Supplemental Figure Legends
advertisement

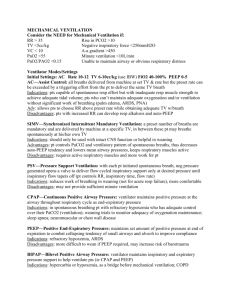
Bedside estimation of nonaerated lung tissue using blood gas analysis Andreas W. Reske, Eduardo Leite Vieira Costa, Alexander P. Reske, Anna Rau, João B. Borges, Marcelo A. Beraldo, Udo Gottschaldt, Matthias Seiwerts, Dierk Schreiter, David Petroff, Udo X. Kaisers, Hermann Wrigge, Marcelo B. P. Amato. SUPPLEMENTAL DIGITAL CONTENT 1 Methods Modeling the relationship between physiological shunt and PaO2 To study the relationship between physiological shunt and its surrogate PaO2, we built a model based on Berggren’s equation and on Fick’s principle (Figs. S1-S3, Supplemental Digital Content 2, http://links.lww.com/CCM/A554; Supplemental Digital Content 3, http://links.lww.com/CCM/A555; and Supplemental Digital Content 4, http://links.lww.com/CCM/A556, respectively). Using this model, PaO2 can be determined from physiological shunt if the following parameters are entered (values used in parentheses): oxygen extraction rate (0.3), pH (7.4), arterial partial pressure of carbon dioxide (PaCO2, 40mmHg), FiO2 (1.0), hemoglobin, oxygen consumption, and cardiac output. We used random samples of normal distributions of oxygen consumption (mean=400ml/min and SD=20ml/min) and of hemoglobin values (mean=10g/dl and SD=0.5g/dl). Cardiac output values were sampled from normal distributions generated with the mean values increasing from 6.0 to 10.0 L/min in steps of 0.5 L/min, and with a coefficient of variation of 5%. For each cardiac output distribution, we ran the model 160 times with physiological shunt values varying from 0.025 to 0.8 in steps of 0.005. In all the following notations, “x” represents either venous, lung capillary or arterial blood. Hemoglobin oxygen saturation was calculated according to equation 1 (S4). (1) Blood oxygen content was calculated according to standard formula (equation 2) (S5). 2 (2) Alveolar partial pressure of oxygen was used to approximate capillary partial pressure of oxygen assuming null diffusion gradient (equation 3) (S6). (3) The lung was considered as a two-compartment model consisting of shunt or perfect oxygenation. Arterial oxygen content was calculated according to Fick's principle (equation 4) (S2, S3). (4) The mathematical model The input variables to the model were cardiac output (QT), shunt fraction (Fshunt), pH, PaCO2, Hb, FiO2 =1, maximal oxygen extraction rate (ERmax), PvO2init, and oxygen consumption (VO2max). In the first run, mixed venous oxygen content was calculated according to equation 2, where x = mixed venous blood, PvO2 = PvO2init, and SvO2 was calculated using equation 1. Arterial oxygen content was then calculated as a perfusion weighted average of CcO2 and CvO2 according to equation 4. DO2 for each compartment was subsequently calculated by multiplying QT by the arterial oxygen content. VO2 was calculated according to equation 5: 3 VO2 = DO2 . ERmax if DO2 . ERmax < VO2max (5) VO2 = VO2max if DO2 . ERmax ≥ VO2max A new value for the mixed venous oxygen content was then obtained using equation 6. (6) PvO2 and SvO2 were determined from CvO2 by solving equations 1 and 2 to an acceptable error of 1:1000 using the Newton-Raphson method. The new calculated PvO2 substituted PvO2init in the second run of the model yielding a new, updated value of PvO2. This process continued until PvO2 would change by less 0.001 mmHg each run. At this point, the algorithm stopped and gave the following output variables: PvO2, SvO2, CvO2, PcO2, ScO2, CcO2, PaO2, SaO2, CaO2, VO21, VO21, CvO21, CvO22, DO2, and VO2. Some of the parameters in the model were calibrated using data obtained in the animal experiments described below. A more sophisticated model was used to simulate the influence of different inspired oxygen fractions on the calculus of venous admixture. In this model, we added 49 compartments in parallel to the shunt compartment. We assumed that the remaining non-shunting cardiac output was evenly distributed across those 49 compartments, each one having different ventilation and, consequently, a different V/Q ratio. In each 4 compartment, end-capillary partial pressure of oxygen was allowed to equilibrate with the alveolar partial pressure of oxygen, which was obtained by solving the mass balance equation for oxygen (equation 7) with the Newton-Raphson method. The model was adjusted to present an average V/Q ratio of 0.89 and a distribution with log(SD) = 0.26. Clinically, this model would represent a patient with moderate to severe V/Q inhomogeneity, typically found in patients submitted to low tidal-volume ventilation (S12). V V PiO 2 PAO 2 CcO 2 CvO 2 Q Q (7) The acronym PiO2 refers to the inspiratory partial pressure of oxygen. Animal experiments To obtain data for a wide range of lung aeration, we used data from an experiment during which ten pigs (mean weight 27 kg, standard deviation 2.3 kg) were subjected to saline lung lavage (surfactant washout) and subsequent injurious mechanical ventilation leading to experimental acute lung injury (ALI) as described below. Arterial and mixed-venous blood gases were obtained at different airway pressures resulting in varying amounts of nonaerated lung. The pigs were premedicated (intramuscular acepromazin, ketamin and midazolam), anesthestized (continuous intravenous infusion of ketamine, thiopental and midazolam), tracheotomized (7.0 mm ID endotracheal tube) and mechanically ventilated (New Port e500, Newport Medical, CA, USA). Ventilator settings during baseline pressure controlled ventilation were: driving pressure of 10 cmH2O, positive 5 end-expiratory pressure (PEEP) of 5 cmH2O, respiratory rate of 20*min-1, inspiratoryto-expiratory ratio (I:E) of 1:2 and the fraction of inspired oxygen (FiO2) was 1.0. A pulmonary artery catheter (PAC 7.5F, CCOmbo CCO/SvO2, Edwards Lifesciences, Germany) was introduced via the right external jugular vein for sampling of mixed venous blood. The correct position of the PAC was confirmed by analysis of pressure tracings. The left femoral artery was cannulated for sampling of arterial blood and continuous blood pressure monitoring. Arterial and mixed venous blood-gases were analyzed using a co–oximeter (ABL 800 flex, Radiometer©, Copenhagen, Denmark). Experimental lung injury was induced by repeated lung lavage with normal saline (30 ml/kg body weight, body temperature) until the PaO2 remained stable below 100 mmHg for at least 10 minutes during ventilation with pure oxygen (S7). A mean number of 10 (standard deviation 3.2) lung lavages was required to reach this criterion. Immediately after the lung lavage procedure, injurious mechanical ventilation with low PEEP (1 to 5 cmH2O) and high peak airway pressures (42 to 48 cmH2O) was started and maintained for three hours. After completion of this period of injurious mechanical ventilation, pigs were submitted to a lung recruitment maneuver. The lung recruitment maneuver was performed by stepwise increases of PEEP and peak airway pressures using the following ventilator settings: respiratory rate of 20*min-1, I:E of 1:2 and FiO2 of 1.0. Maintaining a constant driving pressure of 15 cmH2O, PEEP was increased in steps of 5 cmH2O from 25 cmH2O to 45 cmH2O. Each incremental PEEP step lasted two minutes. The sequence of incremental PEEP steps was continued until the peak airway pressure reached 60 cmH2O or until our blood gas-based recruitment target - PaO2 plus arterial partial pressure of carbon dioxide (PaCO2) equal ore greater than 400 mmHg - was reached. Immediately after the lung recruitment maneuver, a decremental PEEP titration was started during which PEEP was decreased in steps of 2 cmH2O from 25 to 5 cmH2O. During the 6 decremental PEEP titration, each PEEP level was maintained for four minutes with a fixed driving pressure of 6 cmH2O during pressure controlled ventilation. Arterial and mixed-venous blood samples were drawn at the end of each PEEP step and immediately afterwards analyzed at body temperature. At the end of the experiment, animals were killed by an intravenous overdose of thiopental and potassium chloride. Patients We analyzed data of patients in whom CT scanning had been requested by the treating physician as clinical diagnostic procedure for emergency trauma workup or in patients from Intensive Care Unit (ICU). All patients had indwelling arterial catheters which were placed for routine hemodynamic management through which arterial blood was sampled for blood gas analysis immediately before or after CT. Patients with multiple trauma were treated by the trauma team following standardized institutional guidelines with a whole-body helical CT with contrast medium as the central diagnostic component (S8-S10). Pressure controlled mechanical ventilation (Oxylog 3000, Dräger, Lübeck, Germany) during primary resuscitation and transportation to the CT suite was standardized and included the following ventilator settings: target tidal volume of 6-8 ml/kg estimated body weight (estimated weight in kilograms equals height in centimeters minus 100), a respiratory rate of 20*min-1 and PEEP of 10 cm H2O unless higher PEEP had already been applied upon admission. The FiO2 during initial resuscitation and CT was 1.0. Subsequent FiO2 adjustment was at the discretion of the physician in charge. 7 For intensive care unit patients, all previous ventilator settings were maintained on the transport ventilator (Oxylog 3000, Dräger, Lübeck, Germany) during transportation to the CT suite, only the FiO2 was changed to 1.0 before transportation. Derecruitment due to disconnection from the mechanical ventilator was prevented by clamping the endotracheal tube. Physiological and demographic data, ventilator variables and blood gas measurements data had been prospectively and automatically entered into the patient data management system of our institution. CT scanning All patients underwent multislice helical CT using either a Somatom Volume Zoom (Siemens, Erlangen, Germany) or a MX-8000 IDT 16 (Philips Medical Systems, Hamburg, Germany) scanner during uninterrupted mechanical ventilation. The following scan protocols were used: Somatom Volume Zoom - 120 kV tube voltage, 165 mAs tube current, 4 x 2.5 mm collimation, pitch 1.1; and MX-8000 IDT 16 - 120 kV tube voltage, 180 mAs tube current, 16 x 1.5 mm collimation, and pitch 0.622. Depending on the CT scanner, the reconstruction filters “B” (MX-8000 IDT 16) or “B60f” (Somatom Volume Zoom) were used for reconstruction of CT image series covering the entire thorax. Contrast material was administered when clinically indicated (120 ml Iopamidol, Schering AG, Berlin, Germany). 8 Prediction of CT-shunt from PaO2/FiO2 values In a final regression analysis relating PaO2/FiO2 and CT-shunt (%Mass [-200 to +100] HU, this choice of interval is justified in the discussion section of the main text), we choose PaO2/FiO2 as the dependent variable, since that will be used to estimate CTshunt. We performed a logit transformation of CT-shunt /100 to ensure that it remains within the interval [0, 100] and to have much higher homoscedasticity. Supplemental Figure 4 (Supplemental Digital Content 5, http://links.lww.com/CCM/A557) and the value for the coefficient of determination R2=0.85 demonstrate that these quantities are also modelled well by a linear relationship. The result of the regression analysis is CT-shunt ln 0.79 0.00735 PaO2 / FiO2 100 CT-shunt with 95% CIs of [0.52, 1.05] and [-0.0081, -0.0066] for the intercept and slope respectively. This equation was used to calculate the results presented in Table 3 of the main text relating PaO2/FiO2 and the predicted amounts of CT-shunt in the form of a lookup table. In addition to this table, Supplemental Figure 4 (Supplemental Digital Content 5, http://links.lww.com/CCM/A557) and Supplemental Figure 5 (Supplemental Digital Content 6, http://links.lww.com/CCM/A558) also illustrate the 95% confidence interval of the regression line as well as the 75% and 95% prediction intervals within which the respective percentage of CT-shunt values predicted from PaO2/FiO2 measurements will fall. Preliminary validation tests Thorough and statistically powerful validation of our findings requires sufficiently large validation samples the collection of which is an ongoing project of our research group. Therefore, we performed analyses on a preliminary validation sample (12 9 patients) in order to check our initial results. All patients had acute respiratory distress syndrome (ARDS, mild to severe) according to the Berlin definition of ARDS (S11). Visual inspection of a plot showing the new data points of the test patients together with the initial data revealed no obvious differences between the initial and the test data. The same applies to comparison of the regression residuals of the test data (calculated using the regression equation obtained with the initial data) to the regression residuals of the initial analysis. As prediction of the amount of nonaerated lung parenchyma from measurement of PaO2/FiO2 is to be validated here, we chose the ln transformation of PaO2/FiO2 as the independent variable for these figures. 10 We also tested whether the amount of nonaerated lung parenchyma (nonaerated lung mass within -200 to +100 HU) predicted from PaO2/FiO2 (measured during 100% oxygen ventilation) of the new patients would fall into the 75% prediction intervals given in Table 3 of the main text. Because we have only few validation data for testing the prediction intervals given in Table 3, we omit further statistical analyses, but mention in passing that 10 out of the 12 values lie within the 75% prediction interval. This corresponds well to what one expects. Taking these new results from the validation sample into account, we feel reassured that our results do apply to mechanically ventilated patients with a clinically relevant spectrum of lung conditions, including ARDS patients and we look forward to presenting more powerful validation results in the future. 11 References for the Supplemental Digital Content S1. Berggren SM: The oxygen deficit of arterial blood caused by nonventilating parts of the lung. Acta Physiol Scand 1942; 4(suppl XI):1– 92. S2. Riley RL, Cournand A: Analysis of factors affecting partial pressures of oxygen and carbon dioxide in gas and blood of lungs; theory. J Appl Physiol 1951; 4:77-101 S3. Riley RL, Cournand A, Donald KW: Analysis of factors affecting partial pressures of oxygen and carbon dioxide in gas and blood of lungs; methods. J Appl Physiol 1951; 4:102-120 S4. Severinghaus JW: Simple, accurate equations for human blood O2 dissociation computations. J Appl Physiol 1979; 46:599-602 S5. Roughton FJ, Severinghaus JW: Accurate determination of O2 dissociation curve of human blood above 98.7 percent saturation with data on O2 solubility in unmodified human blood from 0 degrees to 37 degrees C. J Appl Physiol 1973; 35:861-869 S6. Riley RL, Cournand A: "Ideal" Alveolar air and the analysis of ventilation-perfusion relationships in the lungs. J Appl Physiol 1949; 1:825-847 S7. Lachmann B, Jonson B, Lindroth M, et al: Modes of artificial ventilation in severe respiratory distress syndrome. Lung function and morphology in rabbits after wash-out of alveolar surfactant. Crit Care Med 1982; 10:724-732 S8. Schreiter D, Reske A, Stichert B, et al: Alveolar recruitment in combination with sufficient positive end-expiratory pressure 12 increases oxygenation and lung aeration in patients with severe chest trauma. Crit Care Med 2004; 32:968-975 S9. Reske AW, Reske AP, Heine T, et al: Computed tomographic assessment of lung weights in trauma patients with early posttraumatic lung dysfunction. Crit Care 2011; 15:R71 S10. Huber-Wagner S, Lefering R, Qvick LM, et al: Effect of whole-body CT during trauma resuscitation on survival: a retrospective, multicentre study. Lancet 2009; 373:1455-1461 S11. The ARDS Definition Syndrome-The Task Force. Berlin Acute Definition. Respiratory Distress JAMA 2012; 307:doi:10.1001/jama.2012.5669 S12. Feihl F, Eckert P, Brimioulle S, Jacobs O, Schaller MD, Mélot C, Naeije R. Permissive hypercapnia impairs pulmonary gas exchange in the acute respiratory distress syndrome. Am J Respir Crit Care Med 2000; 162:209-215 13 Supplemental Figure Legends Supplemental Figure 1: Supplemental Figure 1 illustrates the regression of the logarithmically (ln) transformed PaO2/FiO2 on Riley‘s approximation to shunt for theoretical data from model simulations (left panel), data from the animal experiment in pigs with acute lung injury (middle panel) and data from the 77 patients with single data-points (right panel). All PaO2/FiO2 measurements or simulations were made during 100% oxygen ventilation. For the definition of Riley‘s approximation to shunt, the reader is referred to the Methods section of the main manuscript. The red dashed lines correspond to the least squares regression lines. PaO2/FiO2 - arterial partial pressure of oxygen divided by the fraction of inspired oxygen (FiO 2). ln, natural logarithm. R2 - coefficient of determination. Supplemental Figure 2: Supplemental Figure 2 illustrates the influence of the fraction of inspired oxygen (FiO2) on the correlation between venous admixture (in the case of FiO 2 below 1) or physiological shunt (pure oxygen ventilation), respectively, and lnPaO2/FiO2. The plots represent simulated data, using a multi-compartment model with 49 compartments representing moderate to severe ventilation-to-perfusion inhomogeneity and one shunt compartment (see supplemental Methods). This situation is typically found in patients submitted to low tidal-volume ventilation. The wider scattering of data points associated with lower FiO2 obviously degrades the correlation and is the consequence of two phenomena: a) in the presence of low V/Q units with critically low alveolar-PO2, random changes in cardiac output, hemoglobin 14 concentration or oxygen consumption (as simulated in the model) have larger impact on PaO2 and on the calculus of venous admixture; and b) we simulated changes in FiO2 around the mean (50%), with a standard deviation (SD) of 10% to reproduce slightly varying FiO2 values during the patient evolution. Despite the proper computation of the FiO2 actually applied, the impact on venous admixture and on PaO2/FiO2 is non-linear, causing additional scattering. Supplemental Figure 3: Supplemental Figure 3 illustrates the influence of the fraction of inspired oxygen (FiO2) on the correlation between Riley‘s approximation to physiological shunt and CT-shunt (upper panels) and between the logarithmically (ln) transformed PaO2/FiO2 and CT-shunt (lower panels). Data in this figure were obtained in a subgroup of 27 patients out of the 77 patients with single data-points for whom we had PaO2/FiO2 measurements for both, 50% and 100% oxygen (with a time interval of approximately ten minutes between measurements and where one data point had to be removed since it was an outlier with very large leverage). The use of 100% oxygen improved the correlations but note that this correlation analysis is not robust enough to demonstrate the influence of FiO2 conclusively. Most of these patients had low levels of CT-shunt, thus representing healthier conditions than the simulations with greater ventilation-to-perfusion inhomogeneity in Supplemental Figure 2 (Supplemental Digital Content 3, http://links.lww.com/CCM/A555). For the definition of different shunt entities, the reader is referred to the Methods section of the main manuscript. The thick red dashed lines correspond to the least squares regression lines and the black dashed lines mark the 95%CIs of the regression line. PaO2 - arterial partial pressure of oxygen. ln - natural logarithm. %Mass-200 to +100 HU (left panel) refers to the lung 15 mass within the given interval of Hounsfield Units (HU) expressed as percentage of the total lung mass. R2 - coefficient of determination. 16 Supplemental Table 1. Patient data Number of patients (female) Number of CTs / patient Age (years) Body mass index Multiple trauma patients (%) Other patients (%) Patients with ARDS (%) Time to first CT (hours) Time to repeat CT (hours) Contrast medium PEEP (cm H2O) PIP (cm H2O) PaO2/FiO2 at CT (mm Hg) PaCO2 at CT (mm Hg) delta PaO2/FiO2 (mm Hg) Hemoglobin (g*dl-1) Total lung weight (g) Total lung volume (ml) %V-100 to +100 HU (%) %V-500 to -100 HU (%) %M-100 to +100 HU (%) %M-200 to +100 HU (%) %M-500 to -100 HU (%) single CT 77 (17) 45 (15-82) 25.7 (20.2-37.0) 61 (79 %) 16 (21 %) 34 (44 %) 2.0 (0.75-437) 69 (90 %) 10 (6-20) 25 (19-37) 327 (54-664) 46.7 (27.3-128.0) 10.6 (5.5-15.3) 992 (636-3019) 3738 (1568-6213) 3.5 (0.1-53.7) 7.0 (1.8-43.6) 12.0 (0.7-78.8) 15.8 (1.3-82.5) 15.6 (5.4-50.8) repeat CT 8 (1) 2 (2-4) 30 (17-75) 24.3 (19.9-29.7) 7 (87%) 1 (13%) 5 (63 %) 1.7 (1.3-120.0) 29 (7-334) 8 (75 %) 10 (10-20) 23 (16-37) 301 (48-592) 48.8 (32.4-78.1) 113 (13-441) 10.0 (8.9-14.5) 1381 (783-3017) 3715 (2078-6351) 5.4 (0.3-45.9) 19.5 (5.6-35.6) 14.2 (0.8-63.7) 20.8 (1.6-71.5) 28.9 (10.3-44.5) Supplemental Table 1 lists descriptive, physiological and quantitative CT data. Data are given as median (minimum-maximum). CT - computed tomography; Body mass index - weight in kilograms divided by the square of the height in meters; ARDS - all patients with acute respiratory distress syndrome defined according to reference 65; Time to first CT - median time between commencement of mechanical ventilation and CT; Time to repeat CT - median time between two consecutive CT; PEEP - positive end-expiratory pressure; PIP - peak inspiratory pressure during pressure controlled mechanical ventilation; PaO2/FiO2 - arterial partial pressure of oxygen divided by the fraction of inspired oxygen, both measured at the time of CT; PaCO2 - arterial partial pressure of carbon dioxide measured at the time of CT. %V refers to the lung volume within the given range of Hounsfield Units (HU) expressed as percentage of the total lung volume. %M was calculated accordingly and expressed as percentage of the total lung mass. 17 Supplemental Table 2. Regression results Univariate Analysis Multivariate Model Independent Partial Attributable Variables Correlation P-value Variance P-value %M-100 to +100 HU %M-200 to -100 HU %M-300 to -200 HU %M-400 to -300 HU %M-500 to -400 HU %M-100 to -500 HU PaCO2 Hemoglobin PEEP PIP Body Mass Index Total lung weight Trauma vs. others Contrast material -0.90 -0.65 -0.50 -0.32 -0.11 -0.42 -0.51 0.17 -0.39 -0.48 -0.37 -0.58 0.39 0.24 <0.0001 <0.0001 <0.0001 0.004 0.36 <0.0001 <0.0001 0.15 <0.0001 <0.0001 0.001 <0.0001 0.001 0.04 81.5 % 5.7 % 1.2 % 0.7 % 0.8 % - <0.0001 <0.0001 0.64 0.43 0.39 0.44 0.01 0.32 0.09 0.18 0.03 0.50 0.02 0.25 89.3 % <0.0001 Best multivariate model Supplemental Table 2 lists the results of univariate and multivariate regression analyses involving variables potentially explaining differences in the logarithmicall (ln) transformed PaO2/FiO2 in patients with single CT. %M refers to the lung mass within the given range of Hounsfield Units (HU) expressed as percentage of the total lung mass. PaCO2 - arterial partial pressure of carbon dioxide measured at the time of CT; PEEP - positive end-expiratory pressure; PIP - peak inspiratory pressure during pressure controlled mechanical ventilation; Body mass index - weight in kilograms divided by the square of the height in meters. Attributable variance refers to the percentage of variance in the ln transformed PaO2/FiO2 explained by the independent variables shown. It corresponds to the R2 change resulting from inclusion of the indicated variable into the pre-adjusted model. Only the variables in bold italic font were included in the multivariate model. 18 Supplemental Table 3 Look-up table for prediction of CT-shunt from PaO2/FiO2 values PaO2/FiO2 predicted CT-shunt (%) 75% prediction interval (%) 40.00 62.1 46.5 to 75.5 50.00 60.3 44.7 to 74.1 60.00 58.5 42.9 to 72.6 70.00 56.7 41.2 to 71.1 80.00 54.9 39.4 to 69.6 90.00 53.1 37.7 to 68.0 100.00 51.3 36.0 to 66.3 120.00 47.6 32.7 to 62.9 140.00 44.0 29.6 to 59.4 160.00 40.4 26.6 to 55.8 180.00 36.9 23.9 to 52.1 200.00 33.5 21.3 to 48.4 220.00 30.3 19.0 to 44.8 240.00 27.3 16.8 to 41.2 260.00 24.5 14.9 to 37.6 280.00 21.9 13.1 to 34.3 300.00 19.5 11.5 to 31.0 320.00 17.3 10.1 to 28.0 340.00 15.3 8.9 to 25.1 360.00 13.5 7.7 to 22.4 380.00 11.9 6.7 to 20.0 400.00 10.4 5.9 to 17.7 420.00 9.1 5.1 to 15.7 440.00 8.0 4.4 to 13.9 460.00 6.9 3.9 to 12.2 480.00 6.1 3.3 to 10.7 500.00 5.3 2.9 to 9.4 520.00 4.6 2.5 to 8.2 540.00 4.0 2.2 to 7.2 560.00 3.5 1.9 to 6.3 580.00 3.0 1.6 to 5.5 600.00 2.6 1.4 to 4.8 19 This table lists values of CT-shunt and the respective 75% prediction interval (PI) which were predicted from PaO2/FiO2 values. For a future patient, the 75% PI specifies the range within which a single CT-shunt value which was predicted from a PaO2/FiO2 value will lie with 75% certainty. Such a PI should not be confused with the much narrower confidence interval for the mean of future measurements of CTshunt for a given PaO2/FiO2. The somewhat unconventional 75% PI was chosen here to provide the clinician with an interval narrow enough to suggest a course of action, but broad enough to include a good majority of the expected values. The equation for regression relating PaO2/FiO2 and CT-shunt found in our study was used for calculation. This regression equation was: CT - shunt ln 100% CT - shunt 0.79 0.00735 PaO2 / FiO2 The 95% confidence intervals for coefficient and intercept in the regression equation were -0.0081 to -0.0066 and 0.52 to 1.05, respectively. The calculations shown in this table are only valid for 100 % oxygen ventilation. PaO 2/FiO2 - arterial partial pressure of oxygen divided by the fraction of inspired oxygen (FiO2). ln - natural logarithm. CTShunt is given as percentage of the total lung mass for [-200 HU to +100] Hounsfield Units. For further information, the reader is referred to Supplemental Figure 3 (Supplemental Digital Content 4, http://links.lww.com/CCM/A556) and Supplemental Figure 4 (Supplemental Digital Content 5, http://links.lww.com/CCM/A557). Supplemental Figure 4: Supplemental Figure 4 demonstrates the linear relationship between the transformed CT-shunt and PaO2/FiO2. CT-shunt is calculated as %Mass within the [-200 to +100] 20 Hounsfield Units interval and is transformed according to ln[CT-shunt /(100- CTshunt)]. Note the uniformity of the variance over all PaO 2/FiO2 values as reflected in the P-value of 0.97 for the Breusch-Pagan test as compared to the P-value 0.001 for linear regression between the logarithmically (ln) transformed PaO2/FiO2 and CTshunt. This homoscedasticity is a prerequisite for the reliability of the confidence and prediction bands. In addition to the 95% prediction interval, the somewhat unconventional 75% prediction interval is presented here to provide the clinician with an interval narrow enough to suggest a course of action, but broad enough to include a good majority of the expected values. Supplemental Figure 5: The linear regression and confidence and prediction bands of Figure S4 are transformed back to the “natural” units for CT-shunt in %Mass within the [-200 to +100] Hounsfield Units interval. Supplemental Figure 6: Individual within-patient correlation between the logarithmically (ln) transformed PaO2/FiO2 and CT-shunt in patients with repeat CT from the present study (left panel) and the study by Borges et al. (right panel, see reference 12 in the main text). The solid black lines correspond to the individual least squares regression lines, or connect individual data points (if only two data points were available). The corresponding correlation between changes (delta) in ln-transformed PaO2/FiO2 and changes in CT-shunt in patients with repeat CT is illustrated in Figure 6 in the main text. PaO2/FiO2 - arterial partial pressure of oxygen divided by the fraction of inspired oxygen (FiO2). ln - natural logarithm. R2 - coefficient of determination. %Mass-200 to 21 +100 HU refers to the lung mass within the given interval of Hounsfield Units (HU) expressed as percentage of the total lung mass. Supplemental Figure 7: Supplemental Figure 7 illustrates the relationship between "percent-volume” and “percent-mass” estimates of nonaerated lung (CT-shunt). "Percent-volume" (%Volume) was calculated as the volume of nonaerated lung within the [-100 to +100] Hounsfield Units (HU) interval and calculated as percentage of the total lung volume. “Percent-mass” (%Mass) denotes the mass of nonaerated lung within the [100 to +100] HU interval which is calculated as percentage of the total lung mass. Data of the 77 patients with single data points were used for this analysis. Please note that, independent from the function chosen to fit the relationship, expression of CT-shunt as %Volume underestimates the true mass fraction (%Mass) of nonaerated lung. 22