Assessment 7 Dermatology
advertisement
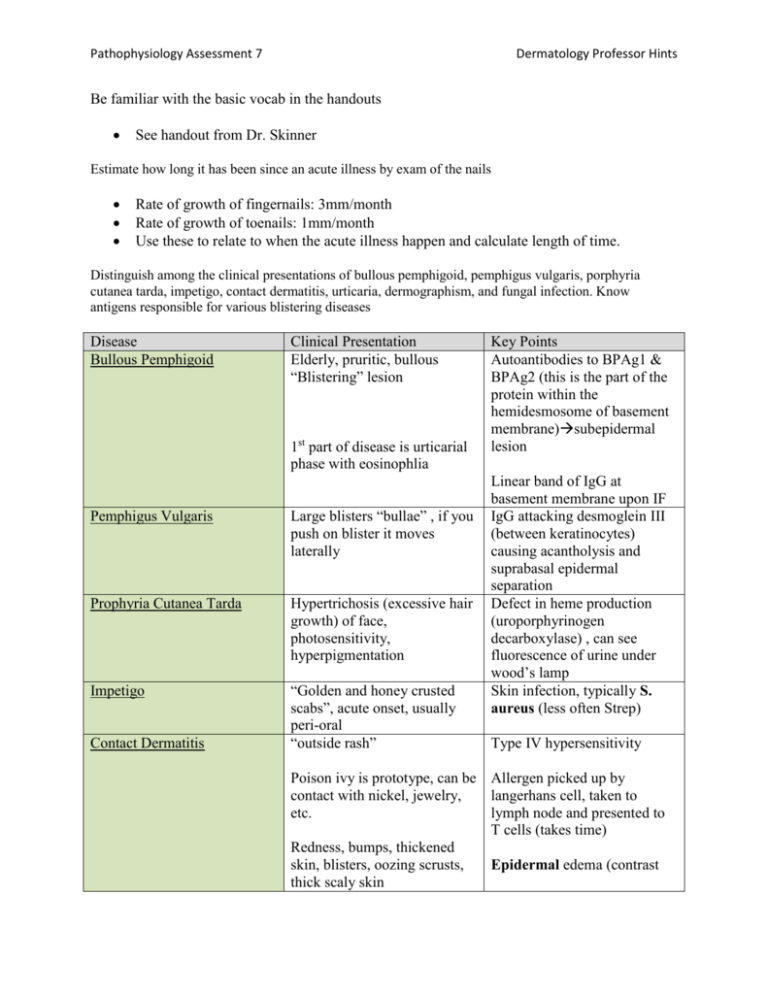
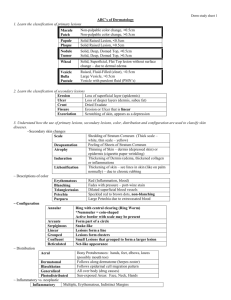
Pathophysiology Assessment 7 Dermatology Professor Hints Be familiar with the basic vocab in the handouts See handout from Dr. Skinner Estimate how long it has been since an acute illness by exam of the nails Rate of growth of fingernails: 3mm/month Rate of growth of toenails: 1mm/month Use these to relate to when the acute illness happen and calculate length of time. Distinguish among the clinical presentations of bullous pemphigoid, pemphigus vulgaris, porphyria cutanea tarda, impetigo, contact dermatitis, urticaria, dermographism, and fungal infection. Know antigens responsible for various blistering diseases Disease Bullous Pemphigoid Clinical Presentation Elderly, pruritic, bullous “Blistering” lesion 1st part of disease is urticarial phase with eosinophlia Pemphigus Vulgaris Large blisters “bullae” , if you push on blister it moves laterally Prophyria Cutanea Tarda Hypertrichosis (excessive hair growth) of face, photosensitivity, hyperpigmentation Impetigo “Golden and honey crusted scabs”, acute onset, usually peri-oral “outside rash” Contact Dermatitis Key Points Autoantibodies to BPAg1 & BPAg2 (this is the part of the protein within the hemidesmosome of basement membrane)subepidermal lesion Linear band of IgG at basement membrane upon IF IgG attacking desmoglein III (between keratinocytes) causing acantholysis and suprabasal epidermal separation Defect in heme production (uroporphyrinogen decarboxylase) , can see fluorescence of urine under wood’s lamp Skin infection, typically S. aureus (less often Strep) Type IV hypersensitivity Poison ivy is prototype, can be Allergen picked up by contact with nickel, jewelry, langerhans cell, taken to etc. lymph node and presented to T cells (takes time) Redness, bumps, thickened skin, blisters, oozing scrusts, Epidermal edema (contrast thick scaly skin Pathophysiology Assessment 7 Dermatology Professor Hints with urticaria) Urticaria “inside rash”, transient, itchy, edematous, lightly erythematous, papules or wheals with central clearing. *Streaks and blisters are characteristic of plant dermatitis (teacher said to know this for exam) Dermal edma, Type 1 hypersensitivity, IgE mediated, hives, etc. Can be due to drugs, foods, malignancy, etc. Dermographism Complaint of itching, when skin is scratched hives show up Fungal Infection (dermatophyte) Tinea’s Don’t order random lab tests, maybe a CBC, ESR, and relevant chemistry panel Normal skin, but when scratched produces hives (we perform this and we have the diagnosis) Tinea pedis: Athletes foot Tinea cruris: Jock itch Tina corpora: Ringworm of body Tinea capitis: infected hair shafts on scalp Tinea unguium: Nails Know dx criteria for atopic dermatitis Pruiritic skin disease of uknown origin typified by pruitus, eczematous lesions, xerosis “The itch that rashes” Acute, eczematous, crusted scaly plaques, marked by excoriation Facial and extensor involvement in infants, flexor involvement in adults (very testable) Major criteria o Pruitis Pathophysiology Assessment 7 Dermatology Professor Hints o Morphology & Distribution Flexor adults Extensor/facial in infants o Relapsing dermatitis o History of dermatitis Minor criteria o Dennie morgan folds under eyelid o o o o Pityrasis alba (ill defined patches on cheeks and skin) Icthyosis (fish scaled appearance on lower extremities) Hyperlinear palms (marked skin lines on palms) Keratosis pilaris (lateral aspect of arms and legs are hyperkeratotic, papules around hair follicles) Know causes (and clinical presentations thereof) of alopecia Androgenic Alopecia o Common baldness o Gradual miniaturization of hairs with transformation of large terminal follicles into small ones o Dependent on DHT o Men: Frontotemporal recession, women at the crown of scalp o Treat with minoxidil or fenasteride o Propecia inhibits Type 2 5-alpha reductase Telegen Effluvium o Excess of hair shunted into telogen phase from anagen o Pregnancy is the prototype Anagen Effluvium o Drugs can cause, effects 80-90% of hair Alopecia Areata o Circular areas of complete hair loss with normal scalp o Nail pitting associated with this (know this) o Lymphocytic infiltrate, immunological process Traction alopecia o Use or rollers, combs, etc. Folliculitis o S. Aureus is main cause (know this) o Inflammation of opening of hair follicle o Less often caused by pityrosporum Pathophysiology Assessment 7 Dermatology Professor Hints Know epidemiology of squamous cell, basal cell and melanoma. Distinguish among them by appearance (description). Know common sites for metastasis, genetic and viral associations Cancer Squamous Cell Carcinoma (SCC) Epidemiology Associated with cumulative sun exposed, Appearance/Description/Associations Associated with stratum spinosum keratinocytes Risk factors: p53 mutation UV, HPV, chronic inflammation, burns, arsenic, radiation, leukoplakia Metastasis to lymph nodes and lung* Nests of tumor cells, keratin pearls Basal Cell carcinoma (BCC) **Most common neoplasm in United States PCTH Mutation (SHH /SMO pathway) Risk factors: “Pearly border and telangiectasia” UV, fair complexion, sunburns, FH, immunosuppression (10x increase) Metastasis is rare* Histologically can have different subtypes (looks more basophilic histologically (purple), palisading Pathophysiology Assessment 7 Dermatology Professor Hints basal cells form nests with clefting) Melanoma Environment and genetic predispositions Nodular: no radial growth phase, superficial: more radial growth, pigmented has dark spots, mopheaform has flatter more sclerotic appearance CDK2N (more familial), BRAF mutation Acral lentiginous melanoma most common in dark skinned patients melanoma under nails and on soles of feet Assymetric Lentigo malignamelanoma in situ in older individuals (remember lentigo is just liver spots, lentigo maligna is melanoma in situ transposed on a lentigo) Diameter >6mm Border Irregularity Color Irregularity *Ugly duckling sign is buzzword for melanoma according to Dr. Kennedy (one mole looks different than rest) Nodular melanoma (starts off in vertical phase) According to PaPh 50% develop from nevi, does not correlate to all sources I’ve read. First radial growth phase, then vertical (vertical has poor prognosis based on depth) Lymph node involvement is #1 prognostic factor, based on initial Pathophysiology Assessment 7 Dermatology Professor Hints biopsy however it is depth of vertical growth Know pathophys of warts, treatment thereof Caused by HPV, virus inoculated by defects in epithelium Condylomata accuminata o HPV 6,11 (low risk for cancer), 16 and 18 high risk Flat warts can be spread by shaving Treatment o Duct tape, salicyclic acid, liquid nitrogen, TCA, cantharidin, podophylin, laser, imiquimod (promotes innate immunity), oral cimetidine, intralesional candida antigen Know exacerbating factors of acne Disorder of pilo-sebaceous units Plugging of follicular hole Exacerbating factors o Increased testosterone causing increased sebum secretion (androgen receptors on sebaceous glands) o Mechanical irritation o Greasy occlusive products o Hyperandrogenic states Polycystic ovarian disease Virilizing tumors Congenital adrenal hyperplasia o Steroids can induce acne (especially on back/upper trunk)