4.2 CPG Minute 09 06 08
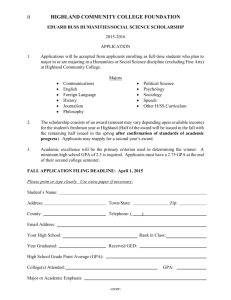
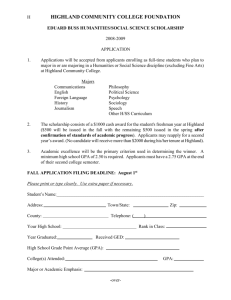
advertisement
Highland NHS Board 5 August 2008 Item 4.2 HIGHLAND NHS BOARD DRAFT MINUTE of MEETING of the CLINICAL PLANNING GROUP (SERVICE REDESIGN COMMITTEE) Board Room, Assynt House Assynt House Beechwood Park Inverness IV2 3BW Tel: 01463 717123 Fax: 01463 235189 Textphone users can contact us via Typetalk: Tel 0800 959598 www.nhshighland.scot.nhs.uk Monday 9 June 2008 – 2.00 pm Present Dr Ian Bashford, Board Medical Director, in the Chair Dr Eric Baijal, Director of Public Health & Health Policy Mr Quentin Cox, Chair, Area Clinical Forum Prof John Cromarty, Director of Pharmacy Mr Stuart Denholm, Clinical Director, Raigmore Hospital Dr Moray Fraser, Clinical Director, North Highland CHP (videoconference) Dr Chris Lush, Clinical Director, Clinical Services & Support Directorate, Raigmore Ms Una Lyon, Lead Nurse, Raigmore (deputising for Heidi May) Dr Alistair McIntyre, Chair, Area Medical Committee Dr John May, Clinical Director, Surgical & Anaesthetic Directorate, Raigmore Dr Ken Proctor, Associate Medical Director (Primary Care) Dr Ian Scott, Clinical Director, South East Highland CHP In Attendance Dr Helen Shannon, Consultant Radiologist (item 3) Ms Katherine Sutton, Superintendent Radiographer (item 3) Ms Linda Kirkland, General Manager, Medical Directorate (item 4) Miss Irene Robertson, Board Committee Administrator Apologies - Ms Margaret Brown, Mrs Helen Bryers, Dr Grace Fergusson, Dr Michael Hall, Dr Rod Harvey, Mr Nigel Hobson, Dr D A Russell Lees, Dr Chris MacGregor, Ms Heidi May, Mr Ray Stewart and Dr Angus Venters 1 MINUTES The minute of meeting held on 12/11/07 was approved. 2 CLINICAL ADVICE TO THE BOARD – FUTURE OF CLINICAL PLANNING GROUP A copy of the Group’s current remit had been circulated along with some proposals relating to membership and working arrangements. The Chair reminded the Group of an earlier proposal that the Group should merge with the Financial Planning Group. The view held was that the Clinical Planning Group (CPG) should continue to function as a separate committee providing a high level of clinical scrutiny of appropriate issues while taking cognisance of financial considerations, identification of the risks of implementation or non-implementation, a priority of the issue, and give a view as to the possibility and capacity for implementation. The submissions to the CPG should be in broad business case form and be comprehensive, and have undergone the appropriate consultation. It was felt that the Area Clinical Forum being essentially a professional advisory body would not have the capacity to undertake the Working with you to make Highland the healthy place to be high level scrutiny required, whereas the members of the CPG had a managerial mandate and were better placed to bring a broader clinical perspective to the issues under debate. The CPG, as currently constituted, brought together primary and secondary care and provided a forum for comprehensive clinical debate on strategic issues. It was proposed that the existing membership should be expanded to ensure an inclusive representation, the revised membership agreed to comprise of the following: Board Medical Director - Chair Nominated Planning Lead (Head of Service Planning) Associate Medical Director (Primary Care) Director of Public Health & Health Policy Clinical Director, Raigmore Hospital Clinical Directors, Raigmore Directorates CHP Clinical Directors Mental Health Clinical Leads Board Nurse Director Associate Nurse Director Head of Midwifery Associate AHP Director Director of Pharmacy Chair of Area Medical Committee Area Clinical Forum Representative In the event that a member was unable to attend a CPG meeting, it was agreed that a deputy should attend. It was also agreed to co-opt expert members for specific topics, as necessary and appropriate to ensure that a full and comprehensive clinical opinion was sought from NHS Highland. The Chair advised that the CPG had previously been accountable to the Improving Health Services Committee. As that committee had been disbanded, consideration would require to be given to lines of accountability, reporting arrangements and links with other committees. With regard to business, it was felt that the focus of the CPG should be service provision and redesign. For agenda setting purposes, the following criteria were proposed: Issues should be identified as local, regional, tertiary or national. Proposals should be presented to the CPG in broad business case form. In some cases, the proposals should have been through other appropriate fora, eg new drugs requiring service change would have gone through the New Medicines Sub Group of the Area Drug and Therapeutics Committee. Proposals should have a clinical sponsor and they should present the case to the CPG. The financial considerations must be identified. The CPG may also commission specific pieces of work as appropriate and should have a close working relationship with the Planning Group and respond to the Planning Group request for a clinical opinion on submissions. It was proposed that meetings be held quarterly, additional meetings to be convened for urgent business as required. However, some members felt that the Group should meet more frequently, say every two months. Dr Bashford undertook to further refine the proposals relating to membership and organisational arrangements, taking into account the points raised during discussion, and would circulate these in advance of the next meeting for the Group’s consideration and agreement. 2 The Group Remitted to Ian Bashford to substantiate the proposals for membership and working arrangements for consideration and agreement. 3 MRI SERVICES, RAIGMORE HOSPITAL The Chair welcomed Dr Helen Shannon, Consultant Radiologist and Katherine Sutton, Superintendent Radiographer to the meeting. Dr Shannon spoke to the circulated business case for the provision of appropriate MRI scanning facilities to deliver Government waiting times targets, reducing access time for MRI scanning from 9 to 4 weeks by 31/03/09, and MRI imaging of an appropriate quality to allow the highest levels of diagnostic accuracy for MRI examinations of Highland patients. Timely MRI investigation was key to underpinning the proposed 18 weeks RTT plan. NHS Highland had also committed to a 2 week diagnostic waiting time for suspected cancer patients. This would require a significant increase in capacity to support the delivery of the targets and effective contingency arrangements to allow for predictable down time. The existing scanner had reached its technological limit, further upgrades were not an option. In addition, the advice of the College of Radiologists was that scanners should be replaced every 7 years and the existing machine had been installed in 2002/03. Dr Shannon confirmed that the Department of Radiology was developing an equipment replacement programme to ensure timely replacement of expensive items of equipment in the future. It had been their expectation that an updated MRI scanner would be required in the financial year 2009/10 to meet the increasing demands for scanning but also in terms of complexity of cases. Dr Shannon detailed activity and rising demand for services year on year – predicted to grow nationally at up to 15% per annum. It was noted that Highland provided services to Western Isles, while patients in Argyll and Bute were covered by an SLA with NHS Greater Glasgow & Clyde. To achieve and maintain a 9 week waiting time with one scanner, allowing for existing demand it would be necessary to extend the operational hours of the scanner to 72 hours per week. Discussions had taken place with staff regarding the possibility of extending the working day; however this would impact on their other commitments such as on call rotas. Extending the working day was one of seven options set out in the business case. Of these, Option 7- the provision of a second staffed MRI scanner within the MRI Department at Raigmore Hospital with the existing scanner continuing in use for more routine cases to the end of the 10 year term of its lease in 2012, was the preferred clinical option. This option would address clinical concerns over image quality, the limitations of the existing technology and also allow the building in of business continuity by having contingency MRI scanning services available. It would also allow the best quality of MRI scanning services to be provided for the Highland population. In addition, the two scanners could operate using a shared control room area, making more efficient use of staff. Dr Shannon indicated that despite running two scanners it was anticipated that the working day would require to be extended within the coming 2 – 3 years. John Cromarty enquired about activity in other boards in terms of utilisation of scanners and if there might be lessons to be learned from benchmarking. He also asked if any of the other options could be implemented more quickly, eg referral to other centres. It was noted that there was no spare capacity currently at any of the other Scottish centres. This option was also counter to the principle of treating patients as near to their home as possible and it could potentially impact on other specialist services in Highland. It was suggested that in order to maximise the use of the equipment, consideration should be given in the short term to restructuring the model of service, looking at skill mix, training requirements, increasing the staffing pool with the potential for shift work. 3 The paper also provided a financial evaluation, summarising the financial consequences of each of the purchase options over a 6 year period. Dr Shannon explained that lease options were not included in the paper, as they had proven not to be viable. She added that the Planning Group had asked for clarification on a number of the financial aspects of the case and she would be gathering some further information which she would also share with the Clinical Planning Group. The Group: 4 Agreed to clinically support the purchase of a second scanner as detailed in Option 7 of the business case on clinical grounds, noting that further financial clarification was being sought concerning purchase/lease options. Recommended that consideration be given in the short term to developing a mixed model of service with a view to maximising scanning resources. Recommended that the business case be re-referred to the Planning Group. MS TREATMENT – NATALIZUMAB (TYSABRI) The Chair welcomed Linda Kirkland, General Manager, Medical Directorate, who spoke to her circulated report. She explained that the paper and business case referred to Old Highland, essentially Raigmore patients, as the patient pathway for Argyll and Bute residents lay within NHS Greater Glasgow & Clyde. The paper outlined the advantages of Natalizumab. A resubmission of Natalizumab 300 mgs concentrated solution for infusion was considered by the Scottish Medicines Consortium (SMC) who gave a decision on the product on 10 August 2007. The SMC advises NHS Boards and Area Drug and Therapeutics Committees on its use in NHS Scotland. The advice is summarised as follows: “Natalizumab is accepted for restricted use within NHS Scotland as a single disease modifying therapy in highly active relapsing remitting multiple sclerosis (RRMS) only in patients with rapidly evolving severe RRMS, defined by two or more disabling relapses in one year and with one or more gadolinium-enhancing lesions on brain magnetic resonance imaging (MRI) or a significant increase in T2 lesion load compared with a previous MRI. In a post-hoc sub-group analysis of the pivotal trial, which included patients with rapidly evolving severe RRMS, it was associated with a significant reduction in the annualised relapse rate and the probability of a sustained progression of disability over two years compared with placebo.” The number of patients involved in NHS Old Highland would be small: there were currently approximately 70 patients in the SMC highly active relapsing remitting multiple sclerosis of whom approximately 22% would be eligible and suitable for the treatment. John Cromarty referred to the advice issued by the SMC and estimated that this may involve possibly five additional patients a year. As the prevalence of MS was evidently higher in the Highlands and Islands than elsewhere in Scotland, it was suggested that it might be useful to benchmark the prevalence in other Scottish Board areas and attempt to identify possible contributory factors. In response to a specific question, Professor Cromarty confirmed that horizon scanning in NHS Highland for new drugs coming on line was undertaken in conjunction with Pharmacy and Specialist Consultants projecting their potential requirements: two patients were identified in 07/08 and ten potentially for 08/09. 4 Where SMC approval had been given to a drug and there were no suitable alternative drugs, the Group were of the view that it was unnecessary for such cases to be submitted to it for clinical consideration. However, if there was some doubt surrounding the clinical case, the efficacy and cost-effectiveness, there were associated staffing or ancillary costs, and significant service redesign, then the Group agreed that it would be appropriate for consideration of such cases in order to provide a broader and more comprehensive clinical perspective. (Subsequent to the meeting, Professor Cromarty clarified that Natalizumab was not included in the Highland Joint Formulary. As it was now SMC approved, it was suggested that a Highland Joint Formulary application should be submitted, probably following consideration of this business case. Having considered the business case and the SMC advice, the Group agreed that the clinical case for Natalizumab within the SMC restricted use was clinically effective and sound.) There could also be potential savings in terms of social care and this issue could perhaps be raised with the Highland Council. The Group Remitted to Ian Bashford to convey its recommendation to the Planning Group that the clinical evidence for restricted use was sound and that the Planning Group should consider the case. 5 DVT The Group was advised that some further work required to be done on deep-veinous thrombosis throughout NHS Highland. Once this had been progressed, Maimie Thompson would prepare a comprehensive report for the Group’s consideration at a future meeting. 6 ANTICOAGULATION Dr Chris Lush spoke to the topic: Currently, the consultant haematologists undertook testing and dosing and there was a need to review the present service provision model and to review the clinical governance issues of providing a consistent and quality assured service Variations in testing and dosing arrangements existed throughout NHS Highland One model of redesign would be to consider transferring anticoagulation and monitoring to primary care: this would require a coordinated approach to ensure consistency of equipment, training and quality control for a standardised quality service. There would be resource implications for funding this technical service based within primary care and also remuneration for primary care staff. A wider discussion ensued and there was a significant number of models that needed to be considered for delivering this service across NHS Highland within primary care. The Group: Supported this early proposal in principle generally. Noted that there were a number of key actions required at an operational level to define the models for the process of implementation Suggested that a business case required to be completed and resubmitted. 5 7 FUTURE AGENDA ITEMS The following topics were agreed for future consideration: Clinical Planning Group working arrangements, agenda, links with other committees (next meeting) MRSA screening – a general update on the pilot screening sites currently, the principles of MRSA screening generally and any specific implications for NHS Highland (next meeting) DVT (future meeting) Diabetes Enhanced Service – a comprehensive update on proposed arrangements to consider moving the management of insulin-dependent diabetic patients into the primary care setting – this will require a comprehensive paper and clinical sponsorship (future meeting) 8 AOCB 8.1 Referral Prioritisation The Chair reported briefly on this issue raised by the Area Medical Committee. It related to GP referrals being made on patients to hospital consultants and the subsequent reprioritisation of the referral by hospital consultants. As this was involved with e-referral and online triage, the Chair indicated that he would pursue the issue within the eHealth Department of NHS Highland. He would report back to the Group on the outcome in due course. 9 SCHEDULE OF MEETINGS IN 2008 A proposed schedule of meetings for the remainder of the year was circulated for the Group’s agreement. It was suggested that meetings be held quarterly, however there was some feeling that more frequent meetings were required, say every two months. After discussion, the Group agreed the following dates for 2008:(Mondays, 2pm) 8 September 13 October 8 December The Group would give further consideration to the frequency of meetings in 2009. 10 DATE OF NEXT MEETING The next meeting would be held on Monday 8 September 2008 at 2.00pm in the Board Room, Assynt House. The meeting concluded at 4.30pm 6