Percutaneous Techniques for Treating Disc Disease
advertisement

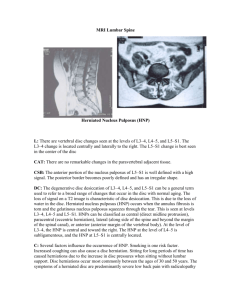
LS III-3 Percutaneous Techniques for Treating Disc Disease Marco Leonardi, M.D. Servizio di Neuroradiologia, Ospedale Bellaria, Bologna, Italy. Introduction The percutaneous approach to disc diseases was proposed many years ago and several different techniques have been applied. Some are more “surgical”, like the Caspar technique based on the insertion of thick tubes, even bilaterally, to allow mechanical rupture and removal of nucleus fragments. Other methods may be considered more “mildly-invasive” and “radiological”, such as chemonucleolysis with chymopapain or mechanical fragmentation by means of thin probes and suction of nuclear fragments, such as the Onik procedures. More recently, technological advances have led to the use of an oxygen-ozone mixture to obtain chemical lysis of the nucleus or mechanical fragmentation with thinner probes. This presentation describes the different uses of these modalities which are based on the percutaneous approach to the disc and the basic diagnostic information supplied by discography. In fact, discography underlies all of these techniques given the need to check the exact position of the needle and the exact size and position of the herniated nucleus: percutaneous techniques are effective when the herniated part is connected with the centre of the nucleus which is the sole possible percutaneous target. The percutaneous techniques have no possibility of reaching the herniated part, their effect is on the nucleus and will be effective on the herniations if there is a continuity which will “transfer” the therapeutic effects to the herniated fragment. Chemonucleolysis Chemonucleolysis exploits the enzymatic activity of papain, which acts on the proteoglycans, breaking up their protein “core” with a consequent reduction of the water content of the nucleus pulposus. Chymopapain may give rise to allergic and anaphylactic reactions as well as a toxic enzymatic action on the arachnoid capillaries (if injected intrathecally). For this reason, chemonucleolysis must be performed under discographic guidance. Chemonucleolysis with papain is widely used in France. In Italy we have performed more than two thousand procedures with good results in 83% of cases. One patient presented a vertebral body discitis which resolved in three months with drug management. Onik’s Automated Discectomy This method is based on the use of a probe under vacuum which automatically aspirates and fragments disc material which is collected in a bottle together with the flushing saline solution. Like chemonucleolysis, it is performed under discographic guidance. Automated discectomy is indicated in smaller herniations than those treated by chemonucleolysis. In our experience, treating about 400 patients, it was successful in 75% of cases. Oxygen-Ozone Therapy This technique is described in more detail, because it is the newest procedure with few literature reports available. At disc level, the mechanism of oxygen-ozone action is the oxidation of proteoglycans with rupture of the sulphydryl bonds and a reduction of hydrophilic capacity, similar to that of chymopapain, but more attenuated with a significant decrease in pain after treatment. At root level, the mechanism of action is generically described as anti-inflammatory. From December 1997 to August 2000 we treated 444 patients, 240 men and 204 women, administering 723 treatments at disc levels L4-L5 and L5-S1 in 85% of cases. Two levels were treated in 160 patients and three levels in eight. Repeat treatments involved the same level in 100 patients and a different level in 25. We describe 191 patients who underwent treatment at a single sitting with a follow-up visit six months later. All patients had a four to six month history of intractable back and leg pain despite conservative measures without neurological deficit. All patients underwent CT and/or MR scan with a diagnosis of disc herniation at one or more levels. Patients with neurological deficit or neurological features suggesting migrated herniated fragment were excluded. Treatment consisted in intervertebral disc puncture in fluoroscopy (G22 needle) followed by discography to confirm correct needle placement and ascertain the morphology of the herniation (to rule out herniated fragments) and the degree of disc degeneration. A 27 mcmg/ml ozone mixture was injected 4ml into the disc and 8ml into the perivertebral and periradicular soft parts. Patients were then assessed after 7-10 days, one month and six months. Treatment was successful in 126 cases, with no change in symptoms in 56 and a worsening of symptoms in nine. One of the latter presented mild spondilo-discitis treated conservatively with success; the other eight probably deteriorated because of disease progression. As a whole, excellent-good results were achieved in 66% of cases, a lower percentage than that of enzymatic chemonucleolysis. This is an important parameter since comparison with chemonucleolysis is best suited to ascertain the advantages of ozone therapy given the similar degree of invasiveness. However, ozone treatment is even less invasive than chemonucleolysis: a narrower gauge needle is used and the period of discomfort following treatment and bed rest is reduced to two or three days instead of one to two weeks; no hospital stay is necessary thereby making the cost of ozone therapy ten times lower. Repeat treatments will enhance results and are usually suggested by patients satisfied with the previous outcome and keen to repeat the treatment for a recurrence or to enhance results giving a significant but incomplete improvement of symptoms. Manual Percutaneous Discectomy Based on the use of probes, similar to Onik’s introductory system, and special mini-forceps for the mechanical removal of the nucleus pulposus this technique has been implemented in few cases and no conclusions can yet be drawn on its effectiveness. Treatment of Failures Most patients who fail to benefit from percutaneous treatments are referred for surgery without any negative effects. Our series included two patients who underwent surgery soon after oxygen-ozone therapy. They presented severe disc degeneration, probably the result of nucleolysis with ozone which will be the topic of a separate report. Conclusions Papain and Onik were widely used about ten years ago, results were satisfactory in selected cases, but several problems arose. In fact, papain (chymodiactin) obtained FDA authorisation in 1982, but never received EU approval, which is a major drawback in Europe, especially nowadays with the increasingly high risk of litigation in the case of failure or complication. In our experience, the Onik procedure is indicated for small herniations, and the ratio between cost-invasiveness and pathology definitely favours a more conservative approach or a less invasive procedure. Intradiscal ozone therapy is successful in a slightly lower percentage of patients than those treated by chemonucleolysis, but it is well tolerated even in elderly patients. The burning sensation experienced on paraspinal and periradicular injection of the ozone is temporary. The slight reduction in the percentage of positive results compared with chemonucleolysis becomes negligible in the context of a wider cost-benefit assessment. The percutaneous approach allows the treatment of disc herniation with a satisfactory level of good results, average 70%, in selected cases, with small or medium size herniations with continuity between the central nucleus and the herniated fragment. Note More and more frequently we find disc pathology associated with vertebral spine instability, especially in elderly people or in post surgical cases. The diagnosis of vertebral instability is crucial and will radically affect the therapeutic approach (cage stabilisation, etc.). From August 1999 to date, our neuroradiology unit has investigated vertebral instability by loaded lumbosacral spine CT scans (AL-CT) using a custom-made axial compressor. CT study aims to disclose vertebral instability and/or significant changes to disc morphology by simulating the movement from sitting to standing by applying a load equal to 65% of the patient’s body weight. The examination includes two CT acquisitions of the lumbosacral spine from L3 to S1 at rest and after application of the axial load followed by multiplanar and 4D-Angio reconstructions and a cine comparison of the reformatted images with and without axial-loading (Kodak PACS Workstation). This type of CT examination is essential in doubtful cases to avoid inappropriate treatment of simple disc herniations. Acknowledgements: I wish to express my gratitute to my coworkers, Giuliano Fabris, Antonino Lavaroni, Carlotta Barbara, Luigi Simonetti and Silvia Giatti, whose help has proved invaluable. Prof. Marco Leonardi Servizio di Neuroradiologia Ospedale Bellaria Via Altura 3 40139 Bologna, Italy Tel.: +39.051.6225520 Fax: +39.051.6225785 E mail: marco.leonardi@ausl.bologna.it References 1. Barbara C, Simonetti L, Giatti S, Leonardi M: Trattamento percutaneo dell’ernia discale lombare con iniezione intradiscale di miscela di ozono. XVI Congresso Nazionale dell’Associazione Italiana di Neuroradiologia. Rivista di Neuroradiologia, 12 (suppl.4):39, 1999. 2. Bocchi L, Ferrata P, Passariello F, Belloni G, Bonaldi G, Moschini L, Solini A, Ruggieri N, Pasquini U, Salvolini U, Indemini F, Tabasso G, Fabris G, De Nardi F, Leonardi M: La Nucleoaspirazione secondo Onik nel trattamento dell’ernia discale lombare. Analisi multicentrica dei primi risultati su oltre 650 trattamenti. Rivista di Neuroradiologia 2 (Suppl 1): 119-122, 1989. 3. Bocci V: Ozone as a bioregulator. Pharmacology and toxicology of ozonetherapy today. J Biol Regul. Homeos Agents 10: 31-53, 1998. 4. Fabris G, Lavaroni A, De Nardi F, Leonardi M, Biasizzo E: La Chemonucleolisi nell’ernia discale lombare. Rivista di Neuroradiologia 2 (Suppl 1): 93-101, 1989. 5. Fabris G, Lavaroni A, Leonardi M: Discography. Edizioni del Centauro, Udine 1991. 6. Leonardi M, Fabris G, Lavaroni A: Percutaneous Diskectomy and Chemonuclelysis. In: Medical Radiology, Interventional Neuroradiology. Edited by A. Valavanis. Springer-Verlag, Heidelberg 1993: 173-190. 7. Leonardi M: Discography – How-to-Workshop, course n. 550. RSNA ‘93, Radiological Society of North America, 79th Annual Meeting, Chicago November 28 - December 3, 1993. Radiology 189 (suppl): 78, 1993. 8. Leonardi M: Discography, Chemonucleolysis and Percutaneous Discectomy. How To Workshop, course n. 450.. RSNA ‘90, Radiological Society of North America, 76^ Annual Meeting, Chicago 25-30 novembre 1990; Radiology 177: 59, 1990. 9. Muto M, Avella F: Percutaneous treatment of herniated lumbar disc by intradiscal oxygenozone injection. Interventional Neuroradiology 4: 279-286, 1998. 10. Resta F, Lavaroni F, Fabris G, Bettinelli A, Mangiagalli E, Leonardi M: Percutaneous Treatment of Lumbar Disc Herniation. Rivista di Neuroradiologia 8 (Suppl. 1): 53-58, 1995. 11. Zanotti B, Fabris G, De Nardi F, Zappoli F, Biasizzo E, Lavaroni A, Leonardi M: L’ernia discale lombare e le terapie percutanee. Rivista di Neuroradiologia 4 (Suppl 2): 87-93, 1991. Captions Figure 1 AP and lateral view: the correct positioning of the needle at the centre of the disc is very important. Figure 2 Discography L4-L5: good position of the needle. Diffuse degeneration of the nucleus with posterior herniation. Figure 3 CT-Discography L4-L5, after oxygen-ozone injection: lateral right hernia. Little gas bubbles are recognisable around the nerve root and on the lateral margin of the herniated disc. Figure 4 CT-Discography L4-L5, after oxygen-ozone injection: large median disc herniation. Gas bubbles are recognisable in the hernia, around the nerve roots and in the paraspinal muscles. Figure 5 CT-Discography L5-S1, after oxygen-ozone injection: large discal hernia, paramedian, left. Gas bubble in the herniated disc.