Antimalarial drugs
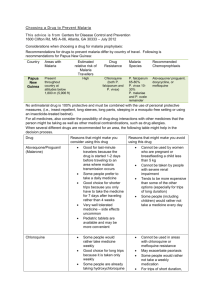
advertisement
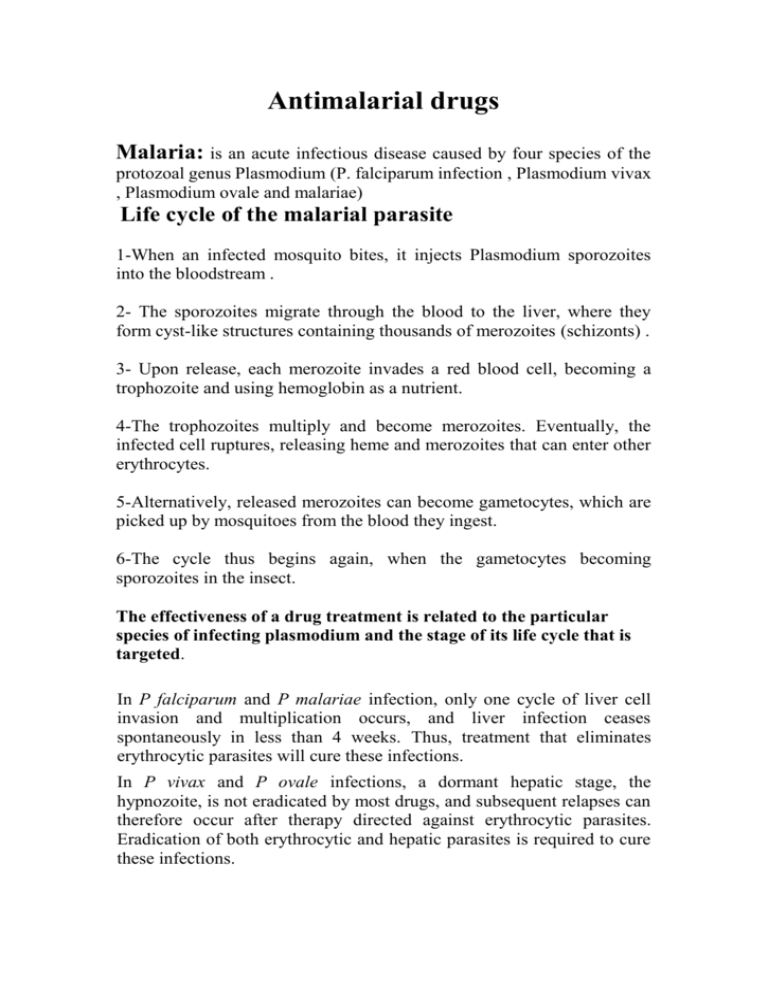
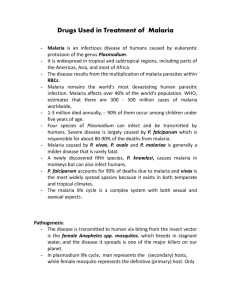
Antimalarial drugs Malaria: is an acute infectious disease caused by four species of the protozoal genus Plasmodium (P. falciparum infection , Plasmodium vivax , Plasmodium ovale and malariae) Life cycle of the malarial parasite 1-When an infected mosquito bites, it injects Plasmodium sporozoites into the bloodstream . 2- The sporozoites migrate through the blood to the liver, where they form cyst-like structures containing thousands of merozoites (schizonts) . 3- Upon release, each merozoite invades a red blood cell, becoming a trophozoite and using hemoglobin as a nutrient. 4-The trophozoites multiply and become merozoites. Eventually, the infected cell ruptures, releasing heme and merozoites that can enter other erythrocytes. 5-Alternatively, released merozoites can become gametocytes, which are picked up by mosquitoes from the blood they ingest. 6-The cycle thus begins again, when the gametocytes becoming sporozoites in the insect. The effectiveness of a drug treatment is related to the particular species of infecting plasmodium and the stage of its life cycle that is targeted. In P falciparum and P malariae infection, only one cycle of liver cell invasion and multiplication occurs, and liver infection ceases spontaneously in less than 4 weeks. Thus, treatment that eliminates erythrocytic parasites will cure these infections. In P vivax and P ovale infections, a dormant hepatic stage, the hypnozoite, is not eradicated by most drugs, and subsequent relapses can therefore occur after therapy directed against erythrocytic parasites. Eradication of both erythrocytic and hepatic parasites is required to cure these infections. Drugs is classified into 3 types: 1-Drugs that eliminate developing or dormant liver forms are called tissue schizonticides.e.g. primaquine 2- those that act on erythrocytic parasites are blood schizonticides.e. g. chloroquine, mefloquine,quinine and pyrimethamine 3-those that kill sexual stages and prevent transmission to mosquitoes are gametocides e.g. quinine,chloroquine and primaquine No one available agent can reliably effect a radical cure, ie, eliminate both hepatic and erythrocytic stages. Few available agents are causal prophylactic drugs, ie, capable of preventing erythrocytic infection. However, all effective chemoprophylactic agents kill erythrocytic parasites before they increase sufficiently in number to cause clinical disease. Tissue schizonticide: Primaquine Clinical indications: 1-eradicates primary exoerythrocytic forms of P. falciparum and P. vivax. 2- eradicates secondary exoerythrocytic forms of recurring malarias (P. vivax and P. ovale),so primaquine is the only agent that can lead to radical cures of the P. vivax and P. ovale malarias, which may remain in the liver in the exoerythrocytic form after the erythrocytic form of the disease is eliminated. 3-The sexual (gametocytic) forms of all four plasmodia are destroyed in the plasma or are prevented from maturing later in the mosquito, thus interrupting the transmission of the disease. Note: Primaquine is not effective against the erythrocytic stage of malaria and, therefore, is often used in conjunction with a blood schizonticide, such as chloroquine, quinine, mefloquine, or pyrimethamine. Mechanism of action: This is not completely understood. Metabolites of primaquine are believed to act as oxidants that are responsible for the schizonticidal action. Adverse effects: Primaquine has a low incidence of adverse effects, except for druginduced hemolytic anemia in patients with genetically low levels of glucose-6-phosphate dehydrogenase.. Blood schizonticide: 1.Chloroquine Clinical indications: 1-Chloroquine has been the mainstay of antimalarial therapy, and it is the drug of choice in the treatment of erythrocytic forms of plasmodia., except in resistant strains. 2- Chloroquine is also effective in the treatment of gametocytes. Mechanism of action: 1-Damage to parasite mediated by accumulated heme. 2-Alkinization of food vacuole. 3-Decreased DNA synthesis. Adverse effects: 1-Side effects are minimal at the low doses used in the chemo suppression of malaria. .2- At higher doses, many more toxic effects occur, such as gastrointestinal upset, pruritus, headaches, and blurring of vision . Note: An ophthalmologic examination should be routinely performed. 3-Chloroquine should be used cautiously in patients with hepatic dysfunction or severe gastrointestinal problems or in patients with neurologic or blood disorders. 4-Chloroquine can cause electrocardiographic changes, because it has a quinidine-like effect. Resistance: Resistance of plasmodia to available drugs has become a serious medical problem throughout Africa, Asia, and most areas of Central and South America. Chloroquine-resistant P. falciparum exhibit multigenic alterations that confer a high level of resistance. Note: When a chloroquine-resistant organism is encountered, therapy usually consists of an orally administered combination of quinine, pyrimethamine, and a sulfonamide, such as sulfadoxine. 2. mefloquine Clinical indication: Mefloquine is used for infections caused by multidrug-resistant forms of P. falciparum. Mechanism of action: remains to be determined, but like quinine, it can apparently damage the parasite's membrane. Adverse reactions; at high doses range from nausea, vomiting, and dizziness to disorientation, hallucinations, and depression. 2-Electrocardiographic abnormalities and cardiac arrest are possible if mefloquine is taken concurrently with quinine or quinidine. 3.Quinine and quinidine Clinical indications: These drugs are reserved for severe infestations and for malarial strains that are resistant to other agents, such as chloroquine. Mechanisim of action: Quinine and its stereoisomer, quinidine , interfere with heme polymerization, resulting in death of the erythrocytic form of the plasmodial parasite. Adverse effect : 1-Cinchonism a syndrome causing nausea, vomiting, tinnitus, and vertigo. These effects are reversible and are not considered to be reasons for suspending therapy. 2-However, quinine treatment should be suspended if a positive Coombs' test for hemolytic anemia occurs. Drug interactions include potentiation of neuromuscular-blocking agents and elevation of digoxin levels if taken concurrently with quinine. Blood schizonticide and sporontocide: Pyrimethamine 1-The antifolate agent pyrimethamine is frequently employed to effect a radical cure as a blood schizonticide. 2-It also acts as a strong sporonticide in the mosquito's gut when the mosquito ingests it with the blood of the human host. Mechanisim of action: Pyrimethamine inhibits plasmodial dihydrofolate reductase at much lower concentrations than those needed to inhibit the mammalian enzyme. Clinical indications; 1-Pyrimethamine alone is effective against P. falciparum.(treatment of acute attack and prophylaxis). 2- In combination with a sulfonamide sulfadoxine(fansider), is also used against P. malariae .It cause megaloblastic anemia. Exercise one: match anti-malarial drugs with side effect? 1-quinidine haemolytic anemia in patient with G-6-P-D deficiency. 2-Pyrimethamine disorientation, hallucinations, and depression. 3- mefloquine. Cinchonism a syndrome 4-Primaquine blurring of vision . 5-Chloroquine megaloblastic anemia Exercise two: match anti-malarial drugs with site of action? 1-quinidine tissue schizonticides 2-Pyrimethamine blood schizonticides 3- mefloquine. gametocides 4-Primaquine Blood schizonticide and sporontocide 5-Chloroquine Exercise three: match anti-malarial drugs with mechanism of action? 1-quinidine inhibit plasmodial dihydrofolate reductase 2-Pyrimethamine Damage to parasite mediated by accumulated heme. 3- mefloquine. act as oxidants that are responsible for the schizonticidal action. 4-Primaquine damage the parasite's membrane. 5-Chloroquine interfere with heme polymerization