Supplemental Digital Content

Supplemental Digital Content 1
Donor inclusions used for this study
We used the MP arm of the extended data set of our original study (376 recipients of a machine perfused kidney) (1). This extended set consists of the 336 DBD and DCD machine perfused kidney recipients who were included between November 1, 2005 and October 31,
2006 plus the machine perfused DCD kidney recipients who were included between
November 1, 2006 and August 17, 2007 following an amendment to the study protocol. This amendment is described in the Results section of the NEJM paper (pages 10 and 13), as well as in that paper’s figure 2, which shows subgroup analyses that were conducted on this extended data set of 752 recipients in total (i.e. 376 in the CS arm and 376 in the MP arm). All
376 recipients of machine perfused kidneys have therefore received a graft that was part of the same study, and those are exactly the kidneys that were also described in the NEJM paper. No additional inclusions were done solely for the biomarker analysis. For the present biomarker analysis, we chose to use this extended data set, as this would result in a superior statistical power to detect any effects, and there would be significantly more DCD kidney recipients to analyze (82 instead of 42). This higher percentage of DCD kidneys in the extended data set does also account for the somewhat higher overall DGF incidence in the extended data set versus the main data set of our RCT.
Biochemical analysis
LDH and ASAT were measured using standard automated clinical photometric kit assays on a
Modular P800 analyzer (kit category nrs. 04794940/04796217 and 04571100/04571118, respectively, Roche Diagnostics, Mannheim, Germany). The activity of GST was measured spectrophotometrically (Power Wave 200 Spectrophotometer, Bio-Tek Instruments,
1
Winooski, USA) at 340 nm via the conversion of 1-chloro-2,4-dinitrobenzene (CDNB) to glutathione-S-dinitrobenzene. The working substrate consisted of 0.1 ml of 100 mM CDNB added to 0.1 ml of 200 mM glutathione with 9.8 ml Dulbecco’s phosphate buffered saline.
The final pH of the reaction was set at 6.5. Calibration was performed with GST prepared from human placenta tissue (Sigma Aldricht, Zwijndrecht, The Netherlands). H-FABP was measured using a commercially available human H-FABP enzyme-linked immuno sorbent assay (ELISA) kit (Hycult Biotechnology, Uden, The Netherlands). Activity of Ala-AP and
NAG were measured using colorimetric assays (2). NAG was measured using a modified enzyme assay according to Findlay (3) at pH 4.25 using p -nitrophenylN -acetyl-β-Dglucosaminide as a substrate. Ala-AP was detected with the modified enzymatic assay of
Pfleiderer (4) using alaninep -nitroanilide as a substrate.
2
References
1. Moers C, Smits JM, Maathuis MH et al. Machine perfusion or cold storage in deceaseddonor kidney transplantation. N Engl J Med 2009; 360: 7.
2. van den Eijnden MM, Leuvenink HG, Ottens PJ et al. Effect of brain death and nonheart-beating kidney donation on renal function and injury: an assessment in the isolated perfused rat kidney. Exp Clin Transplant 2003; 1: 85.
3. Findlay J, Levvy GA, Marsh CA. Inhibition of glycosidases by aldonolactones of corresponding configuration. 2. Inhibitors of beta-N-acetylglucosaminidase. Biochem J
1958; 69: 467.
4. Pfleiderer G. Particle bound aminopeptidase from pig kidney. Methods in enzymology .
London: Academic Press, 1970: 514-521.
3
Table S1: Univariate characteristics of GST and H-FABP measured in donor plasma just before organ retrieval. Values are expressed as median (interquartile range).
Biomarker concentration in donor plasma:
Glutathione-S-transferase (U/l)
Heart-type fatty acid binding protein (pg/ml)
Biomarker concentration in donor plasma:
Glutathione-S-transferase (U/l)
Heart-type fatty acid binding protein (pg/ml)
Overall
252 (205–329)
2,272 (1,129–4,713) no DGF DGF
261 (207–342) 242 (192–300)
2,111 (1,128–4,907) 2,450 (1,168–4,359)
Table S2: Multivariate risk analysis (logistic regression model) for delayed graft function testing whether GST or H-FABP concentrations in donor plasma just before organ retrieval had any independent prognostic value for the risk of developing DGF after transplantation.
Other covariates in each model were: Renal vascular resistance at the end of MP
(mmHg/ml/min), donor age (yr), donor type (DCD vs. DBD), CIT (hr), the duration of prep-value
0.081
0.97 transplant dialysis (yr), the number of previous transplants of the recipient, recipient age (yr), and the number of HLA mismatches. In this table only the adjusted odds ratios and p-values for the biomarker of interest are shown.
Biomarker covariate
Risk of delayed graft function
(biomarker measured in donor plasma)
Glutathione-S-transferase (U/l)
Heart-type fatty acid binding protein (pg/ml)
Odds ratio
(95% CI)
1.00 (1.00–1.00)
1.00 (1.00–1.00) p-value
0.22
0.36
4
Table S3: Pearson’s correlation coefficients between the six biomarkers at the end of machine perfusion, and for each biomarker’s correlation with cold ischemic time (CIT) and renal vascular resistance (RR) at the end of machine perfusion. Numbers printed in bold indicate those correlations that were statistically significant (p<0.05).
CIT RR
LDH
ASAT
GST
Ala-AP
0.15
0.08
0.06
0.11
0.08
0.10
0.05
-0.08
NAG 0.11 0.08
H-FABP 0.03 <0.01
H-FABP
0.39
0.29
0.43
0.16
0.32
NAG
0.24
0.15
0.21
0.28
Ala-AP
0.08
0.09
0.15
GST
0.45
0.44
ASAT
0.56
5
600
400
200
0
0
800
600
400
200
0
0
5
5
LDH
10 15 pump time (h)
20 p=0.05
25
Ala-AP
10 15 pump time (h)
no DGF
no DGF
DGF
20
DGF p=0.62
25
50
40
30
20
10
0
0
3
2
1
0
0
ASAT
DGF
no DGF
5 10 15 pump time (h)
20 p=0.03
25
5
600
400
200
0
0
NAG
10 15 pump time (h)
6
no DGF
20
DGF p=0.01
25
12000
10000
8000
6000
4000
2000
0
0
GST
no DGF
5 10 15 pump time (h) p<0.0005
20 25
H-FABP
DGF
DGF
no DGF
5 10 15 pump time (h) p<0.0005
20 25
Figure S1: Evolution of each biomarker’s perfusate concentration in time split into kidneys that developed DGF and kidneys with immediate function. Lines are a least square fit to mean biomarker concentrations per time point after the initiation of MP, with gray lines drawn for kidneys with immediate function and black lines for kidneys that developed DGF. The baseline function used for each least square fit was a typical equation for molecular saturation in fluids: y = ax / (x + b), where a and b are determined by the least square method. Curves were corrected for outliers using Dixon’s Q test. P-values are the result of Mann-Whitney tests which compared the areas-under-the-curve per group.
7
600
400
200
0
0
800
600
400
200
0
0
5
5
LDH
10 15 pump time (h)
20 p=0.006
25
Ala-AP
10 15 pump time (h)
20
DCD
DBD
DBD
DCD p=0.09
25
50
40
30
20
10
0
0
3
2
1
0
0
ASAT
600
DCD
400
5
DBD
10 15 pump time (h) p<0.0005
20 25
200
0
0
5
NAG
DCD
DBD
10 15 pump time (h)
8
20 p=0.001
25
12000
10000
8000
6000
4000
2000
0
0
GST
DBD
5 10 15 pump time (h) p<0.0005
20 25
H-FABP
DCD
DCD
DBD
5 10 15 pump time (h)
20 p=0.005
25
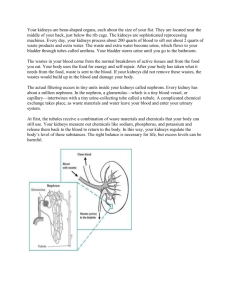
Figure S2: Evolution of each biomarker’s perfusate concentration in time split into kidneys recovered from DBD and kidneys recovered from
DCD. Lines are a least square fit to mean biomarker concentrations per time point after the initiation of MP, with gray lines drawn for DBD kidneys and black lines for DCD kidneys. The baseline function used for each least square fit was a typical equation for molecular saturation in fluids: y = ax / (x + b), where a and b are determined by the least square method. Curves were corrected for outliers using Dixon’s Q test. Pvalues are the result of Mann-Whitney tests which compared the areas-under-the-curve per group.
9
10
Figure S3: Kaplan-Meier plots of one year death censored graft survival split at each biomarker’s median value. Logrank tests showed that all p-values for the difference between each pair of survival curves were above 0.05. Vertical lines indicate cases that were censored upon death with a functioning graft.
11