Follicular carcinoma
advertisement
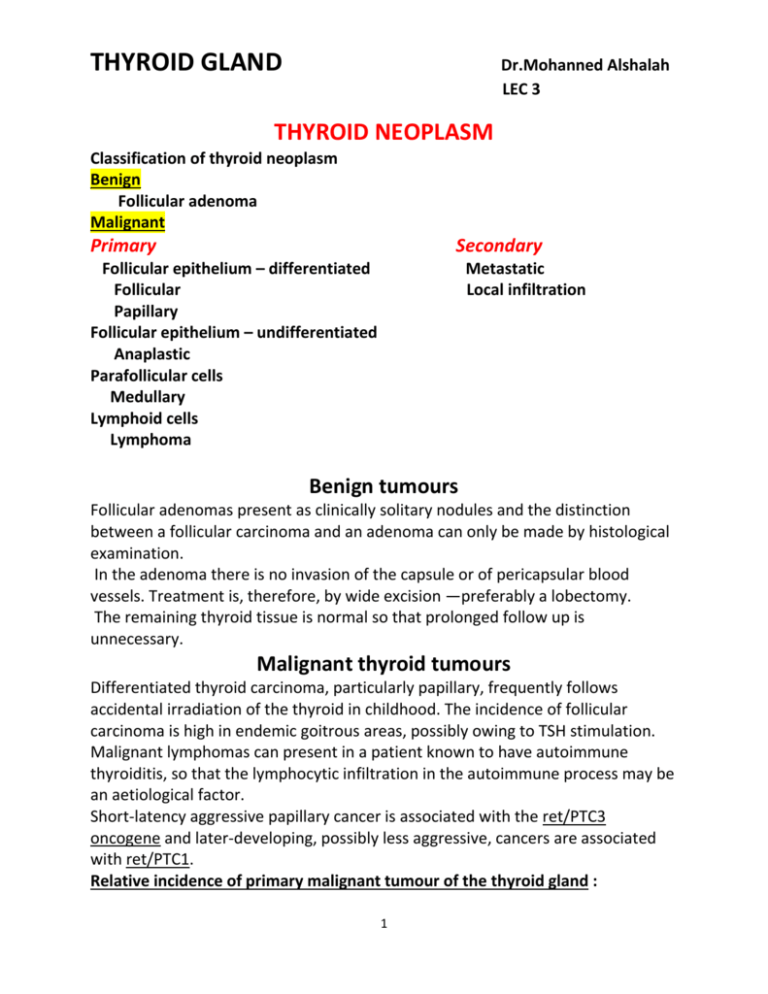
THYROID GLAND Dr.Mohanned Alshalah LEC 3 THYROID NEOPLASM Classification of thyroid neoplasm Benign Follicular adenoma Malignant Primary Secondary Follicular epithelium – differentiated Follicular Papillary Follicular epithelium – undifferentiated Anaplastic Parafollicular cells Medullary Lymphoid cells Lymphoma Metastatic Local infiltration Benign tumours Follicular adenomas present as clinically solitary nodules and the distinction between a follicular carcinoma and an adenoma can only be made by histological examination. In the adenoma there is no invasion of the capsule or of pericapsular blood vessels. Treatment is, therefore, by wide excision —preferably a lobectomy. The remaining thyroid tissue is normal so that prolonged follow up is unnecessary. Malignant thyroid tumours Differentiated thyroid carcinoma, particularly papillary, frequently follows accidental irradiation of the thyroid in childhood. The incidence of follicular carcinoma is high in endemic goitrous areas, possibly owing to TSH stimulation. Malignant lymphomas can present in a patient known to have autoimmune thyroiditis, so that the lymphocytic infiltration in the autoimmune process may be an aetiological factor. Short-latency aggressive papillary cancer is associated with the ret/PTC3 oncogene and later-developing, possibly less aggressive, cancers are associated with ret/PTC1. Relative incidence of primary malignant tumour of the thyroid gland : 1 THYROID GLAND Dr.Mohanned Alshalah LEC 3 Papillary carcinoma 60 % Follicular carcinoma 20% Anaplastic carcinoma 10% Medullary carcinoma 5% Malignant lymphoma 5% Diagnosis of thyroid neoplasm Diagnosis is obvious on clinical examination in most cases of anaplastic carcinoma, although Riedel’s thyroiditis is indistinguishable. It is not always easy to exclude a carcinoma in a multinodular goitre, and solitary nodules, particularly in a young male patient, are always suspect. FNAC in preoperative diagnosis has an important value. Incisional biopsy may cause seeding of cells and local recurrence and is not advised in a resectable carcinoma. In an anaplastic and obviously irremovable carcinoma, however, incisional or core needle biopsy is justified. When a preoperative diagnosis is made, imaging with ultrasound, MRI or CT is required for the assessment of the extent of the primary tumour. Imaging provides valuable information on nodal involvement, which permits preoperative planning for nodal dissection. Frozen section histology has a limited role in thyroid surgery. It cannot reliably differentiate between encapsulated benign and malignant follicular neoplasms and is of more value in confirming whether nodes are involved with papillary cancer, thereby influencing the extent of nodal surgery. Papillary carcinoma Most papillary tumours contain a mixture of papillary and colloid- filled follicles. Histologically the tumour shows papillary projections and characteristic pale empty nuclei (Orphan Annie-eyed nuclei). Papillary carcinomas are very seldom encapsulated. foci may occur in the same lobe as the primary tumour or, less commonly, in both lobes. They may be due to lymphatic spread in the rich intrathyroidal lymph plexus or to multicentric growth. Spread to the lymph nodes is common but blood-borne metastases are unusual unless the tumour is extrathyroidal. The term extrathyroidal indicates that the primary tumour has infiltrated through the capsule of the thyroid gland, although 2 THYROID GLAND Dr.Mohanned Alshalah LEC 3 minimal invasion of the sternothyroid muscle is much less significant than infiltration into the oesophagus or trachea. The term ‘occult carcinoma’ is applied to all papillary carcinomas less than 1 cm in diameter. These have a uniformly excellent prognosis although those presenting with nodal or distant metastases justify more aggressive therapy. Follicular carcinoma These appear to be macroscopically encapsulated but microscopically, there is invasion of the capsule and of the vascular spaces in the capsular region. Multiple foci are seldom seen and lymph node involvement is much less common than in papillary carcinoma. Blood-borne metastases are more common and the eventual mortality rate is twice that of papillary cancer. Hurthle cell tumours are a variant of follicular neoplasm in which oxyphil (Hurthle, Askanazy) cells predominate histologically. Hurthle cell cancers are associated with a poorer prognosis. Prognosis in differentiated thyroid carcinoma Compared with most cancers the prognosis in differentiated thyroid carcinoma is excellent. Although influenced by histological type, prognosis is much more dependent on age at diagnosis, size of the tumour, metastatic disease and the presence of either extrathyroidal spread (in papillary cancer) or major capsular transgression (in follicular carcinoma). Tumour–node–metastasis staging of thyroid cancer?? Surgical treatment The conservative approach advocates lobectomy with isthmusectomy in most patients with total thyroidectomy reserved for specific indications (those with bilateral disease or judged to be in a high-risk category). The more radical approach advocates routine total thyroidectomy often as a staged procedure depending on the pathological findings of the initial lobectomy. Additional measures 3 THYROID GLAND Dr.Mohanned Alshalah LEC 3 Thyroxine; It is standard practice to prescribe thyroxine (0.1–0.2 mg daily) for all patients after operation for differentiated thyroid carcinoma to suppress endogenous TSH production. Thyroid hormone replacement is obviously necessary after total thyroidectomy and in the majority of patients after near total thyroidectomy, and is usually given in the form of thyroxine. Radioiodine; If metastases take up radioiodine they may be detected by scanning and may be treated with large doses of radioiodine. For effective scanning, all normal thyroid tissue must have been ablated, either by surgery or preliminary radioiodine, and the patient must be hypothyroid to improve uptake. Alternatively, synthetic recombinant TSH may be used to stimulate uptake. Patients who require repeated radioiodine administration for scanning and therapy, should be given tri-iodothyronine (40–60 μg daily–1) because it is much shorter acting and, on stopping it, increased TSH secretion and thyroid avidity for iodine recover quickly so that radioiodine may be given after several days. The patient is thereby spared weeks of developing thyroid insufficiency after stopping thyroxine before radioiodine may be given. Thyroglobulin; The measurement of serum thyroglobulin is of value in the followup and in the detection of metastatic disease in patients who have undergone surgery for differentiated thyroid cancer. This measurement may obviate the need for serial radioactive iodine scanning but when a rise occurs, a scan will be indicated to confirm and locate the metastatic disease. Undifferentiated (anaplastic) carcinoma This occurs mainly in elderly women. Local infiltration is an early feature of these tumours with spread by lymphatics and by the bloodstream. They are extremely lethal tumours and survival for more than 1—2 years after presentation is most unusual. Many of these aggressive lesions present in an advanced stage with tracheal obstruction and require urgent tracheal decompression. The trachea may be decompressed and tissue obtained for histology by isthmusectomy. Tracheostomy is best avoided.Radiotherapy should be given in all cases and may provide a worthwhile period of palliation as may combination chemotherapy. Medullary carcinoma 4 THYROID GLAND Dr.Mohanned Alshalah LEC 3 These are tumours of the parafollicular (C)-cells derived from the neural crest. High levels of serum calcitonin and carcinoembryonic antigen are produced by many medullary tumours. These levels fall after resection of a tumour and will rise again if the tumour recurs. This is a valuable tumour marker in the follow-up of patients with this disease. Diarrhoea is a feature in 30 per cent of cases and this may be due to 5-hydroxytryptamine or prostaglandins produced by the tumour cells. Some tumours are familial and may account for 10—20 per cent of all cases. Medullary carcinoma may occur in combination with adrenal phaeochromocytoma and hyperparathyroidism in the syndrome known as multiple endocrine neoplasia type IIa (MEN IIa). The familial form of the disease frequently affects children and young adults whereas the sporadic cases occur at any age with no sex predominance. When the familial form is associated with prominent mucosal neuromas involving the lips, tongue and inner aspect of the eyelids, with occasionally a Marfanoid hahitus, the syndrome is referred to as MEN type IIb. Treatment is by total thyroidectomy and either prophylactic or therapeutic resection of the central and bilateral cervical lymphnodes. Familial cases are now detected by genetic screening for the RET oncogene mutations which identifies individuals who will develop medullary cancer later in life. The genetic tests are supplemented by estimating serum calcitonin levels in the basal state and after stimulation by either calcium or pentagastrin. A rise in calcitonin levels under these circumstances should lead to a prophylactic thyroidectomy. Phaeochromocytoma must be excluded by measurement of urinary catecholamine levels in all cases before embarking upon thyroid surgery to avoid the potential hazards associated with this condition. Malignant lymphoma The response to irradiation is good and radical surgery is unnecessary once the diagnosis is established by biopsy. (Trucut) or open biopsy is usually necessary. The prognosis is good if there is no involvement of cervical lymph nodes. Rarely, the tumour is part of widespread malignant lymphoma disease, and the prognosis in these cases is worse. 5