whether the patient is at risk of harming him/herself or others. Determining the specific behavioral or psychiatric diagnosis should not be your focus. However, increasing your general knowledge of the spectrum of psychiatric and behavioral disorders will enable you to better understand your patients and to more effectively communicate with other healthcare personnel. Therefore, the following sections will discuss the essential characteristics of the different types of psychiatric conditions. The definitions of specific conditions come from the Diagnostic and Statistical Manual of Mental Disorders, also known as the DSM, which is published by the American Psychiatric Association. It is currently in its fourth version. This manual provides healthcare personnel with the diagnostic criteria for all currently defined psychiatric disorders. Description: Psychotic disorders are characterized by a gross distortion of reality, bizarre delusions, social withdrawal, and lack of emotional expression. The term psychosis refers to dysfunctions of thought and of behavior. Epidemiology: -Schizophrenia has a 1% lifetime prevalence.6-8 -Psychoses, such as schizophrenia, account for around 900,000 ED visits annually.8 -Schizophrenia is disproportionately more common among homeless persons. -The onset typically occurs in a person’s late teens to late 20s. -The suicide rate of patients with schizophrenia is around 10% to 13%.6 Examination Findings: -Patients with schizophrenia present with both positive and negative symptoms. -Positive symptoms (meaning symptoms that are present) include: -Hallucinations, most commonly auditory or visual. -Disorganized and or eccentric behavior. -Delusions. -Agitation. -Incoherent thoughts. -Tangentiality (tending to digress from one topic to another). -Negative symptoms (meaning the absence of normal mental and social functions) include: -Decreased speech (known as alogia). -Flat affect (defined as a decreased range of expression). -Poor self-care. -Loss of motivation. -Loss of social interest. -Additionally: -Depression often occurs and can be severe. -The patient may exhibit cognitive dysfunction (attention and memory deficits). -Insight and judgment are impaired. Diagnostic Criteria: -Two or more symptoms must be present for 6 months: -Delusions. -Disorganized speech. -Disorganized behavior. -Hallucinations. -Negative symptoms, such as flat affect and avolition. -Additional criteria include: -The disorder causes significant impairment in social and or occupational function. -The disorder is not due to a medical condition or substance abuse. Assessment and Management: -Protect yourself, the patient, and others. -Restrain the patient, if necessary, and per local protocol. -Maintain alertness. -Assess and stabilize the ABCs. -Obtain a SAMPLE history and head to toe physical exam. -See the “Assessment and Management” sections of this course for further details. -Determine the suicide risk. -Manage co-existing medical and or traumatic conditions. Medications the patient may be taking: -Atypical Antipsychotics, such as: -Risperidone (trade name Risperdal®). -Olanzapine (trade name Zyprexa®). -Quetiapine (trade name Seroquel®). -Ziprasidone (trade name Geodon®). -Aripiprazole (trade name Abilify®). -Clozapine (trade name Clozaril®). -Typical Antipsychotics, such as: -Chlorpromazine (trade name Thorazine®). -Thioridazine (trade name Mellaril®). -Haloperidol (trade name Haldol®). -Loxapine (trade name Loxitane®). Other Concerns: -Patients with schizophrenia have a high risk for homicide and suicide.7 -1/3 attempt suicide. -10% complete suicide. -This tendency toward violent behavior can be especially concerning if the patient is suffering from command hallucinations (hallucinations in which a patient believes that he or she has orders to harm him/herself or others).6 Special Note on a Subtype of Schizophrenia – Paranoid Schizophrenia: These patients exhibit extreme, unwarranted mistrust or suspiciousness. A paranoid schizophrenic believes someone is out to get him or her. In addition, the patient may appear cold, antagonistic, defensive, hypersensitive, and argumentative. These patients typically avoid intimacy and may exhibit unpredictable behavior, such as outbursts of aggression or bizarre behavior. Description: Mood disorders are characterized by a period of time when a particular mood dominates a person’s life. Mood is defined as a pervasive, sustained emotion. In general, there are two types of mood disorders: depression and bipolar disorder. Depression: -Definition: Depression is a mental state characterized by persistent feelings of sadness, often associated with physical signs such as changes in sleep, appetite, energy, and activity. -Other Characteristics of Depression Include: -Patients often feel worthless and hopeless. -They often state a desire to be left alone. -The condition results in significant impairment of functioning. -The condition is typically episodic with periods of remission. -Epidemiology: -Depression is one of the most prevalent psychiatric conditions. -The lifetime prevalence is 5% to 20%.7 -Depression is a major cause of suicide – 15% risk.6 -Signs and Symptoms Include: -Persistent sadness along with the following signs and symptoms: -To help remember this list it is useful to use the mnemonic “SIG – E – CAPS.” -S = Sleep changes (which can be increased or decreased). -I = Interest (which is exhibited as a loss of interest in pleasurable activities). -G = Guilt (which is exhibited as feelings of guilt or worthlessness). -E = Energy (which is exhibited as fatigue and decreased energy). -C = Concentration (which is exhibited as decreased concentration). -A = Appetite (which can be increased or decreased). -P = Psychomotor (which means that patient movements can be agitated or slowed). -S = Suicide (which is exhibited as thoughts of suicide). -Diagnostic Criteria Include: -5 or more symptoms present for a 2 week period of time. One of the five symptoms must be depressed mood or loss of interest in pleasurable activities. **Depressed mood. **Loss of interest in pleasurable activities. -Changes in weight. -Excessive guilt or feelings of worthlessness. -Thoughts of death or suicide. -Sleep disturbances. -Psychomotor agitation or retardation. -Loss of energy, feelings of fatigue. -Difficulty concentrating. -Additional criteria include: -The disorder causes significant impairment in social and or occupational function. -The disorder is not due to a medical condition or substance abuse. -Medications the patient may be taking: -SSRI (selective serotonin reuptake inhibitors) Antidepressants, such as: -Fluoxetine (trade name Prozac®). -Sertraline (trade name Zoloft®). -Paroxetine (trade name Paxil®). -Citalopram (trade name Celexa®). -Escitalopram (trade name Lexapro®). -Atypical Antidepressants, such as: -Venlafaxine (trade name Effexor®). -Bupropion (trade name Wellbutrin®). -Tricyclic Antidepressants, such as: -Desipramine (trade name Norpramin®). -Nortriptyline (trade name Pamelor®). -Amitriptyline (trade name Elavil®). -Imipramine (trade name Tofranil®). -Clomipramine (trade name Anafranil®). -Other Concerns: -Depression is often accompanied by other conditions, such as substance abuse or anxiety. -Depression can complicate the presentation of medical conditions, such as cardiovascular disease or diabetes. -Depression often follows episodes of severe stress. -Depression is differentiated from normal bereavement (which is defined as intense suffering after tragic loss), in that normal bereavement does not last longer than 2 months. Bipolar Disorder: -Definition: Bipolar disorder is a condition characterized by the presence of at least one episode of mania, which lasts at least one week. Mania is a persistently elevated, expansive, and irritable mood. -Other Characteristics: -A patient with bipolar disorder typically suffers from alternating depression, manic episodes, and normal moods. -Depressive periods last longer than manic episodes. -Delusions or hallucinations can occur in either manic or depressive stages. -The patient can quickly become argumentative, violent, and suicidal. -Manic episodes are accompanied by reckless behavior, such as excessive spending, gambling, or sexual promiscuity. -Epidemiology: -The suicide rate for bipolar disorder is 10% to 15%.6 -The lifetime prevalence of bipolar disorder is 0.4% to 1.6%.7 -Signs and Symptoms: -To help recall the signs and symptoms of bipolar disorder, the mnemonic “DIG – FAST” is used. -D = Distractibility (which means the patient can easily lose focus). -I = Insomnia (which means the patient has a decreased need for sleep). -G = Grandiosity (which means the patient overestimates his or her self worth or capabilities). -F = Flight of ideas (which is exhibited as the patient having racing thoughts). -A = Activity level increased. -S = Sexual indiscretions (which is exhibited as excess involvement in pleasurable activities). -T = Talkative (which is exhibited as fast speech). -Diagnostic Criteria Include: -Persistently elevated, expansive, and irritable mood lasting for at least 1 week. (This time period definition can be reduced to less than one week if the manic episode required hospitalization). -Three or more of the following symptoms must be present during this period: -Decreased need for sleep. -Racing thoughts. -Distractibility. -Psychomotor agitation. -Pressured speech. -Inflated self-worth. -Excessive involvement in pleasurable activities, such as sex. -Additional criteria include: -The disorder causes significant impairment in social and or occupational function, is severe enough to require hospitalization, or is present with psychotic features. -The disorder is not due to a medical condition or substance abuse. -Medications the patient may be taking include: -Lithium (trade name Eskalith®), which is one of the most commonly prescribed medications for bipolar disorder. -Valproic Acid (trade name Depakote®). -Carbamazepine (trade name Tegretol®). Assessment and Management: -Protect yourself, the patient, and others. -Restrain the patient, if necessary, and per local protocol. -Maintain alertness. -Do not leave the patient alone. -Avoid confrontation, especially if the patient is acutely manic. -Be supportive and calm. -Assess and stabilize the ABCs. -Obtain a SAMPLE history and head to toe physical exam. -See the “Assessment and Management” sections of this course for further details. -Determine the suicide risk. -Manage co-existing medical and or traumatic conditions. -Administer medications, such as haloperidol, if the patient is overtly psychotic. Be sure to consult medical direction. Description: Anxiety is defined as a feeling of uneasiness or a sense of threat about impending problems. It is one of the most common emotions that humans experience. Anxiety becomes a disorder when fears and apprehension dominate psychological life. Panic Disorder: -Definition: -Panic disorder is defined as recurrent attacks of sudden anxiety resulting in great emotional distress. -These attacks can be either unprovoked or related to a particular stimulus. -Signs and symptoms have rapid onset and dissipate in less than an hour. -Other Characteristics: -Patients often feel that they are suffering from a serious medical condition. -Patients often have marked anxiety about future attacks. -Depression occurs in over half of patients. -Patients have an increased risk of suicide. -Epidemiology: -The point prevalence of panic disorder (at any one point in time) = 7.3%. -Panic disorder occurs more frequently in women. -It develops in early adulthood and has a peak onset in the mid-twenties.7 -About 60% of patients with panic attacks seek care. 32% of these patients present to the ED.9 -Signs and Symptoms Include: -Feelings of intense fear and tension. -Feelings of chest tightness and shortness of breath. -Hyperventilation, which can lead to paresthesias (numbness or tingling). -Palpitations, tachycardia, and feeling like one’s heart is jumping out of one’s chest. -Sweating. -Dizziness or lightheadedness. -Tremors. -Fear of dying or losing control. ****NOTE: Panic disorder mimics a wide variety of medical conditions. Helpful clues to narrow your list of concerns are to consider the patient’s history of anxiety and psychiatric conditions, as well as the particular age of the patient. -Diagnostic Criteria Include: -A discrete period of fear or discomfort with at least four of the following: -Palpitations or tachycardia. -Trembling. -Sweating. -Dizziness or unsteadiness. -Chest pain or discomfort. -Choking sensation. -Nausea or abdominal distress. -Shortness of breath. -Chills or hot flashes. -Fear of losing control. -Fear of dying. -Paresthesia (numbness or tingling). -Derealization or depersonalization. -Additional criteria include: -The person must have been concerned about having additional attacks for at least a month after the initial episode. -The episodes must not be caused by another mental disorder. -The disorder is not due to a medical condition or substance abuse. -Management: -Assess the patient for medical or traumatic causes. -Support and reassure the patient. -Calm the patient to help decrease his or her respiratory rate, if the patient is hyperventilating. -Administer medications, per medical direction orders, including: -Benzodiazepines (such as, diazepam and lorazepam) to help calm the patient. -Antihistamines for sedation (such as, diphenhydramine and hydroxyzine). -Medications the patient may be taking include: -Antidepressants, such as: -Paroxetine (trade name Paxil®). -Zoloft (trade name Sertraline®). -Some patients may also be on benzodiazepines, such as: -Alprazolam (trade name Xanax®). -Diazepam (trade name Valium®). -Lorazepam (trade name Ativan®). -Oxazepam (trade name Serax®). Specific Phobia Disorder: -Definition: -Specific phobia disorder is an exaggerated, disabling, irrational fear about the presence or anticipation of a specific situation or object. -Exposure to the stimulus will induce an immediate panic attack. -Common Phobias Include: -Agoraphobia, which is fear of crowds. -Acrophobia, which is fear of heights. -Aerophobia, which is fear of flying. -Arachnophobia, which is fear of spiders. -Claustrophobia, which is fear of being trapped in small spaces. -Epidemiology: -Specific phobia disorder is the most common psychiatric disorder.7 -It occurs in 25% of the population at some time in a person’s life. -It is more prevalent in women than men. -Signs and Symptoms Include: -Tenseness. -Restlessness. -Tremors. -Tachycardia or palpitations. -Difficulty breathing. -Sweating. -Diagnostic Criteria: -Persistent excessive fear caused by the presence or anticipation of a specific situation or object. -The patient recognizes that the fear is excessive. -The patient goes to great lengths to avoid the stimulus. -The distress caused by the stimulus, or the measures that the patient takes to avoid the stimulus, cause marked impairment. -The condition is not caused by another mental disorder. -Management: -Support and reassure the patient. -Manage underlying conditions. -Do not force the patient to do anything he or she does not wish to do. Post-Traumatic Stress Disorder: -Description: -Post-traumatic stress disorder is a type of anxiety disorder that results from a severe psychosocial event. -The event is typically life-threatening, such as rape, war, or a natural disaster. -This condition is characterized by hyperarousal (manifested as an exaggerated startle response), persistent re-experiencing of the event, and efforts to avoid recollection. -Epidemiology: -Post-traumatic stress disorder has a lifetime prevalence of 8%. -The prevalence of this disorder in assault victims and soldiers is 60%.6 -Signs and Symptoms Include: -Repetitive, intrusive memories. -Avoidance of reminders. -Poor impulse control. -Increased arousal/startle. -Depression. -Nightmares and sleep alterations. -Survivor guilt. -Additionally, this disorder is often complicated by substance abuse. -Diagnostic Criteria Include: -Persistent re-experiencing of an event through recollection, nightmares, or flashbacks. -Intense distress caused by reminders. -Increased arousal characterized by two of the following: 1) Insomnia. 2) Irritability 3) Hypervigilance. 4) Exaggerated startle response. 5) Poor concentration. -Three of the following: 1) Amnesia. 2) Decreased pleasure from activities. 3) Emotional numbing. 4) Active avoidance of reminders. 5) Restricted affect. -Symptoms must be present for at least one month. -Management Considerations: -Show respect. -Support and protect the patient. -Medications the patient may be taking: -Tricyclic Antidepressants, such as: -Desipramine (trade name Norpramin®). -Nortriptyline (trade name Pamelor®). -Amitriptyline (trade name Elavil®). -Imipramine (trade name Tofranil®). -Clomipramine (trade name Anafranil®). -Monoamine Oxidase Inhibitors, such as: -Isocarboxazid (trade name Marplan®). -Phenelzine (trade name Nardil®). -Tranylcypromine (trade name Parnate®). -SSRI Antidepressants, such as: -Paroxetine (trade name Paxil®). -Zoloft (trade name Sertraline®). -Some patients may also be on benzodiazepines, such as: -Alprazolam (trade name Xanax®). -Diazepam (trade name Valium®). -Lorazepam (trade name Ativan®). -Oxazepam (trade name Serax®). Description: Eating disorders are characterized by a preoccupation with body image and size, as well as abnormal eating behaviors. Eating disorders include: anorexia nervosa and bulimia nervosa. Anorexia Nervosa: -Characteristics Include: -Excessive fasting. -Intense fear of become being fat or gaining weight. -Refusal to maintain weight above 85% for age. -Preoccupation with body size and shape. -The patient often denies the seriousness of his or her current low weight. -Additionally, anorexia nervosa is frequently associated with menstrual cycle disturbances. -Epidemiology: -Anorexia nervosa has a 0.5% to 1.0% prevalence in females. -90% of cases occur in females. -The lifetime mortality for anorexia nervosa is around 10%.6,7 Bulimia Nervosa: -Characteristics: -Unlike anorexia nervosa, patients are typically at or above their expected weight. -Bulimia nervosa is characterized by recurrent episodes of binge eating, with purging. -Binging is characterized by a sense of lack of control over eating. -Purging is recurrent behavior to avoid weight gain, such as excessive exercise, or induction of vomiting and diarrhea. -The person is aware of his or her behavior. -These patients also tend to be perfectionists. -Epidemiology: -Bulimia nervosa has a 1% to 3% point prevalence in females. -It has a 0.1% to 0.3% prevalence in males.6,7 Management: -Support and reassure the patient. -Manage dehydration and other physical problems. Other Considerations: -Patients may suffer from anemia, hypoglycemia, esophageal rupture, arrhythmias, and other medical complications. Description: Personality disorders are chronic, fixed maladaptive patterns of behavior, stemming from immature personality development. Cluster A – Odd and Eccentric Personality Disorders: -Description: -These individuals prefer social isolation. -Types: -Paranoid Personality Disorder: Is characterized by pervasive distrust and suspicion of others. -Schizoid Personality Disorder: Is characterized by a lack of desire for or joy from close relationships, as well as diminished affect and emotional detachment. -Schizotypal Personality Disorder: Is characterized by eccentric behavior and acute discomfort in close relationships. Cluster B – Dramatic and Erratic Personality Disorders: -Description: -These patients tend to be very disruptive. -Types: -Antisocial Personality Disorder: Is characterized by disregard for the rights of others. -Borderline Personality Disorder: Is characterized by instability, impulsivity, and poor selfimage. -Histrionic Personality Disorder: Is characterized by excessive emotion and attention seeking. -Narcissistic Personality Disorder: Is characterized by pervasive feelings of grandiosity and a need for admiration. Cluster C – Anxious and Fearful Personality Disorders: -Types: -Avoidant Personality Disorder: Is a pattern of social inhibition characterized by avoidance of social relationships due to feelings of hypersensitivity. -Dependent Personality Disorder: Is characterized by submissive, clingy behavior, and excessive need to be cared for. -Obsessive-Compulsive Personality Disorder: Is characterized by a preoccupation with orderliness and perfection. Introduction: Cognitive disorders are psychiatric conditions that result from biologic causes, including: metabolic derangements, endocrine diseases, degenerative neurologic processes, infections, drug abuse, drug reactions, neoplasms, trauma, and cardiopulmonary diseases. Cognition is defined as mental activities pertaining to learning, memory, and thinking. Delirium: -Definition: Delirium is an acute transient disturbance in consciousness accompanied by decreased cognition (memory, perception) and decreased attention that is caused by an identifiable precipitant. -Characteristics Include: -Decreased concentration and disorientation. -Rapid onset (hours to days). -Fluctuates (periods of normal function interspersed with confusion). -Patient illusions or hallucinations (most commonly visual). -Clouding of consciousness. -Short term memory is altered, while long term memory is typically preserved. -The cause is a medical condition and or substance use or withdrawal. -Symptoms may be worse at night time, known as “sundowning.” -Common Causes Include: -Infection. -Metabolic derangements, such as hypoglycemia, hypoxia, and hypercarbia. -Post-surgery. -Post-seizure. -Head trauma. -Significant pre-existing psychiatric condition. -Substance abuse or withdrawal. -Recognize that medication intoxication is the most common cause, with anticholinergic-like drugs being the most common category of medications causing delirium. Dementia: -Definition: Dementia is a potentially irreversible state of mental dysfunction characterized by memory impairment and other cognitive deficits. -Characteristics Include: -Patient alertness, with no alterations in level of consciousness. -Stable, slow, downhill course. -Slow onset (weeks to years). -Pervasive disturbance in judgment and abstract thinking in the patient. -Causes significant social and occupational impairment. -Patients may have delusions and hallucinations. -Patients may also display: -Aphasia (which is the inability to verbalize). -Apraxia (which is the inability to carry out purposeful movement). -Agnosia (which is a failure to recognize objects). -Disturbances in executive functioning. -Types of Dementia Include: -Alzheimer’s, which is the most common. -Vascular, which is the second most common, and is caused by multiple “mini-strokes.” -AIDS. -Parkinson’s. -Head trauma. Assessment and Management: -Protect yourself, the patient, and others. -Restrain the patient, if necessary, and per local protocol. -Maintain alertness. -Maintain a quiet, well lit, comfortable environment. -Assess and stabilize the ABCs. -Obtain a SAMPLE history and head to toe physical exam. ***Be sure to identify: -The baseline level of function of the patient. -The time frame of symptom onset. -The progression over 24 hours. -The patient’s level of cognition. Are thoughts coherent? Is the patient able to pay attention? -The patient’s level of consciousness. -Determine the patient’s suicide risk. -Manage co-existing medical and or traumatic conditions. -See the “Assessment and Management” sections of this course for further details. Other Concerns: -Patients are often unable to give informed consent. -Patients may display aggressive behavior. -Patients are at risk for falls and self injury. Introduction: All patients with psychiatric or behavioral conditions should be screened for substance use or abuse. Drug users may be ill from intoxication, addiction, or withdrawal. Refer to the Medic-CE Toxicology Series for further details on the assessment and management of substance abuse patients. Basic Definitions: -Addiction: Is an overwhelming dependence on a substance. -Intoxication: Is a reversible syndrome following ingestion of a substance that causes significant maladaptive changes. -Overdose: Refers to poisoning as a result of taking an excessive dose of a drug, whether legal or illegal. -Withdrawal: Is the development of symptoms following abrupt cessation of use of a drug in a habituated individual. Withdrawal symptoms act as reinforcement for continued abuse. Signs and symptoms include: altered CNS function, shaking, sweating, and vital sign instability. Substance Abuse: -Substance abuse is defined as use of an illicit drug, or excessive non-medical use of a licit drug. -It is a maladaptive pattern of substance use that may lead to significant impairment or distress as manifested by the following: 1) Failure to fulfill responsibilities at home, school, or work. 2) Recurrent legal problems related to the substance. 3) Recurrent substance use in physically hazardous situations. 4) Recurrent substance use despite persistent social or interpersonal problems related to the effects of the substance. Substance Dependence: -Substance dependence is a maladaptive pattern of substance use that involves certain physiologic, behavioral, and cognitive changes. -Substance dependence is characterized by at least three of the following symptoms occurring in a 12 month period: 1) Withdrawal. 2) Tolerance. 3) Repeated, failed efforts to cut down. 4) Excessive time spent trying to procure the substance. 5) Repeated, unintended, and or excessive use. 6) Reduction in important recreational, occupational, and or social activities. 7) Continued use of a substance despite awareness of adverse consequences, such as legal, health, interpersonal, or work-related problems. ***NOTE: “Dependence” involves tolerance and or withdrawal. Physical Addiction: -Physical addiction involves adaptation of the body to a substance. With physical addiction, a person undergoes physiologic changes that require the drug to be present in order to prevent the development of the withdrawal syndrome. -The following are important principles related to physical addiction. 1) Withdrawal from long-acting drugs is relatively mild and of longer duration. 2) Withdrawal from short-acting drugs is more intense and of a more rapid duration. 3) Different drugs within a same class can maintain the same physical dependence. That is why methadone can be used as a substitute for heroin or morphine dependence. Psychological Dependence: -Psychological dependence is characterized by an intense craving for a substance and drugseeking behavior. -Psychological dependence is reinforced by feelings of euphoria and well-being. -A person who is psychologically dependent is preoccupied with procurement of the substance. However, there are no consequences of withdrawal with psychological dependence. Somatoform Disorders: -Somatoform disorders are characterized by a patient experiencing physical symptoms with no apparent cause. -Additionally, a patient has false and bizarre beliefs about his or her body. -Somatization Disorder: -These patients are typically preoccupied with many physical symptoms. -The symptoms have no organic cause or are in excess of what is expected by a medical evaluation. -Additionally, the symptoms are not intentionally produced. -Conversion Disorder: -These patients complain of loss of sensory or motor function. -The symptoms cannot be explained by a medical illness. -The symptoms typically occur in close proximity to a significantly stressful event (i.e. death of a loved one leads to psychogenic paralysis). -Additionally, the symptoms are not intentionally produced. -Hypochondriasis Disorder: -This disorder is characterized by a preoccupation with one’s health. -These patient’s have an exaggerated fear of having a serious disease based on misinterpretation of symptoms. Factitious Disorder: -Description: -Factitious disorder is characterized by the intentional production of a physical or psychological symptom. -Patients are motivated by wanting to assume the “sick role.” -External incentives for behavior, such as financial gain are absent. -Patients typically have knowledge of medical terms and can be convincing, demanding, and disruptive. -You may have heard of Munchausen’s syndrome, which is factitious disorder with predominantly physical symptoms. Dissociative Disorders: -Description: -These are a group of disorders characterized by loss of memory of self and division of consciousness and personality into separate parts. -These patients subconsciously avoid stress by dissociating from self. -These disorders involve very complex patterns of behavior and are, fortunately, extremely rare. -Characteristics: -Amnesia, which is the inability to recall past events. -Psychogenic amnesia, which is the failure to recall. -Fugue, which occurs when a person travels far away and assumes a new identity. -Multiple personalities. -Depersonalization, which is when a person loses sense of self. Impulse Control Disorders: -Description: -These disorders are characterized by recurrent impulses with the patient’s failure to control them. Patients typically have a lack of concern for consequences. -Types: -Pathologic gambling, which is a chronic preoccupation with gambling. -Trichotillomania, which is a recurrent chronic urge to pull out one’s hair. Characteristics: -Suicide is the willful act of taking one’s life. -Many people make last minute attempts to communicate their intentions. -The vast majority of people who commit suicide suffer from mental illness or substance abuse. Epidemiology: -Suicide is the eleventh leading cause of death in the United States.10,11 -More Americans die from suicide than homicide each year.12 -More than 1500 Americans attempt suicide each day and around 86 people actually succeed. -Self-inflicted injury and suicide attempts account for 0.4% of all ED visits. -400,000 to 500,000 ED visits per year. -The most common method of suicide attempt or self-inflicted injury identified by the Doshi et al. study in 2005 is poisoning (at 68%), followed by cutting or piercing (at 20%).5 -The most common method for completing suicide is with firearms.10,11 -The ratio of attempted to completed suicides in the general population is 8:1.5 -The ratio of attempted to completed suicides among the elderly is 4:1.13 -Between 40% and 60% of individuals who die by suicide are intoxicated at the time of death.5 -Women attempt more suicides, typically with less lethal methods, such as overdose, wrist slashing, or drowning. Risk Factors for Suicide Include: -A history of substance abuse. -A history of mental illness. -A history of psychiatric treatment. -Lack of social support, such as living alone or being unmarried. -A patient’s first degree relative has committed suicide. -Financial difficulties. -Recent humiliation. -Recent loss of a loved one. -Physical illness. -Lack of plans for the future. -Collecting materials or weapons with which to harm one’s self. -Previous history of self-harm or suicide attempts. -Expressed suicidal thoughts or gestures. -Hopelessness, which is one of the most reliable long-term risk factors. -Age: The risk increases with age. -For men, incidence peaks after 45. -For women, the incidence peaks after 55. -Race: Caucasians, Native Americans, and Alaskan Natives are at higher risk for completing suicide. Assessment and Management: -Most suicide attempts will be self-evident, either because of physical evidence or because of information from the patient or bystanders. -A patient with a behavioral or psychiatric emergency should be asked if he or she has had thoughts about harming himself or herself or taking his or her life. -A person who attempts suicide, whatever the motive, has a real problem that needs help or treatment. -Perform a focused history and physical exam while providing psychological care. -Detailed care and observations at the scene are critical to the patient’s long-term care. -Carefully document observations and information obtained from the patient and bystanders. Focus on identifying suicide plans, triggering factors, and specific details of actions taken. -The details of the suicide attempt are essential in understanding future risk. -All patients should be transported for evaluation. -Do not deny that an attempt occurred so as not to belittle the patient’s feelings. -Do not argue with a patient or challenge a patient to commit suicide. -See the “Assessment and Management” sections of this course for additional details. What you can do – The Surgeon General’s Call to Action – AIM to Prevent Suicide: -Awareness: You can broaden the public’s awareness of suicide and its risk factors by: 1) Promoting public awareness that suicide is a major public health problem and that many suicides are preventable. 2) Expanding awareness of community resources for suicide prevention programs, as well as mental health and substance abuse treatment programs. 3) Reducing the stigma associated with mental illness, substance abuse, and suicidal behavior, as well as the stigma associated with seeking help for such problems. -Intervention: You can help enhance services and programs by: 1) Implementing proper training for health professionals concerning suicide risk assessment, recognition, management, and aftercare. 2) Implementing effective training programs for family members of those at risk and for community helpers on how to recognize, respond to, and refer people exhibiting signs of suicide risk and associated mental health or substance abuse disorders. 3) For the young members of the population, develop programs that address adolescent distress, provide crisis intervention, and incorporate peer support for seeking help. -Methodology: You can help advance the science of suicide prevention by: 1) Enhancing research to understand risk and protective factors related to suicide. 2) Increasing research on effective suicide prevention programs, clinical treatments, and culture-specific interventions. 3) Encouraging the development and evaluation of new prevention technologies, such as firearm safety measures, to reduce easy access to particularly lethal means.12 Legal Considerations of Patient Management: Some patients may have been trying to commit suicide, but will pretend that they were just kidding when you arrive. If you leave a patient, and the patient does something to himself or herself, then you may be charged with patient abandonment. At the same time, you cannot force the patient into treatment. In either case, it is important to involve law enforcement personnel in these situations. Characteristics: Agitation is defined as excessive restlessness associated with mental illness. Violence is an act of physical force exerted for the purpose of causing damage. Agitation or violence can be caused by psychosis, mania, alcohol or drug intoxication, head injury, fear, and panic. Additionally, conditions such as hypoxia, hypoglycemia, and acute stroke may present as confusion and combativeness. Typical signs include: nervous pacing, threatening acts, shouting, cursing, clenched fists, muscle tension, and clenched teeth. Verbal aggression is one of the most common manifestations of violent behavior. Addressing agitation early goes a long way to impacting patient care, caregiver burden, and community resources. Epidemiology: -0.8% to 5.0% of incidents to which EMS personnel respond involve violence.14,15 -Psychiatric ED visits potentially involving agitation approach 1.7 million annually.17 Factors Associated with Increased Risk of Violent Behavior Include: -Male sex. -Substance abuse. -Age (late teens to 20s). -History of violence. -Hostility during the patient interview. -Hallucinations and or delusions. -Lack of insight into delusions. -Depression. -Suicidal tendency. -Low intelligence. -Impulsivity. -Psychosis, acute mania, and dementia. Assessment and Management: -Determine the risk of violence by: -Performing a scene size-up. -Determining the patient’s history of aggression. -Analyzing the patient’s posture. Pay attention to clenched fists and the patient holding lethal objects. -Analyzing the patient’s tone of voice and verbal threats. -Analyzing the patient’s physical activity for quick irregular movements and tense muscles. -See the “Assessment and Management” sections of this course for further details. ****NOTE: It is not possible to predict with certainty which patients will be physically violent. Patient Assessment Step 1 – The Scene Size-up: -Safety: Avoid becoming a victim. 1) Pay close attention to dispatch information. Ask about the potential for violence, and whether police are on the scene. -Most significant behavioral emergencies will have law enforcement personnel dispatched. 2) Survey the scene to determine the risk of an unsafe situation. -High risk scenes involve behavioral emergencies, drugs and alcohol, or domestic violence. -Assess for environmental hazards that may be present, such as from the mechanism of the suicide attempt (i.e. a running car in a garage or a gas stove that has been left on). 3) If you cannot guarantee your own safety, call law enforcement and wait for their arrival. 4) Do not enter a scene unless you can visually locate the patient. 5) Never turn your back on a patient. 6) Scan the scene for objects that the patient can use to harm self or others. If a weapon is present, calmly tell the patient that you cannot help him or her, unless the weapon is released. If the patient does not release the weapon, exit the scene and call the police. 7) Always have an exit route. -Scene Assessment: -Scan the scene for information to assist with assessment and care. Look for: -Evidence of trauma or violence. -Evidence of substance abuse. -Evidence of psychiatric medications the patient may be taking. -Evidence of contributing environmental conditions. -Evidence of medical conditions. -Additionally, survey the scene to determine if there are other patients needing care, such as in multiple suicide or murder-suicide incidents. Patient Assessment Step 2 – The Initial Assessment: -Safety: -Limit crowds around the patient. -Maintain alertness to danger. -Observe Standard Precautions, paying particular attention to appropriate body substance isolation techniques and to wearing necessary protective gear. -Primary Survey: -Assess and stabilize the ABCs. -Assess for life threatening conditions. Many behavioral emergencies are caused by or occur with medical conditions or trauma. -Impression: -Psychiatric disorders manifest in three realms – by disturbances in emotion, behavior, and or cognition. -Form a rapid impression, based on the patient’s activity level, level of thinking, and responsiveness. -Observe affect and body language. -Note evidence of altered behavior, such as rage, depression, anxiety, confusion, or fear. -Determine if the patient is cooperative or uncooperative. -Determine if the patient is a threat to self or others. -If the patient has attempted suicide, care for medical or traumatic issues before addressing behavioral concerns. See the Medic-CE Toxicology Series for specific assessment and treatment options for suicide attempts by toxic ingestion. ****NOTE: All patients who have attempted suicide should be transported. Patient Assessment Step 3 – The Focused Assessment: -Begin by creating a comfortable environment: 1) Establish patient rapport. 2) Remove the patient from a disturbing situation. -Then proceed with the patient history and physical exam. -The Patient History: Perform a complete SAMPLE history if the patient is alert and without injury. Concentrate on the following: 1) Identify the chief complaint: Ask the patient, “What’s going on?”, “What’s the trouble?”, or “What’s bothering you?” This may not be answered explicitly, but can be obtained by observing the patient and listening to what he or she says. Use open-ended questions. The critical information will usually emerge in the first couple of minutes, if you allow the patient to speak. 2) Determine which medications the patient has been taking: It is very important to assess compliance with medications. Identify if there has been a recent change in the patient’s medication regimen. Identify both prescription and non-prescription medications. 3) Identify any contributing medical conditions, such as: HIV, substance abuse, diabetes, cardiovascular disease, neurologic disease, etc. 4) Determine if the patient has a history of psychiatric illness: Is the patient seeing a mental health professional? Has the patient ever been hospitalized for a mental health problem? Is the patient on psychiatric medications? 5) Identify a history of events immediately prior to the incident: Try to identify any possible triggering events for the patient’s condition, such as the loss of a loved one, loss of job, etc. 6) Identify baseline functioning: Attempt to identify the patient’s baseline level of mental and physical health prior to the incident. -Additional Questions to Ask: -Did the patient ingest alcohol or drugs? -Does the patient want to harm him/herself? -Has the patient ever been violent or aggressive? -Has the patient’s mood changed recently? -Has the patient been upset, irritable, or nervous? -Has the patient had any weird, recurrent thoughts? -Has the patient been using any substances or medications to help him or her cope? -The Physical Exam: Inspect the patient from head to toe for evidence of trauma or medical illness. -Head: Identify any evidence of head trauma. -Eyes: Are the pupils dilated or pin-point? -Neck: Is the neck stiff and painful, or supple? -Chest: Does the patient have any lung crackles? Is the patient in respiratory distress? -Abdomen: Is the abdomen distended or tender? -Neurologic Exam: Identify any numbness, weakness, or other neurologic deficits. -Other: -Obtain vital signs. -Assess the patient’s blood glucose level. ****NOTES: -If the patient is severely altered or has a medical illness or traumatic injury, perform a rapid assessment from head to toe, obtain vital signs, and then obtain a SAMPLE history. -The patient may be unable or unwilling to provide information. In these cases, obtain pertinent information from friends, bystanders, and police, where possible. Patient Assessment Step 4 – Carefully Document Findings: -Documentation is one of the most critical components of patient care. This is especially true with behavioral emergencies. -Important items to include in documentation: 1) Physical complaints and injuries. 2) The patient’s mental status, including: -The patient’s intellectual function, focusing on: -Orientation, concentration, judgment, and memory. -The patient’s thought content, focusing on: -Disordered thoughts. -Delusions and or hallucinations. -Worries and or fears. -The patient’s language, focusing on: -Speech pattern and content. -Is it garbled or unintelligible? -The patient’s mood, focusing on: -Anxiety, depression, elation, and or agitation. -Additionally, document the patient’s: -Level of alertness. -Psychomotor activity. -Appearance and hygiene. 3) Witness signatures. 4) A description of interventions performed and any complications from interventions. 5) A description of radical behavioral alterations. Appearance/Behavior: -Assess the level of grooming and hygiene. -Assess the patient’s body language. -Assess the patient’s psychomotor activity: -Is the patient agitated and fidgeting? -Is the patient very lethargic? Does the patient have slow movements? Cognitive Ability: -Assess the patient’s level of consciousness. -Assess Orientation: -Does the patient know who he or she is? Who others are? -Does the patient know where he or she is? -Does the patient know what time it is? -Assess Memory: -Is the patient’s memory intact? Can the patient remember things you tell him or her? Can the patient remember things in the distant past? -Assess Concentration: -Is the patient able to concentrate? Is the patient able to remember events or what he or she said? Mood: -Is the patient’s mood appropriate? -Is the patient angry, confused, withdrawn, irritable, crying, anxious, or fearful? -Identify the patient’s level of alertness and distractibility? Speech: -Assess the rate, tone, and volume of the patient’s speech. Thought: -Thought Processes: How is the patient thinking? -Does the patient make unusual associations? -Do the patient’s thoughts flow logically, or do the patient’s thoughts jump around? -Does the patient answer questions directly? -Thought Content: What is the patient thinking? -Identify suicidal or violent thoughts. Perception: -Has the patient seen or heard things that others could not? -Has the patient had any strange feelings, such as out-of-body experiences? Judgment: -Is the patient making rational choices? Assess the patient’s history of decision making. Insight: -Does the patient understand his or her current condition and its implications? Impulse Control: -Ask if the patient has ever felt like he or she was going to lose control, or hurt someone, or himself or herself. Identify what the patient wanted to do, and if he or she actually did it. Signs and Symptoms of Behavioral Emergencies Include: -Tension, crying, irritability, loss of appetite, and loss of sex drive. -Loss of contact with reality – hallucinations. -Mania. -Depression. -Social withdrawal. -Intoxication or withdrawal symptoms. -Anger. -Confusion. -Fear. -Anxiety. Key Distinguishing Characteristics of Medical Conditions: -An alcohol odor on the breath can represent a diabetic emergency instead of actual alcohol. -Physical problems typically develop more quickly, whereas behavioral or psychiatric conditions develop over time. -Visual hallucinations are typical of physical illness, whereas auditory hallucinations are more common for psychological illness. -Physical conditions result in memory loss, whereas memory is intact in behavioral problems. -Consciousness is usually altered with organic causes. -The physical exam will be mostly normal in a psychiatric condition. -Pupil changes occur with physical conditions, such as intoxication. -Urinary incontinence is present with medical conditions. ****NOTE: Physical trauma or illness may be co-existent with behavioral issues. Geriatric Patients: -Assess the patient’s ability to communicate. -Provide reassurance. -Be aware of deficiencies in eye sight or hearing. -Treat the patient with respect by using the patient’s last name. -Describe all steps you plan to take. -Give the patient the impression that you are going to take your time and are not in a hurry. -Allow friends and family to remain with the patient. -Understand that the majority of conditions presenting as psychiatric emergencies in the elderly stem from an underlying organic cause. -Avoid administering medications. Pediatric Patients: -Try to keep the child near a parent. -Decrease stressful stimuli. -Be clear and simple with explanations. -Speak calmly and slowly. -Clearly identify yourself. -Engage the child to participate in his or her care. -Reassure the child. -Allow the child to display emotions. -Allow the child to keep comforting possessions, such as a blanket. -Do not leave the child alone. Introduction: The way you conduct an assessment establishes rapport with the patient and is part of the care you provide. Intangibles of personal interaction make the difference with helping the patient. ****KEY POINT: The way you carry yourself and speak are of the utmost importance. Basic Principles of Talking to a Patient: -Everyone has limitations. -Every patient has a right to his or her feelings. -Each person has some strength remaining to cope with his or her crisis. -Emotional injury is real. -Results may not be instant. Your role is to provide a good beginning. -Cultural differences are important. Understand where your patient is coming from. The Assessment Environment: -The effectiveness of an evaluation depends on the patient feeling both understood and safe. -It may be necessary to modify the interview environment to accommodate the patient’s mental state. -If the patient is agitated, maintain a comfortable distance and carefully structure the interview. Make slow purposeful movements. -If the patient is disconnected, actively engage him or her. Speak slowly, clearly, and with purpose. -Minimize distressing stimuli. -Never leave the patient alone. Once you respond to an emergency, you are legally responsible for the patient. Questioning: -Introduce yourself and say you are there to help. -Place yourself at eye level with the patient. -Appear calm, comfortable, and in control. -Determine the chief complaint, and then focus on that complaint. -Acknowledge the patient’s feelings. -Try to convince the patient to cooperate through speech. Be an active listener, by repeating what the patient says. -Limit interruptions. -Pay attention. -Be supportive. -Treat the patient with respect. -Use terms the patient uses. -Never appear judgmental. -Avoid arguing. -Never lie. -Do not belittle the patient’s problem. -Do not reinforce false beliefs. -Limit physical touching. -Avoid threatening actions or statements. -Avoid asking why. -Make slow purposeful movements. Avoid making the patient feel rushed. -Inform the patient of everything you do. Explain what might be going on to the patient. -Show respect and do not make assumptions. -Allow the patient to talk. -Ask open-ended questions – those that cannot be answered with a simple yes or no. -Be prepared to stick around for a long time. Preparation: -Ensure your own safety. -Call for back-up, if necessary. -Restrain the patient, if necessary (per local protocol and or medical direction or law enforcement orders). See “Management” sections below. -Observe appropriate Standard Precautions. Initial Management: -Establish spinal immobilization, if injury is suspected. -Stabilize the ABCs: -Secure the airway, if the patient is unresponsive or without a cough or gag reflex. Suction as necessary. -Administer oxygen via non-rebreather mask, if ventilations are adequate. -Assist ventilations with supplemental oxygen and positive pressure ventilations, if ventilations are inadequate. -Assess the patient’s pulse. If pulseless, follow AED protocol. -Manage any medical conditions or injuries. -Violence or agitation can sometimes be caused by reversible medical conditions, such as intoxication, hypoxia, and hypoglycemia. -Naloxone, oxygen, and dextrose, respectively, can be used to treat the underlying condition and calm the agitated patient. Ongoing Management: -Keep the patient calm and maintain normothermia. -Never leave the patient alone, or turn your back on a patient. -Transport the patient to an appropriate facility for physical and psychological treatment. Bring any ingested substances that may be the cause of the patient’s condition. -Perform a detailed exam en route. Continue to calm and reassure the patient. ****NOTE: If the patient becomes violent or threatens to injure him or herself or others, apply patient restraint techniques (including: verbal, physical, and chemical restraint). Begin with the least restrictive method that assures the safety of the patient and healthcare personnel. Introduction: Initial management should focus on non-physical interventions to calm the patient and make the patient receptive to evaluation and treatment. ****NOTE: Not all patients will benefit from verbal restraint, as they may be too agitated to understand your motives. Environmental Modifications: -Decrease external stimuli through relative isolation. -Minimize waiting time. -Remove potentially dangerous objects. -Assure a physically comfortable setting. -Have an escape route for yourself and the patient. -If you wear a badge, remove it prior to approaching the patient to avoid being confused with a law enforcement officer. Verbal De-Escalation (”Talking the Patient Down”): (1) Establish Rapport: -Convey empathy and authenticity. -Useful phrases include: “I understand you are not feeling well,” or “It sounds like you are having a hard time.” -The conversation should have a friendly tone. -Appear non-judgmental and neutral. -Reassure the patient that he or she is in a protective setting. -Allow the patient to express feelings and thoughts with words. -Respect the patient’s personal space. -Remain at the patient’s eye level. -Refrain from intense, direct eye contact. -Avoid confrontational body language. Try to keep your arms uncrossed, hands off hips, and hands in view of the patient. -Have a family member present, if the patient would feel more comfortable. However, be careful not to violate confidentiality. Also, use caution when bringing a family member into a dangerous situation. (2) Verbal Re-Direction: -Appear calm and in control. -Place limits on the patient’s behavior. Inform the patient of the consequences of any actions that he or she may take. The patient should be told that he or she will not be able to harm others or him or herself. -Positive reinforcement should be provided. -Show concern for the patient’s well-being. -Assure the patient that he or she is safe from harm. “Don’t be afraid, we are here to help you.” -Negotiate and appeal to reason. Further Management: -If the patient is not responding to verbal redirection it may be necessary to have a “show of force” and or offer the patient voluntary tranquilizing medication. -If this fails, physical restraints and involuntary medication are needed. -Consult medical direction and call for back up, if necessary. ****Note: This technique should be avoided unless the patient is a danger to self and or others.**** Potential Indications: 1) If no one can communicate with the patient, and the patient is a danger to self or others. 2) If verbal interventions have failed to eliminate the potential danger that a patient poses to him/herself and or others. 3) If the patient refuses voluntary tranquilization and continues to pose a threat to self and or others. 4) If local protocol and state statutes permit patient restraint. Benefits: -Properly applied patient restraint procedures may reduce the possibility of patient injury, can reduce the risk of injury to EMS providers, and can allow for timely assessment and management. Important Notes: 1) Restraints may require police and or medical direction authorization. If you are not authorized to use restraints, wait for someone who is. 2) If you must place the patient in a face down (prone) position, do so for as short a period of time as possible. -Some studies have shown that prone restraint may place the patient at increased risk for inadequate ventilation, hypoxia, and acidosis.17 -Hypoxia and acidosis can lead to agitation, confusion, and aggression. -Airway assessment and management becomes more difficult in the prone position. 3) If aspiration is a concern, place the patient in the lateral position. 4) Restrain the patient in the supine position. If you become concerned about excessive upper extremity movement, place the patient’s arms over his or her head, and restrain the patient’s wrists to the head of the stretcher. 5) Do not “hogtie” the patient. -“Hogtie” = Placing the patient face down with all extremities tied behind the patient. 6) Do not “sandwich” the patient such as between backboards or mattresses, as a form of restraint during transport. 7) EMS personnel should not use pepper spray, stun guns, mace, stun batons, or air tasers. Patient Restraint Technique: -Preparation: -Have police present and obtain medical direction consent, if possible and where applicable. -Have adequate help. -Plan what you are going to do. -Wear appropriate personal protective equipment. -Use padded restraints, such as cloth or gauze; leather may be used but is not as soft as the other two. -Considerations: -Use only enough force to achieve restraint. Do not harm the patient. -Physical restraints should be used in the least restrictive manner possible and for the least amount of time possible. -Procedure: -Stay beyond the patient’s reach until ready. -Act quickly when the decision is made. The key to effective restraint is to take the patient by surprise. -Have one person talk the patient through the restraining. -Patient restraint works best if approached with five people so that one person can control each limb, and a fifth person can manage the head. -Secure the patient to the stretcher with multiple straps – place straps around the extremities (wrists and ankles), chest, thighs, and waist. -Four-point restraints are preferred over two-point restraints. -Securing the legs, just above the knees, often prevents kicking more than restraint of the ankles. -Cover the patient’s face to prevent spitting. -Cervical collars may be applied to limit head mobility and prevent biting. ****NOTE: While gaining initial control, the patient may be temporarily restrained in the prone position. However, personnel must be vigilant for respiratory compromise. Additionally, the patient should immediately be moved to the supine position once the team has control of the patient. -After Care: -Perform a frequent and thorough reassessment of the patient. -Place the patient on the appropriate monitors, such as an EKG and pulse oximeter. -Reassess neurovascular status, especially where the patient is secured. -Reassess the airway, breathing, and circulation. -DO NOT remove restraints once applied. -Completely document the indications for and techniques of restraint. -Describe that other techniques had been used (verbal de-escalation, offer of voluntary tranquilization) and that the patient continued to pose a threat to him/herself and others. -Continue verbal defusing techniques. -The patient should be offered medication when restrained and, if the patient is still agitated, involuntary medication can be considered. Complications Include: -Strangulation, aspiration, impaired circulation, nerve damage, psychological injury, escape, spitting, injury to self, sudden cardiac death, and injury to others. ****NOTE: These complications can occur regardless of the restraint procedure, or patient positioning while restrained. Frequent monitoring is required. Factors Associated with Death in Restrained Patients: 1) Agitated delirium, which is a severe disturbance in the mental status that occurs over a relatively short period of time and is manifested by mental and physiological arousal, hostility, and excess sympathetic stimulation. This condition results from mental illness, substance abuse, or a combination of the two. 2) Hog-tie restraint. 3) Forceful struggle against restraint. 4) Prone positioning. 5) Stimulant use. 6) Chronic disease in the patient. 7) Obesity.17 Introduction: Chemical restraint is the administration of pharmacologic agents to decrease agitation. Typical protocols include a benzodiazepine or antipsychotic administered individually, or a combination of the two types of drugs. -Benzodiazepines: These medications have a relatively benign side effect profile. However, caution should be used to prevent over sedation, respiratory depression, and ataxia. You should be familiar with the particular benzodiazepine’s half-life and onset of action. -Lorazepam: Is one of the most widely used benzodiazepines because it has complete and rapid intramuscular absorption, an onset within 15 to 30 minutes after intramuscular administration, and a duration of action of 8 to 10 hours. -Midazolam: Has a short duration (1 to 2 hours) and can easily lead to the patient falling asleep. -Diazepam and Chlordiazepoxide: Both of these medications have erratic absorption rates and relatively long half-lives. -Clonazepam: Appears to have limited efficacy in agitation and has a relatively long half life (about 20 to 80 hours). -Antipsychotics: These medications can be used alone or in combination with benzodiazepines, especially when psychosis or mania is present. -Side effects include: 1) Extrapyramidal symptoms, such as dystonia and akathisia. -Dystonia is characterized by abnormal tone of the tissues, such as tense contraction of muscles. -Akathisia is a state of motor restlessness (inability to sit still) that may be confused with agitation. 2) Cardiac arrhythmias: -Thioridazine and droperidol increase the risk of cardiac arrhythmias. -The FDA has issued “black box” warnings of possible dysrhythmias associated with droperidol use (prolonged QT). -EKG monitoring is imperative when using these medications. 3) Neuroleptic malignant syndrome, which is characterized by hyperthermia with extrapyramidal symptoms that may result in death. -Haloperidol: Is one of the most widely used antipsychotics for agitation. It can be administered orally, IM, or IV. When administered IM or IV, the onset of action is 30 to 60 minutes, and the duration of effect is up to 24 hours. The onset of action for IV administration is relatively faster than IM. -Other Medications: -Diphenhydramine: Can be used prophylatically to calm the patient during transport between facilities. ****NOTE: Patients should NEVER be pharmacologically PARALYZED for the sole purpose of controlling agitation. Study by Cheney et al., 2006: -A 2006 study by Cheney et al., characterized assaults on EMS personnel by patients requiring restraint use. -The study found that: 1) Those who assault EMS personnel are more likely to be violent, arrested, female, and have injuries while under supervision. 2) Patients under the influence of drugs or alcohol were not more likely to assault EMS personnel, but were disproportionately more likely to be injured while restrained. 3) Reasons for restraint cited by personnel include: -To prevent EMS personnel injury (90% of respondents). -Verbal control was ineffective (84% of respondents). -To prevent patient injury (80% of respondents). -To facilitate assessment and treatment (63% of respondents). ****85% of restrained patients were perceived as being violent, combative, or as exhibiting anger/rage or homicidal behavior. 4) Law enforcement was present in 60% of cases, but the patient was under arrest in only 4% of cases. 5) Assaults occurred in 27% of cases. 6) Perceived need for chemical restraint was cited in cases of: -Assault to EMS personnel (53% of respondents). -Violent patients (24% of respondents). -Patients who were injured while under supervision (60% of respondents). 7) The need for chemical restraints was perceived to be greater in youths than adults and in none of the elderly patients. -Additionally, the article described that violence against EMS personnel is common. -The study concluded that physical restraint is a relatively safe procedure. Definitions: -Competence: Is a legal concept and is determined by the courts. -Capacity: Is determined by a physician based on standards used in the legal system. The patient must be able to understand the situation and the information presented to him or her. The patient must be able to make an informed decision. The patient must be able to appreciate the nature and consequences of, as well as alternatives to, the treatment options. Finally, the patient must be able to communicate that choice. -Consent: Is defined as permission to treat. -Informed Consent: Is defined as permission to treat that involves the patient understanding the treatment or intervention that is offered, the risks and benefits, and the consequences of and alternatives to the treatment that is offered. Informed Consent: -In every conscious, mentally competent adult, treatment must be explained thoroughly, including: its nature, potential effects, and the effect of no treatment. -A mentally competent adult has the right to determine whether or not he or she will be treated. -To be considered an adult an individual must be over the age of 18, in most states. -Furthermore, a person may be considered an adult if he or she is in the armed services, pregnant, a parent, or married. These individuals are technically known as “emancipated minors.” -If the patient is not an adult, or not mentally competent, consent must be obtained from a parent, blood-relative, or legal guardian. If such a person cannot be found, you can go ahead and treat on the grounds of implied consent. -Such determinations are difficult to make with behavioral emergencies; therefore, carefully follow local protocols and consult medical direction. -Treating a patient against his or her will, without consent, is considered assault and battery. Impaired Decision Making: -Typically, people with mental disorders, including intellectual disabilities, are more likely than the general population to experience impairments in their decision making capacity. -Realize that a person’s initial impairment in decision making may simply reflect the difficulties that a physically unwell or mentally distressed person may have in coping with the routine procedures for obtaining consent to treatment. Refusal of Treatment: -Emotionally disturbed patients will commonly refuse treatment. -If the patient is alert and oriented, he or she has the right to refuse treatment. -Document thoroughly all aspects of the encounter, complete a refusal of care form, and have it signed and witnessed by a police officer. Improving Patient Understanding: -Many patients may call for emergency help voluntarily, yet state that they intend to refuse treatment. A study by Jacob et al., 2005, found that an initial choice of refusal of treatment should not necessarily be considered as final, even when a person appears to make that decision with capacity. A patient may refuse treatment, yet be inwardly indecisive. -Effective strategies to gain patient consent may include presenting a simple information sheet accompanied with detailed verbal information. Medical Emergency Waiver of Informed Consent: -If a patient is unable to use his or her mental abilities to reach an informed decision, a medical emergency waiver of informed consent may be granted. This can occur with emergencies involving drugs, alcohol, injury, trauma, and or shock. -The waiver is also granted in situations of life- or health-threatening injury or diseases that require immediate treatment, and where any delay in treatment would result in compromise of the patient’s health. -If the patient threatened him/herself or others, and you have a strong reason to believe the patient’s threats are real, then you can transport without consent, after consulting medical direction. Law enforcement is typically required. Legal Considerations Concerning Restraint: -Involve the chain of command to protect yourself legally: -Before you restrain a patient, consult medical direction. -Involve law enforcement when you need to restrain a patient or transport without consent. Law enforcement personnel can protect you from injury, assist in restraint, and serve as credible witnesses. -Most areas require police authorization to transport or restrain without consent. Consult local protocol. -Use Reasonable Force: -Reasonable force is defined as the minimum amount of force required to keep the patient from injuring himself or others. -It is determined by: 1) The Patient’s Size and Strength: Bigger, stronger patients require more force. 2) Type of Behavior: You can use more force against violent patients. 3) The Patient’s Mental State: It is reasonable to use more force against an agitated patient than a quiet one. 4) The Patient’s Gender: Males may require more force than females. 5) The Method of Restraint: Metal cuffs are not reasonable. -EMTs can use reasonable force to defend against an attack in most areas. -Avoid any act or use of force that may injure the patient. -Patients may become calm and then revert to aggression. Therefore, do not remove restraints. Documentation – Protecting Yourself from Liability and False Accusations: -Document that the patient is able to communicate a choice and that it remains stable over time. -Document that the patient understands his or her condition. -Document that the patient understands the information regarding the intervention. -Document that the patient appreciates the situation and its consequences. -Document that the patient is able to make rational decisions based on the information. -Document that the patient understands alternatives available and the consequences of each. -Document all abnormal behavior. -Verify with witnesses. Have witnesses sign a written report, if possible. -To avoid sexual claims, have same sex attendants and third party witnesses present. ****NOTE: Everything documented is admissible in court. If it is not documented, it is typically considered not to have happened. Each year around 4.3 to 7.4 million people receive treatment in an emergency department for mental health-related conditions.1,2 Many of these patients will require prehospital interventions. A coordinated effort involving prehospital personnel, emergency physicians, and psychiatrists will help reduce the morbidity and mortality that results from emergencies related to behavioral and psychiatric conditions. Patients suffering from mental health disorders can have a variety of presentations, and these disorders can be caused by a variety of conditions. The assessment and management of these patients can be one of the most challenging tasks you will have to perform as a member of the emergency medical services. However, it can also be one of the most rewarding, as you have the opportunity to prevent many unnecessary deaths, as well as to help patients receive the psychiatric care that they need. The purpose of this course was to add to your knowledge of these emergencies, so that you can quickly identify, assess, and determine the appropriate management and disposition of a patient suffering from behavioral/psychiatric emergencies. In addition, this course attempted to provide you with information that will assist you in being able to convey more information to the emergency department staff and, ultimately, provide an even higher quality of care to your patients.