Title: Reproductive and Maternal Health Supplies in Tanzania
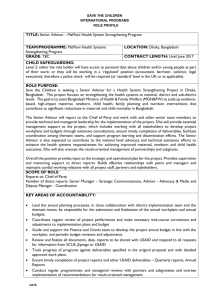
advertisement

Business Case and Intervention Summary Title: Reproductive and Maternal Health Supplies in Tanzania Acronyms ADC ADS AIDS AM A/OTAR BCC CBM CIB CIDA CO2 COTAR CPR CSC CYPs DALYs DFID DMOs DPs EMoc FBO FP GAAP GBS GOT HIV HQ IC I/E IEC ILS IP IRR KPIs IUDs JSI KFW LAPM MCH MDGs MDT M&E MIS MOHSW MKUKUTAII MOU MSD MSI MST MTEF Arrangement of Delegated Cooperation Automated Directive System Acquired immune deficiency syndrome Activity Manager Agreement Officers’ technical representative Behaviour change communication Community-based mobiliser Contract Information Bulletins Canadian International Development Agency Carbon dioxide Contract Officer Technical representative Contraceptive prevalence rate Critical Success Criteria Couple Years of Protection Disability Assisted Life Years Department for International Development District Medical Offices Development Partners Emergency Obstetric care Faith-based organisation Family planning Generally Accepted Accountancy Principles General budget support Government of Tanzania Human Immune deficiency virus Headquarters MSI Impact Calculator Income/expenditure Information, Education, and Communication Integrated logistic system Infection prevention Internal Rate of Return Key performance indicators Inter-uterine device John Snow International German Development Agency Long-acting and permanent methods (of FP) Maternal and child health Millennium development goals MSI Medical development team Monitoring and evaluation Management information system Ministry of Health and Social Welfare Tanzanian poverty reduction strategy Memorandum of Understanding Medical Stores Department Marie Stopes International Marie Stopes Tanzania Medium-term expenditure framework NFP CIP NGOS NPV OMB PFM PMP PMTCT PPRA PPA PSI PSU QTA RCHS REDD R&R form RH RMH SIFPO-MSI SORP SRH SWAP TDHS TFDA TRCHS USAID VCT VFM National family planning costed implementation plan Non-governmental organisation Net Present Value Office of Management and Budget Performance and financial management Performance Management Plan Preventing maternal-to-child transmission Procurement Regulatory Authority Programme Partnership Agreement Population Services International Pharmaceutical Services Unit Quality technical assessment Reproductive and Child Health Services Reducing emissions from deforestation & degradation Report and request form Reproductive health Reproductive and maternal health Support for international FP-MSI Statement of recommended accounting practice Sexual and reproductive health Sector-wide approach Tanzanian Demographic and Health Survey Tanzania Food and Drug Authority Tanzania Reproductive Child Health Survey US Agency for International Development Voluntary counselling and testing (for HIV) Value for money Intervention Summary What support will the UK provide? UK government will provide £5m per year for three years. This should ensure adequate supplies of essential medications for ante natal care and safe deliveries across the country, and adequate resources for contraceptive implants, which offer women effective long acting protection from pregnancy. Why is UK support required? Tanzania’s progress in reducing maternal mortality is slow. The last estimate was that 440 women die for every 100 000 pregnancies. About a third of these deaths could be prevented, if women who do not want to get pregnant are able to access effective contraception. To prevent the other two thirds of deaths requires a ‘safe delivery’. Although there has been significant investment in improving safe motherhood, and now over half of the women give birth in health facilities, almost all such facilities currently lack basic life saving drugs. By providing long term contraceptives, this project will really help rural women who find it difficult and expensive to access effective health services on a frequent basis. Choice over when to have children not only improves the woman’s life, it increases the health and life chances of existing children as well. Maternal health drugs decrease the risks of death from haemorrhage and high blood pressure, as well as other complications resulting from anaemia and malaria. Women are more likely to give birth in a health facility if it is known to have adequate supplies of drugs. Providing the commodities alone however is not enough – so this project will also offer support to supply chain and policy development, so that the commodities are appropriately stored, distributed and used. Providing effective contraceptives and life saving drugs is a core function of the health system – the project will therefore work at a policy level to build capacity and increase commitment to ensuring that government takes on this responsibility as a key component of ensuring women’s health and survival. The project will be implemented through USAID, who are the lead development partners in this area in the country. What are the expected results? The impact of this programme is to reduce maternal deaths and contribute to achieving Millennium Development Goal 5. The outcome is to ensure that family planning and maternal health supplies are available in Tanzania throughout the health system. The key changes which are expected to result from the support include: prevent the deaths of at least 1280 Tanzanian women by improving the quality of antenatal care and deliveries across the whole of Tanzania provide 250,000 contraceptive implants per year which will contribute to 400 couple years of protection (This in turn will avert 140 000 unwanted pregnancies 20 000 unsafe abortions and 490 maternal deaths) provide drugs used antenatally to prevent malaria and anaemia, and drugs used around the time of delivery to prevent haemorrhage and eclampsia strengthen Government of Tanzania’s drug management and distribution system, and support policies for improved use. Business Case Strategic Case A. Context and need for a DFID intervention RATIONALE Maternal mortality is high in Tanzania, and safe delivery care needs to be available to all women in childbirth as well as access to family planning.i Both safe delivery care and family planning in Tanzania are hampered by a lack of reproductive and maternal health (RMH) supplies in the facilities where they are neededii. The understanding of how critical these supplies are to good development outcomes is growing internationally. DFID has not had a health programme in Tanzania for some time and working in RMH supplies (where there are clear gaps) is an area where the need is great and DFID can quickly make a difference without large staff investment. Family planning. Increasing access to family planning could reduce maternal mortality in Tanzania by as much as one third by reducing the number of births and a woman’s exposure to the risk of dying. In addition, family planning increases birth spacing between children, which increase survival for both the child born and the older sibling. Between 2005 and 2010 there has been a significant increase in use of family planning from 26 to 34% (married women using modern contraception). This momentum needs to be maintained. Maternal health care. A functioning health system is required to deliver safe delivery care. Part of a functioning health system is to provide the necessary equipment and supplies to deliver these services. There are shortages of maternal health supplies within the Tanzanian health system with considerable anecdotal evidence of widespread stockouts of maternal health supplies in all districts of Tanzania. To begin to understand the situation better, USAID has just carried out a quantification of drugs for maternal health which indeed revealed serious shortages. Without commodities the gains from investments in training and other elements of service delivery will not be realised and women will continue to die in childbirth. Drug availability is one of the key indicators of quality that women have when assessing health services. Without a reliable consistent supply of supplies, maternal and reproductive health services will not be delivered. The Development Partners must work together to encourage greater political commitment and investment in these areas to ensure the family planning programme sustainability. Other donors with in-depth knowledge and years of experience working on RMH are working to strengthen service delivery and support contraceptive social marketing. Given DFID’s current plan to keep its health programme slim and focused on tangible impact, supporting supplies is a good strategic niche for DFID. Buying supplies allows DFID to make a real impact on Tanzania’s health programme without the need for major staff input. DFID is already funding Marie Stopes International Tanzania (MST) to deliver muchneeded family planning outreach services in rural areas. The regionally-funded Evidence for Action in Maternal Health (E4A) is beginning work in Tanzania in early 2012. This new business case on RMH supplies will build links with the work of MST and E4A. CONTEXT High maternal mortality. Maternal and infant mortality remain high in Tanzania, especially in rural areas. The maternal mortality ratio is 454 deaths per 100,000iii live births (2010). This is a non significant fall from 578iv (2005). Maternal health is affected by the poor coverage, poor quality services and a high unmet need for contraception. Access to RMH services is critical to Tanzania’s development. Without it, the Millennium Development Goals (MDGs) cannot be met. High fertility levels are a challenge to development. The total fertility rate (the number of children the average woman bears) in Tanzania is 5.4 - with levels of 6.1 in rural areasv. The population of Tanzania is scheduled to grow to 69 m by 2050 vi from its current 46 million. This will put real pressure on food and water resources in some parts of the country and on the provision of basic services. However, significant progress has been made over the last decade in scaling up family planning programmes. Trends in Contraceptive Use: Tanzania Percent of currently married women TDHS 1991-92 TDHS 1996 TRCHS 1999 THDS 2004-05 TDHS 2010 34 25 27 26 20 18 17 13 10 9 7 4 Any method Any modern method 5 6 7 Any traditional method Progress: DFID contribution last year is credited with significant impact as it has ensured that family planning projects and Government services have, for the first time in several years, had a consistent adequate supply of long acting contraceptive methods High unmet need for family planning in Tanzania persists. In Tanzania, despite these recent gains lack of family planning is a problem. It has been found that one in four currently married women of reproductive age want to space or limit births but are not currently using any method of family planningvii. This is called ‘unmet need’ for contraception and implies that there is a high demand for family planning by women in Tanzania that is not being met by current services. Commodity security is a challenge ‘Commodity security’ means that family planning is consistently available to women, that she has a choice of methods, that she can afford the method she chooses and that she receives good quality of care. Without it confidence in any programme will be eroded. While commodity security brings together many complex issues, there are many countries that have made progress toward securing itviii. Achieving commodity security involves funding, procurement, supply chain management, and service delivery. The Government of Tanzania as well as the DPs can work together toward ensuring that each step toward the achievement of commodity security is supported. Contraceptive supplies are a key step in commodity security. Without the essential supplies, the family planning programme cannot function. Whether the GoT or the DPs fund the contraceptives, they must be purchased and in the warehouse for the family planning programme to work. DFID sees the importance of RH supplies and has played an active role in the global Reproductive Health Supplies Coalition at the central level. Support to the RMH supply system will continue this work at country level where it is most important. DFID’s 2010 contribution was positive with real evidence of increasing confidence in programmes and demand from women. Maternal health supplies for safe delivery DFID provides general budget support and other donors fund the health basket. The GoT states that maternal health is a ‘top priority’. Commodity supply is however dealt with as a part of the general health system, without specific attention or prioritisation. However with the increased focus on improving maternal health outcomes, the move to focus specifically on maternal health products, in conjunction with reproductive health supplies, is occurring in other countries as well. There are risks associated with the proliferation of condition specific vertical programmes, but in resource poor countries such as Tanzania, without some specific attention supply chain management will remain inadequate. (Note that RMH supplies in Tanzania are integrated into the essential medicines supplies and are not a vertical programme. Additional attention to seeing they are prioritised would ideally be temporary.) Why do mothers die? The majority of African maternal deaths are from obstetric complications around childbirth including haemorrhage, hypertensive disease (eclampsia), infection, and prolonged labour.ix These complications can be managed within a facility but require trained staff and adequate supplies of simple medications. The quality of maternal health services must improve. About half of Tanzania women give birth in health facilities and 51% of these are assisted by health professionalsx and these proportions have been increasing in recent years. There is a big push internationally and in Tanzania to cut maternal mortality by increasing the numbers of women giving birth in facilities. This will only be effective however if these facilities offer a quality service including essential medications. A recent study found that one of the barriers to increased births in facilities in Tanzania was that the facilities were not perceived to be adequately equipped or supplied.xi Maternal health commodities are not priority within the essential medicines list. While FP commodities are well tracked with good logistics support, maternal health commodities have been dealt with as a part of the general health system. The essential drug budget is under funded. It is only in 2011 that there has been a study by USAID on maternal health drugs. These would include magnesium sulphate (for eclampsia), ferrous sulphate (for maternal anaemia), and uterotomics, such as misoprostol and oxytocin (to ensure the management of the third stage of labour and prevent post partum haemorrhage). The USAID quantification study has shown no GoT attempt to prioritise MH supplies as essential medicines, widespread stock outs and only one month’s supply of drugs in the country (with no provision to purchase more for this financial year). Maternal health commodities are not expensive. These maternal health commodities are relatively cheap and the quantification study determined that all the maternal health commodities required for one year was under £3 million. Quantification of maternal health commodity needs is additionally complicated because many products uses are not confined to maternal health--and maternal health services are part of the general health service. Logistics systems also need to be supported to ensure MH supplies reach facilities. Considerable donor effort (particularly by USAID) has been put toward the tracking of family planning and HIV commodities in the supply chain over the past twenty years. No particular effort has been made to determine whether key maternal health commodities are present in facilities. Supporting maternal health commodity logistics would include attention given to how these commodities are prioritised and tracked within the system and—ultimately, whether they are available at the health facilities. Political support is required for RMH supplies to remain a priority. Despite expressed commitments to maternal health, there is much less willingness to invest in family planning and safe delivery and address the many constraints that prevent women from accessing services. To develop a sustainable high quality system, that is not continually reliant upon external support will require focused policy and advocacy (see Political Appraisal). Beneficiaries. The beneficiaries of the programme will be poor women of Tanzania who have not had reliable access to safe delivery and family planning services in the past. EVIDENCE Who delivers reproductive and maternal health services in Tanzaniaxii Public sector. The majority of RMH services are delivered by the Ministry of Health and Social Welfare. About 96% of women receive some antenatal care and the vast majority of this is at public sector facilities. While half of Tanzanian women chose to give birth at home, 41% of women used public sector facilities to deliver their babies. About two thirds of women using contraceptives received their family planning from the public sector. Private sector. A smaller proportion (7.5%) gave birth in a voluntary/religious hospital and less than two per cent gave birth in private hospitals. Marie Stopes Tanzania is delivering about one-fifth of the contraceptive services in the country. Less than a fifth of women bought their contraceptive through private pharmacies or shops. Some faith-based hospitals were not choosing to provide family planning while others were. Health benefits of family planning. There is a wealth of strong evidence that the health benefits of family planning to women and their children are multiple. Unfortunately, pregnancy and childbirth are risky. In developed countries, 1 in 7,300 women will die in childbirth or from pregnancy related causes. In Tanzania in 2005, the chances of dying in childbirth were 1 in 25xiii. (These risks have fallen slightly in the last five years) And most of these deaths are preventable. Internationally, if every woman had the number of children she wanted when she wanted them, maternal mortality would drop by one thirdxiv. This is because there are safer times to be pregnant (between 18 and 35 rather than earlier or later) and spacing and limiting births reduces risks. Birth-spacing also has benefits to the children. Babies born less than two years after their older sibling are twice as likely to die before they reach their first birthdays as those born more than three years apartxv. When women are unable to practise family planning, they have unintended pregnancies. Unintended pregnancies are more likely to end in abortion. In Tanzania, where abortion is illegal under most circumstances, this is likely to be unsafe and extremely risky for women. Recent estimates suggest that approximately 19% of Tanzania’s maternal mortality is due to unsafe abortionxvi. Family planning can avoid many of these unintended pregnancies in the first place. Method Mix. Women’s preference for spacing births versus limiting their total number of births influences their choices of contraceptive methods. Those wanting to stop childbearing are likely to use one of the most effective methods while those wishing to postpone a birth choose among short-acting reversible methods.xvii It is well documented that a family planning programme must offer the full range of methods to all womenxviii. Long-acting and permanent family planning methods are more effective but are often difficult for clients to access and are not used as widely as other methods, particularly in Africaxix. Reducing maternal mortality Eleven countries account for 65% of all global maternal deaths: India, Nigeria, DRC, Afghanistan, Bangladesh, Indonesia, Pakistan, Ethiopia, Niger, Tanzania, and Angola. The evidence on how to reduce maternal mortality is strong. Causes of death. Haemorrhage accounts for the greatest proportion of maternal deaths (34% in Africa). Hypertensive disorders are responsible for a further 9% of deaths while infections count for a further 10%xx. These are all direct obstetric complications that occur around the time of childbirth and all require the availability of maternal health supplies. Postpartum haemorrhage (PPH) remains the leading direct cause of maternal mortality in Africa and Asia, contributing to approximately 30%xxi or 140,000 deaths per annum. A further 2 million women suffer severe morbidity due to the effects of anaemiaxxii. In efforts to meet MDG 5, addressing PPH has become a significant focus. Clinical effectiveness of maternal health supplies. Technologies, including products, have played a central role in maternal mortality reduction. The international 33 country Magpie Trial showed that magnesium sulphate halved the risk of eclampsia xxiii.xxiv. xxv. In addition, the inclusion of magnesium sulphate in the treatment of eclampsia has substantially reduced fits, morbidity and deaths in Tanzaniaxxvi. A recent study in 33 countries looked at the use of magnesium sulphate for pre-eclampsia and found that magnesium sulphate was effective - the number of women with pre eclampsia needed to treat to prevent a death from eclampsia was 43. It was cost effective, particularly in poor countries , where there was an incremental cost of 456$ (301$-779$) to prevent a case of eclampsia, There has been progress in tackling post partum haemorrhage with active management of the third stage of labour and the administration of misoprostol and oxytocinxxvii. A meta analysis suggested that the effectiveness of prophylactic misoprostol in reducing PPH mortality was 45% and oxytocin was 50%. An economic assessment translated into an incremental cost effectiveness of $34 – 40 per DALY for oxytocin and $53 for misoprostolxxviii. Misoprostol is more expensive than oxytocin and has more side effects; however it is more stable and therefore potentially more suited to poorly resourced settings or those with inadequate cold chainsxxix. WHO has approved misoprostol as a safe alternative in the absence of oxytocin if administered by health workers trained in its correct use. Supplies crucial. Skilled attendants can only perform effectively if they are properly equipped and suppliedxxx. There is consistent evidence that a lack of, or poor quality, drugs, equipment and supplies at RMH facilities has an adverse effect on the utilisation of non-emergency services and on women’s survival chancesxxxi,xxxii. A wide range of common problems with equipment and supplies within RMH health facilities have been documentedxxxiii. Supplies are often missing, incomplete or not readily at hand in RMH facilities. RMH services are highly dependent on the availability of the essential drugs, identified as effective and relatively inexpensive xxxiv and included in the WHO essential drugs listxxxv. A national drug policy is a key component of any strategy to improve the management and use of drugsxxxvi. Despite many essential drugs being cheap and having long shelf lives, many providers lack knowledge about them, clinical guidelines are out of date and drug supply systems are inefficient or ineffective, making access to these drugs either unpredictable and/or entirely absent. Inappropriate handling, storage and distribution can alter the quality of drugs leading to serious health consequences and wasted resourcesxxxvii. The drug situation also affects the way in which health services are regardedxxxviii. Users associate a lack of drugs with poorer quality of carexxxix. Maternal health supplies for safe pregnancy and delivery Pregnancy/Birth Maternal health commodity Condition for which drug is stage required Antenatal Care (ANC) Sulphadoxine Pyrimethamine* Malaria prevention Anaemia FeFol* Normal delivery (all women) Oxytocin Misoprostol Ergometrine Post-partum haemorrhage Episiotomy pain relief Lignocaine* Delivery with complications (emergency cases) Magnesium Sulphate Calcium gluconate Hydralazine*, Methyldopa* Pre-eclampsia and eclampsia Antedote to Magnesium Alternate anti-hypertensives *Multiple uses beyond safe motherhood Procurement as a mechanism to strengthen access to essential drugs, supplies and equipment. Ensuring the right drugs, supplies and equipment are in the right place whenever they are needed depends on a functioning and effective procurement system. As safe motherhood tend to fall within government essential drug budgets, procured and supplied through government channels, they are exposed to the systemic problems of drug supply management described abovexl. With contraceptive commodities often funded and procured by donors, national governments face the challenge of managing multiple funding and procurement routes for maternal, STI, family planning and HIV/AIDS products, which can lead to fragmented procurement with high transaction costsxli. Government capacity needs to be strengthened. A study of Reproductive Health Commodity Security (RHCS) in four countries with poor MNH SRH indicators (Cambodia, Nigeria, Uganda and Zambia)xlii highlights the drawbacks of multiple donor and government procurement where government systems lack adequate oversight capacity. One of the main findings was the inability of the countries to translate national policy objectives into implementation and results. Wider political will was found to be questionable and there was weak ownership, capacity and coordination at all levels. This affected the allocation of funds to RMH commodity procurement and logistics at local and devolved levels, where RMH may not be a priority. Contraceptives were found to be on the countries’ essential drugs lists, but some maternal health drugs and equipment were not. Missing products included magnesium sulphate, oxytocin and MVA kits. All the countries lacked information and strategies for addressing maternal health commodity security, although the importance of supplies was usually stressed in reproductive health policies. In Tanzania, a recent reportxliii found a very similar situation with inadequate oversight capacity of government systems with a need to improve capacity and coordination throughout the system. The just completed DFID-funded Support for Family Planning project found that purchasing contraceptives to fill commodity gaps works in the short run to ensure there are no contraceptive stock-outs at the district level. But the Project Completion Report (PCR) also reported that short-term gap filling did not solve the persistent problem—that government did not address the underlying problems and that future programmes should build in appropriate political advocacy. An audit of the medical supplies department by the controller and auditor general, raised very significant concerns around the robustness of control systems and financial management in MSD, and offered wide ranging recommendations xliv REPORT OF THE ER AND AUDITOR GENERAL ON What are the Reproductive and Maternal Health supply gaps in Tanzania? The following table shows the forecast for Tanzania’s total contraceptive needs from 2012 to 2014. These estimates are based on long experience of estimating Tanzania’s contraceptive needs. Tanzania 2012-2014 Contraceptive Forecast Contraceptive Commodity Microgynon Microval Depo IUD Implanon Jadelle Condoms 2012 amount 4,273,998 1,093,134 3,816,000 55,222 184,828 52,131 11.7m 2013 amount 4,487,698 1,147,791 4,044,960 57,983 199,614 56,301 12.5m 2014 amount 4,712,082 1,205,180 4,287,658 60,882 215,583 60,805 12.9m Determining the RMH supplies gap The following table shows the forecast for Tanzania’s maternal health supplies from 2012 to 2014. These estimates are based on a modelling exercise using estimates of numbers of deliveries and proportions of women suffering from various birth complications. In contrast to the contraceptive estimates, this is the first time these estimates have been collected for maternal health supplies. It is possible that use will be lower than expected, because of clinician and patient behaviour. (This may be particularly true for commodities such as iron which despite clinical benefit are not popular products. Less Fe-fol will be purchased accordingly. ) Maternal health supplies: 2012-2014 Forecasts estimated costs (US$) (based on morbidity/demographic data) TANZANIA - MCH Commodities. £1.00 Equal $1.56 January-12 MATERNAL HEALTH SUPPLIES 2012 FORECASTS ESTIMATED QUANTITY AND COST COMMODITIES unit cost Quantitie s 1 Oxytocin 5IU/ml in 1ml vials 0.18 2,400,870 2 Misoprostol 200mcg tabs 0.15 0.268 3 Ergometrine 0.5mg/ml in 1ml vials Magnesium Sulphate 500mg/ml in 10ml 4 vials 1.3 product cost$ freight$ total cost (prod. + fr.) $ 782,500 432,157 $ 117,375 86,431 $ 23,475 518,588 $ 140,850 70,015 18,764 3,753 22,517 380,325 494,423 98,885 593,307 224,162 $ 53,438 1,344,971 $ 320,627 5 Fe-Fol 200 + 0.25 tabs Sulphadoxine + Pyrimethamine 500+25 6 tabs 0.0033125 338,357,4 15 0.039834 6,707,570 1,120,809 $ 267,189 7 Lignocaine 2% in 50ml vials Calclium Gluconate 100mg/ml in 10ml 8 vials 0.951249 93,090 88,552 17,710 106,262 5,820 4,429 886 5,315 0.761 9 Hydralazine 20mg/ml in 1ml vials 1.42 39,650 TOTAL: 56,303 11,261 67,564 2,600,000 520,000 3,120,000 £2,000,00 0 TOTAL UKP: MATERNAL HEALTH SUPPLIES 2013 FORECASTS QUANTITY AND ESTIMATED COST COMMODITIES unit cost Quantities product cost$ total cost (prod. + fr.) $ freight$ 1 Oxytocin 5IU/ml in 1ml vials 0.18 2,670,000 480,600 96,120 576,720 2 Misoprostol 200mcg tabs Ergometrine 0.5mg/ml in 1ml 3 vials Magnesium Sulphate 4 500mg/ml in 10ml vials 0.15 835,000 125,250 25,050 150,300 0.268 40,000 10,720 2,144 415,000 539,500 107,900 647,400 303,750,000 1,006,172 201,234 1,207,406 6,909,000 275,213 55,043 330,256 101,500 96,552 19,310 115,862 0.76 6,400 4,864 973 5,837 1.42 43,000 61,060 12,212 73,272 2,599,931 519,986 3,119,917 5 Fe-Fol 200 + 0.25 tabs Sulphadoxine + 6 Pyrimethamine 500+25 tabs 1.3 0.0033125 7 Lignocaine 2% in 50ml vials Calclium Gluconate 100mg/ml 8 in 10ml vials Hydralazine 20mg/ml in 1ml 9 vials 0.039834 0.95125 TOTAL: 12,864 TOTAL UKP: £2m MATERNAL HEALTH SUPPLIES 2014 FORECASTS ESTIMATED QUANTITY AND COST COMMODITIES unit cost product cost Quantities freight total cost (prod. + fr.) $ 644,61 3 $ 158,93 7 1 Oxytocin 5IU/ml in 1ml vials 0.18 2,984,322 $ 537,178 $ 107,436 2 Misoprostol 200mcg tabs 0.15 882,985 $ 132,448 $ 26,490 - - 585,642 $ 884,444 117,128 $ 176,889 702,77 0 1,061,3 33 $ 283,461 $ 56,692 340,15 3 $ $ 125,86 3 Ergometrine 0.5mg/ml in 1ml vials Magnesium Sulphate 500mg/ml in 4 10ml vials 5 Fe-Fol 200 + 0.25 tabs 0.268 1.3 0.0033125 Sulphadoxine + Pyrimethamine 500+25 6 tabs 0.039834 7 Lignocaine 2% in 50ml vials 0.951249 450,494 267,002,060 7,116,060 Calclium Gluconate 100mg/ml in 10ml 8 vials 110,266 104,891 20,978 9 0.761 6,892 $ 5,245 $ 1,049 $ 6,293 1.42 46,966 66,692 13,338 80,030 2,600,000 520,000 9 Hydralazine 20mg/ml in 1ml vials TOTAL: TOTAL UKP: 3,120,0 00 £2,000, 000 * The quantities of Fe-Fol were adjusted slightly to meet the anticipated budget. NB: An inflation factor has not been applied to unit costs. The maternal health drugs gap is currently not possible to determine as attempts to track it have only begun in 2011. The above estimates are not based on drugs in the system but on rough estimates of the need for maternal health supplies. What DFID would fund DFID would like to work with GoT, USAID and UNFPA and other donors to determine the RMH supply gaps and to ensure that they are filled for 2012-2014. This is likely to involve purchasing the entire estimated demand for implants and most maternal health commodities. (In these instances the ongoing active management of the supply chain will allow more accurate projections of demand and use to be made.) DFID will therefore support the active logistical management of five maternal health product lines across the country to minimise the risks of stock outs. The cost of this is about $100 000 per product per year. In addition, DFID would like to assist in strengthening the logistics around MH supplies. (The US are already funding this for contraceptive products) Finally, DFID will fund some policy and advocacy around increasing the GOT’s commitment to prioritising and funding these RMH supplies in future. Possible annual funding breakdown Output 1: Contraceptive supplies Output 2: MH supplies Output 3: MH Logistics Output 4: RMH supply policy/advocacy Annual total TOTAL (three years) Amount $US $3.1m $3.1m $0.78m $0.78m $7.8m/yr $23.5m Amount £UK £2m £2m £0.5 £0.5 £5m/yr £15m Why would DFID concentrate on RMH supplies? Other donors with in-depth knowledge and years of experience working on RMH are working to strengthen service delivery and support contraceptive social marketing. These projects are being compromised by the lack of commodities. DFID had no health programme in Tanzania until recently when DFID decided to support the contraceptive commodity supply in 2010. Buying supplies and working with other donors with more dedicated staff time, allows DFID to make a real impact on the health and lives of women in Tanzania whilst minimising transaction costs for DFID and government. DFID filled a key commodity gap in Tanzania’s contraceptive supply in 2010-2011. DFID bought much of the country needs for contraceptive implants and injectables (the most popular method) and these supplies are what are currently filling Tanzania’s medical stores. Without these key commodities, there would have been many unintended pregnancies and health staff would have been unable to answer women’s demand for family planning. Maternal health drugs have been somewhat overlooked in Tanzania and internationally – but they are a key component of preventing death and suffering for women. By investing in this area, we are adding value to the scale up of activity in this area by ourselves and other donors. B. Impact and Outcome that we expect to achieve The impact of this programme is to contribute to achieving MDG5 and reduce maternal deaths, which is in line with DFID’s Business Plan action 5.2 to lead international action to improve maternal health. The current UK Government has committed to 10 million new users of family planning world-wide and save the lives of 50,000 women in pregnancy and childbirth. This business case ties well into DFID’s RMH strategy DFID has two strategic priorities: prevent unintended pregnancies by enabling women and girls to choose whether, when and how many children they have; and ensure pregnancy and child birth are safe for mothers and babies. In the RMH Framework, this BC fits under pillar 3: Commodities (‘getting supplies in the right place at the right time and... making them more available’). The outcome of the programmes is to ensure that family planning and maternal health supplies are available in Tanzania throughout the health system. The expected results for the family planning commodities alone will be the commodities to contribute to 400,000 couple years of protection (CYPs) in total. (NOTE: these commodities are considered to contribute to one third of a full CYP as service delivery costs are not included.) This will avert 139,455 pregnancies, prevent 19,697 unsafe abortions and save 490 maternal lives. The maternal health commodity will provide essential medications for safe deliveries. While MH supply intervention measurements are less well developed, we speculate that 260 women’s lives will be saved per year (to total 1270 maternal lives saved by the project as a whole). Output 1 CONTRACEPTIVE SUPPLIES: would purchase contraceptive commodities to provide contraceptive implants for a half a million women across Tanzania, access to longterm and permanent methods of family planning. Output 2 MH SUPPLIES: will be the purchase of the majority of maternal health drugs for Tanzania, which will result in more safe deliveries. Output 3 MH LOGISTICS SUPPORT: MH logistics support will be included in the intervention package to ensure a steady supply of MH supplies, in good condition, to end users. Output 4 POLITICAL COMMITMENT: will help to build political commitment to sustaining these essential reproductive and maternal health supplies (including DFID working with USAID on high level political advocacy). Not intervening would result in: Irregular supplies of family planning commodities, stagnation and de-motivation in family planning programmes and women being unable to routinely and reliably have the choices to control their fertility. Recent gains in improved CPR would be lost. Childbirth would remain riskier as supplies to ensure safe delivery would not be available within the health system. Maternal mortality would be less likely to be reduced. Appraisal Case A. What are the feasible options that address the need set out in the Strategic case? The Strategic Case sets out a clear need to work in RMH supplies as without reliable and consistent supplies, maternal and reproductive health services cannot be delivered. As DFID Tanzania has decided to work on RMH supplies, there are three options to consider: 1) Do nothing to support RMH services to women across Tanzania beyond budget support and existing projects; 2) DFID funds commodities directly to the Tanzanian Government (through the Medical Stores Department). 3) Fund a package of support toward delivery of reproductive and maternal health commodities in partnership with other development partners. Here are DFID’s critical success factors for the programme: Integrated RH and MH commodity supply at all levels of the health system in Tanzania; Longer term commitment to sustain RMH supply by GoT; Low DFID transaction costs; and Effective logistics and coherent policy around RMH supplies. Option 1: Do nothing to support RMH services to women across Tanzania beyond budget support and existing projects What to do: DFID is already supporting the Government of Tanzania with an annual aid framework of £150m (approx Tsh 300 billion)—one of DFID’s largest programmes in Africa. A significant percentage of the DFID Tanzania programme is provided as General Budget Support (GBS) to assist the Government in implementation of its National Strategy for Growth and the Reduction of Poverty (the MKUKUTA). This assistance is complemented by programmes to increase domestic accountability, tackle corruption, improve public financial management, improve both the quality of basic service delivery and the quality and availability of national statistics on development and poverty. DFID contribution to general budget support already supports the health sector indirectly. How to do it: Continue to put DFID funding directly into budget support and various programmes. Why are we doing it? DFID believes that the GoT will make its own priorities in implementation of its National Strategy for Growth and the Reduction of Poverty (the MKUKUTA) and that in this process, they will grow stronger as a government supporting its population with RMH services. DFID believes the GoT has a good understanding of the balances between curative health and preventative health and will make the right decisions in a transparent manner. Option 2: Funds for RMH supplies directly to the Tanzanian Government (through the MSD) What to do: DFID could fund the Medical Stores Department to procure RMH supplies directly. This ensures the RMH supplies will be purchased at the central level. The MSD would then distribute these RMH supplies as part of its Integrated Logistics System. How to do it: Transfer funds directly to the Medical Stores Department and then monitor that these funds are being used correctly. The Global Fund is using this method and is insisting on transparency in the use of the funds. This is seriously slowing the process down and using considerable Global Fund staff resources but this method is slowly yielding results. Why are we doing it? DFID would do this in order to show trust in the GoT to prioritise RMH supplies and build MSD capacity. Ensuring transparency of this process would require considerable DFID staff input and commitment to monitor. Option 3: Fund a package of support toward delivery of reproductive and maternal health commodities in partnership with other development partners. What to do: Fund RMH commodities through the existing USAID or UNFPA systems including some funding for logistics improvements and policy work. DFID has already once filled a contraceptive commodity gap in Tanzania (in 2010) via USAID systems. This new funding would cover some proportion of Tanzania’s contraceptive commodity needs for 20122014. In addition, DFID would fund maternal health supplies for the same timeframe, including logistics support to better track these commodities (most likely through the USAIDfunded JSI Deliver programme (John Snow Inc)). Finally, DFID would support joint donor advocacy work toward ensuring the GoT prioritises RMH supplies in future, and policy work to ensure effective use. How to do it: DFID sets up an Arrangement on Delegated Co-operation with USAID or UNFPA. USAID or UNFPA monitors the programmes and reports back to DFID. DFID would delegate day to day management to the DP to avoid fragmentation and reduce transaction costs whilst achieving mutually agreed objectives. Why are we doing it? USAID and UNFPA have recently agreed to jointly lead on RMH commodities in Tanzania with government. USAID is a leader on RH commodities and is currently looking into maternal health supplies as well. Their logistics contractor JSI is a respected organisation working on logistics systems in developing countries. DFID and USAID have already worked together on two past family planning projects and the systems have run smoothly resulting in a relationship of high trust. UNFPA has an international mandate to work on these issues. Working through these partners minimises the risks of fragmentation and duplication and reduces transaction costs. Political / Institutional Appraisal The Ministry of Health and Social Welfare (MOHSW) is the ultimate authority on RMH in Tanzania. Along with the Development Partners Group, the MOHSW decides how much of the Basket Funding go to RMH. There is apparently no input into these decisions from other ministries despite the wider development benefits and potential savings that accrue from family planning. The hierarchy in the MOHSW includes the Permanent Secretary and then the Chief Medical Officer, offering overall technical direction. Below him is the Director of Preventative Service, followed by the Reproductive and Child Health Services (RCHS) branch. The head of this unit is developing the RH programme to satisfy the unmet need. However, the RCHS continues to face financial and procurement constraints from a variety of sources. There is no line item in the National Budget, no guarantee that a portion of basket funds is earmarked for the purchase of contraceptives or maternal health supplies, no assurance of funding release once funds are allocated for commodities, little diversification of funding sources and a laboriously slow procurement process once funds are issued. The national Contraceptive Security Committee is addressing these critical policy issues that will require continued advocacy in the months and years to come. In 2010, DFID gave funds to fill a commodity gap but those funds were not intended to build capacity. When the Government is responsible for buying the most popular methods and is not fully committed to the programme, the likelihood of stock-outs and shortfalls increase, making the family planning programme more vulnerable. There is an implicit assumption that when there is shortfall donors will fill the gap. This level of scrutiny has not yet been applied to MH supplies. The Medical Stores Department (MSD) is an autonomous department for the MOHSW and operates on a commercial basis, being responsible for its own financial self sustainability. Currently, all donated commodities destined for the Tanzania public sector are distributed through the MSD central warehouse and zonal warehouses. Under current agreements, the MoHSW is responsible for the distribution costs (approximately 15% of the purchase price) owed MSD for any and all donated commodities. The MOHSW currently owes the MSD Tsh 33 billion for the distribution costs that the MSD has already delivered. The system is clearly not working and requires considerable policy attention. The Auditor General’s report has flagged significant irregularities, and weak systems in MSD. An examination of the MTEF funding trends over the past seven years reveals that the family planning allocation and expenditure was functioning well before 2006. Since that year, however, irregularities have appeared showing a lagging commitment. Conditions for full transformation to a transparent system may not yet be present in the Ministry and the presence of competing factions implies that the managerial and organisational capacity is not yet sufficiently strong for change to take place. USAID has conducted extensive dialogue with the GoT to improve the supply gaps and a written commitment has been provided, however as can be seen from the current MTEF, funding from Govt of Tanzania continues to fall. To attempt to address these concerns, DFID is building on the success of the USAID funded programmes and using DFID’s support on PFM to improve release of Government’s stated budget allocations. There are two issues at play: one is the political will to allocate funding for RMH commodities and the other is the technical ability to forecast needs and track the supplies to see they are where they need to be. MTEF funding trends MTEF Estimated need Year (TZ shillings) 2004/05 7.7 bn 2005/06 6.9 bn Amount Allocated 7.7 bn 6.9 bn Amount Released 7.7 bn 6.9 bn 2006/07 6.9 bn 4.8 bn 8.7 bn* 2007/08 2008/09 2009/10 2010/2011 6.4 bn 9.2 bn 9.6 bn 24.0 bn 4.3 bn 3.2 bn 3.5 bn 3.5 bn 2.2 bn 5.0 bn 7.5 bn 11.3 bn (currently held up in procurement) 2011/2012 6.5 bn 1.2 bn 2012/2013 19.3 bn 1.2bn 2013/2014 14.7 bn 1.2bn *additional basket funding released USAID has been tracking family planning supplies for more than a decade in Tanzania. While the system is not perfect, there is knowledge of what contraceptives are available and where they are needed. The USAID Cooperating Agency John Snow International works with the GOT directly to support this work and forecasting family planning commodities needs works reasonably well. Maternal health drugs, however, have not been routinely monitored to the extent that contraceptives have. Recently, the USAID-funded Deliver project has undertaken a drug quantification exercise which reveals an acute shortage of essential maternal health medicines at all levels of the health service in Tanzania. This is despite the high level claims that addressing maternal health is a high priority for Tanzania. UNFPA is currently working on a study of the supply chain of RMH commodities including logistical and financial flows to the Tanzanian mainland. Their findings imply that the Government does not prioritise family planning because of a poor understanding of how family planning benefits Tanzanians. So when budgetary constraints dictate a need to prioritise, family planning does not rank highly as a lack of family planning drugs does not result in an immediate and severe consequence. Maternal health commodities are perceived as higher priority but it is more likely to be technical shortcomings that result in these supplies being stocked-out. Their study is work in progress and UNFPA is still discussing its findings with the GOT. In addition, UNFPA is planning to undertake an Initiative in Ensuring Access to Priority Life Saving Medicines (for Prevention and Treatment of PPH, Treatment of Pre-eclampsia and Eclampsia and Maternal Sepsis) in selected countries in 2012 including Tanzania. There will be a bottleneck analysis/exercise in 2012. Donor context Many donors contribute to the health basket and budget support and this funding will contribute to the health system required for improving maternal care. General budget support and basket donors are focusing on the health system and drug supply. There is a US, DFID, and Australia alliance at country level around reproductive health which is part of the international agreement approved by DFID’s Secretary of State in 2009. This has been cited as a model of good practice in the review of co-operation one year on. The Germans are working in social insurance for pregnant mothers, social marketing of contraceptives & delivery packs as well as emergency obstetric equipment. The US is major players in family planning and on maternal health quality. USAID contributes funding for well over half of the family planning programme in Tanzania and is widely recognised as the lead funder in the sub-sector. USAID’s well developed RH programme has been functioning for over 30 years. Other donors in the sub-sector are the Germans, the Dutch and the Australians. DFID joined their number in 2010 with its first contribution. UNFPA is also an active partner in MRH commodities, having helped to fill commodity gaps on numerous occasions.xlv USAID and UNFPA have recently agreed to jointly lead on RMH commodities in Tanzania. USAID invests approximately $20m annually in family planning but are relatively new to maternal health where their programme is much smaller ($2m). DFID would work with USAID on high level political advocacy to ensure that the GOT gives adequate attention to RMH supplies. Challenges to the delivery of RMH supplies in Tanzania The process of distribution of any commodity is complicated. Private business has the profit motive to ensure efficient delivery of supplies. The public sector has none of these incentives and has, indeed, many disincentives. Until there is political pressure to ensure effective delivery, the delivery of RMH supplies is a complicated process involving (often) expensive drugs. Not only is the efficient delivery of these commodities a technically challenging process, the possibility of corruption at all levels is also present. It is obvious that it is not easy to maintain a complex delivery system in a country with limited resources and technical ability. The challenges could be the subject of hundreds of technical reports although a recent report to DFID presents the challenges as simply as possible. Based on interviews with Tanzanian informants, the following table identifies challenges to delivering RMH commodities in Tanzania in eight steps. There are multiple technical challenges to running a vast delivery system to myriad facilities, many in remote areas. There are also many political reasons why the system is kept as it is. As the technical and political challenges will be dealt with differently, Table 1 identifies each type of challenge at each step in the process. Table 1. Challenges to the delivery of RMH supplies in Tanzania Commodity Process (steps) Technical challenges Political challenges Step 1: BUDGET. GOT determines health budget. MOH determines allocations based on a formula. Based on these, the Ministry of Finance allocates funds to MSD resulting in ‘credit’ for each health facility (as funds are available) Step 2: PRIORITISATION. MSD prioritises commodities according to GOT MOHSW budget Determining demographic service numbers for health facility calculations MSD receives only 30-50% of what it has requested; Irregularities in budget size; GoT owes MSD billions for the distribution of donated commodities; Release of funds held for the end of FY so poor allocation timing; MSD cannot reveal funding shortfalls without MOH PS approval Lack of clarity or understanding of commodity prioritisation process; RMH commodities not on essential lists; donations in kind Ensuring that GOT allocates adequate funding for essential health commodities and that this money actually goes to MSD; annual funding fluctuations; funding arrives late; Assumption that DPs will come in and fill any gaps. (And donors are fickle.) Ambivalence to family planning for religious or ideological reasons in influential individuals Broader development benefits not considered . important; Stock-outs on RMH commodities; MoHSW procurement gets involved in some commodities Step 3: CENTRAL TO DISTRICT. MSD processes orders for facilities from nine zonal stores. (MSD only responsible to deliver to district level.) Inadequate stocks to cover the country because of inadequate funding MSD can’t reveal true stockouts (see above); USAID and the Global Fund are the only donors strengthening this process Step 4: ZONAL WAREHOUSES. MSD Zonal Warehouses receive commodities for health facilities, processes Integrated Logistics System (ILS) Report & Request (R&R) forms, and drop off supplies at District medical office. Varying district capacity; a mixture of integrated (ILS) and vertical programmes (as well as free v pay-for-service) complicates process Government has publicly stated policy on universal access and commitment to free care for certain diseases. Step 5: DELIVERY TO FACILITIES. Health facilities must pick-up medicines and supplies from the District stores; In some cases District stores deliver commodities as they are able. Ordering with the R&R form is not easy; Disbursal not always happening; Lack of transport or fuel; difficult roads; inadequate storage President’s office is pushing MSD to deliver to the health facility; Many health facilities exist in name (and credit )only Step 6: FACILITY LEVEL. Health facilities receive partial delivery of what they need. (This can be from lack of funds in their account or a lack of product availability from MSD.) Stock-outs of critical RMH commodities (these are greater in more remote areas); Reactive health staff make do with what they have, even if from another vertical programme The process that allows facilities to buy commodities when MSD is stocked out is cumbersome. Lack of MSD transparency on stock-outs means that districts cannot spend money to fill commodity gaps Step 7: RE-ORDERING. Health facilities prepare quarterly requests for further commodities with R&R form. A ‘pull’ system means that health facilities a) need to understand what they are ordering; b) must make tradeoffs and do not always make the best choices; and c) don’t know what is not in stock and often expect medicines when they not available. Many DMOs do not understand or don’t care about the Report & Request (R&R) form and simply copy out last month’s form. R&R form is paperbased. Step 8: REPEAT. MSD Central receives requests from health facilities and prepares to begin the quarterly process again. Commodity consumption is never measured; RCH Coordinators could strengthen their role here. Source: Bradford, C (2011). Tanzania Reproductive and Maternal Health Commodities. Trip Report. Environmental and climate change effects The family planning component of the proposed project is likely to have a potentially substantial positive environmental impact and a limited direct detrimental environmental impact. See Annex 1 & 2 for the full climate change assurance note. The maternal drugs component is unlikely to have any significant impact on environmental or climate change issues. Positive environment impact. There is a significant benefit associated with higher uptake of family planning services and smaller family sizes which relates to climate change and pressure on natural resources. Increased contraceptive use should result in a lower fertility rate, which in turn results in slowed population growth. Tanzania’s current 45 million people are currently projected to grow to 67 million by 2025.xlvi Population growth is a major contributor to environmental degradation. As populations grow, settlements expand and encroach on natural habitats, often leading to habitat loss. They also put pressure on natural resources, such as water and ecosystem services. As an example, by 2015, population growth will mean that Tanzania’s per capita water resources could fall below 1,700 m3 per person: the definition of water scarcity. Population growth will also lead to environmental degradation through the demand for additional goods and services, which are particularly important due to the strong urbanisation trends in Tanzania. Potential increasing demand for energy and transport will also have an impact on increased use of fossil fuels, potentially doubling greenhouse gas emissions over the next twenty years, as well as increasing urban air pollution and congestion. Fewer people generate less green house gases which are the main determinant of adverse climate changes. Population growth and increasing urbanisation are key factors as well as climate change in determining future economic costs. These rapid demographic changes will be important in future impacts, adaptation and emissionsxlvii. In fact in a recent paper produced by climate change experts at the Centre for Global Development, family planning was identified as the best buy for a single intervention to reduce green house gasesxlviii. If family planning is combined with girls’ education there are even more significant gains, as the table below shows in terms of the number of tonnes of CO2 saved for $1 million invested. It has been argued that the combination of family planning and girls’ education would be a better investment than the UN Reducing Emissions from Deforestation and Forest Degradation (REDD), which aims to spend $30 billion a year on incentives for developing countries to reduce deforestation and forest degradation.”xlix Table 5: Saving CO2 emissions by development intervention Intervention Family planning combined Tonnes of CO2 saved & girls' education 250,000 Family planning alone 222,222 Girls education alone 100,000 Reduce slash and burn of forests 66,667 Pasture management 50,000 Geothermal energy 50,000 Energy efficient buildings 50,000 Pastureland afforestation 40,000 Nuclear energy 40,000 Reforestation of degraded forests 40,000 Plug-in hybrid cars 33,333 Solar 33,333 Power plant biomass co-firing 28,571 Carbon Capture and Storage (new) 28,571 Carbon Capture and Storage (retrofit) 26,316 It should be noted that, while increased contraceptive use will reduce population growth, caution should be practised in using this argument without stressing the importance of voluntary family planning to allow women to meet their reproductive desires. The health benefits to women alone (e.g. the reduction in maternal mortality) are adequate argument to the provision of good family planning services. Better logistics and drug management should decrease the numbers of drugs and commodities that are damaged or expire, and hence decrease the environmental impacts of disposing of waste products. Potential detrimental environmental impact. There are two possible detrimental effects that this programme might have on the environment: The release of carbon dioxide through transport of drugs and commodities Waste generated as a result of used contraceptive commodities. The programme will attempt to minimise any negative impacts on the environment. Drug and commodity supplies will be routine and there should be no specific additional deliveries for this project Waste disposal should follow carefully-designed protocols. It is on this basis that the programme’s likely impact on climate change and the environment has been categorised as “B”: medium/manageable potential risk, with good opportunity for improvement. Table 6: Evidence rating and climate change and environment category Option Evidence rating Climate change and environment category (A,B,C, D) 1 Do nothing Medium C 2 Go through Medical stores Strong B 3 Work with US Strong B THEORY OF CHANGE IMPACT: RH commodity supply £15 m over three years MH commodity supply High quality RMH services MH commodity logistics support Policy support Family planning need satisfied Women supported in pregnancy & childbirth Convinced policy-makers that RMH is important Advocacy for strong RMH health services •Fewer births • Births are well spaced •Fewer unplanned pregnancies and unsafe abortions •Safe births with fewer complication WIDER IMPACT •Healthy mothers •Healthy children •Less pressure on social services •Improved welfare •Political commitment to maintain system B. Assessing the strength of the evidence base for each feasible option In the table below the quality of evidence for each option is rated as either Strong, Medium or Limited Option 1 2 3 Evidence rating Strong Strong Strong C. What are the costs and benefits of each feasible option? While measuring family planning results has a clear and proven methodology, maternal health supplies have never been tracked carefully and there is no clear methodology yet developed to measure the results obtainable by the presence of MH supplies. (In April 2011, a nascent Maternal Health Supplies working coalition has begun and in October 2011, a proposal for the creation of a Commission on commodities for women’s and children’ health has been put forward as part of the ‘Every Woman, Every child’ global effort. Doubtless, better measures of maternal health supplies will soon follow.) Meanwhile, this work puts DFID Tanzania in the vanguard for seeing the importance of these supplies and attempting to ensure their availability. The cost-benefit analysis below has used a modelling framework based upon the MSI impact calculator which is used by most DFID projects, and forms the basis of the DFID RH results framework. The other assumptions (around the proportionate costs and benefits attributable to commodity supply alone) are based upon guidance from policy division. The CYP is calculated by multiplying the quantity of each method distributed to clients by a conversion factor, to yield an estimate of the duration of contraceptive protection provided per unit of that method. The CYP for each method is then summed for all methods to obtain a total CYP figure. CYP conversion factors are based on how a method is used, failure rates, wastage, and how many units of the method are typically needed to provide one year of contraceptive protection for a couple. The calculation takes into account that some methods, like condoms and oral contraceptives, for example, may be used incorrectly and then discarded, or that IUDs and implants may be removed before their life span is realized. Once again, here are DFID’s critical success factors for the programme: Integrated RH and MH commodity supply at all levels of the health system in Tanzania; Longer term commitment to sustain RMH supply by GoT; Low DFID transaction costs; and Coherent logistic and policy around RMH supplies. Examining the options Options Costs Benefits (Quantitative & Qualitative) (Quantitative & Qualitative) Option 1: No commitment cost Do nothing to to DFID support MRH services to women across Tanzania beyond budget support and existing projects Option 2: Funds for commodities directly to the Tanzanian Government £15m over three years (extendable to five years) DFID staffing: 1.5 FTE (based on Risks & Assumptions Risks Benefits: GoT’s resource allocation to FP and maternal health supplies, which may improve if donor funding is not available, results in a reduction in maternal mortality. Positive benefits: RMH supplies where they are needed would result in a quicker reduction of maternal mortality and a quicker increase in contraceptive prevalence versus option 1, delivering the following quantified results: RMH supplies remain a low priority Logistic systems remain weak Risk Fiduciary risk that funds will not be used for their intended purpose (through the MSD) GFATM experience) totalling approximately £671,000 over three years Main cost drivers will be commodity costs there is international pressure to reduce these – and potential economies of scale. Costs will be explicitly tracked in the log frame - 0.6 million CYPs from the commodities alone resulting in 208,142 pregnancies averted, 29,399 unsafe abortions, 729 maternal lives saved plus (at least) 780 women saved from haemorrhage Non-quantified results: Other lives saved/ disability reduced through MH interventions Improved perceptions of quality of RMNH services and possible increased utilisation Negative benefits: Fiduciary risk that funds will not be used for their intended purpose decreases results. Channelling through MSD results in considerably slower system in the short-term – several years (as evidenced by Global Fund experience) leading to lower results. Option 3: Fund a package of support toward delivery of reproductive and maternal health commodities in partnership with development partners Current situation with MSD is perpetuated Inadequate engagement and support from GoT Risks, if materialised with result in stockouts continuing particularly in the short-term Results would not be realised if distribution and storage problems results in high levels of waste Assumptions: Funding the commodity only results in system changes, including for logistics. Risks £15m over three years (extendable to five years) DFID staffing: 0.1 FTE totalling approximately £45,000 over three years. $30 000 per year for USAID costs UNFPA unquantified at present Positive benefits: RMH supplies where they are needed would result in a quicker reduction of maternal mortality and a quicker increase in contraceptive prevalence versus option 1, delivering the following quantified results; - 0.4 million CYPs from the commodities alone which will result in 139,455 pregnancies averted, 19,697 unsafe abortions, 488 maternal lives saved plus 780 women saved from haemorrhage (result from the maternal health supplies). Non-quantified results: Other lives saved/ disability reduced through MH interventions US Government political change makes funding of family planning impossible Change of provider by USAID during course of support Inadequate engagement and support from GoT USAID staff over-stretched. Improved perceptions of quality of RMNH services and possible increased utilisation (Lack of data/evidence prevents their quantification) Longer-term impact of logistic and policy support on RMH supplies, thereby supporting sustainability. Fragmentation and lack of government coordination of RMH Assumptions GoT is content that funds are not being channelled directly. Continued good experience of working with USAID CSC Option 1 Option 2 Option 3 Integrated RH and MH Commodity supply at all levels of the health system (Max10) Longer-term commitment to sustain RMH supply by GoT Max 5 Low DFID transaction costs Max4 Coherent logistics and policy support around RMH supplies Max 6 TOTAL 2 7 9 3 1 3 4 1 3 1 2 5 10 11 20 Comparison of Options Under option 1, maternal mortality is likely to decline albeit at a slower rate than options 2 and 3. However, any possible reductions could be undermined by the risk that RMH supplies remain a low priority and that the logistics system would remain weak. According to the modelling calculations, option 2 could result in potentially 33% more quantifiable results than option 3 if the funding was completely spent on RMH commodities. It is also the option that DFID would most like to be able to choose as the ideal would be a robust and reliable system of logistics for all essential drugs through MSD lead by Government. But this comprehensive solution has no guarantee of success, noting the risks and assumptions mentioned above. Working through the MSD would require considerable DFID staff time to ensure transparency of spend and to assess fiduciary risk. The experience of the Global Fund shows that this approach may be fruitful in the long run but extremely time consuming for staff. It could also result in severe stock-outs in the short run, thereby undermining results in the short-term. The work of the Global Fund may be setting the stage for DFID to choose Option 2 in future years, particularly if stronger political support for family planning were to be built. But our analytical conclusion is that selecting option 2 now is likely to be premature. Option 3 results in fewer results compared to option 2 as more funds are devoted to policy and logistics capacity building for GOT. However, the experience of the last commodity project has demonstrated that simple commodity procurement is not enough to ensure that GOT will prioritise RMH supplies and ensure they are present in the health system. Ensuring engagement with the GoT and their long term support to maintaining RMH supplies needs active dedicated support to quantification and logistics. In addition, working through another DP will use less DFID staff resources, noting that low transaction costs were identified as a critical success factors. Our analytical conclusion is therefore that option 3 is preferred as it delivers a good package of more guaranteed results whilst in parallel supporting the development of a longer-term sustainable system of RMH supplies. Funding for this option would be channelled through DPs to carry out the package of interventions. Detailed Description of the Selected Option Output 1 Contraceptive commodities are available, particularly long-acting and permanent methods: would purchase contraceptive commodities to provide a half a million women across Tanzania access to a long-term method of family planning. DFID works with USAID to determine that the contraceptive gap is filled for Tanzania. UNFPA may also be involved in this discussion. USAID contractors procure the commodities and they arrive in the government medical stores. This process is straightforward and DFID has already purchased commodities via USAID for Tanzania in 2010. Output 2 Replenishment of essential obstetric drugs throughout Tanzania: will be the purchase of essential MH supplies which will result in more safe deliveries. There will be certain flexibility, as needs assessments are continually evolving, and other donors are funding specific product lines. It is likely that DFID will fully fund the countries requirements for oxytocin ergometrine, magnesium sulphate, llignocaine calcium glocomnate and hydralazine. This work is less well defined as maternal health commodities have been less studied than family planning commodities. The maternal health commodities list is still under discussion and there are many challenges to determining the baselines. USAID is beginning to consider which tracer drugs should be used to track maternal health supplies throughout the system but there is considerable work still to be defined. Output 3 Logistics systems strengthened for maternal health drugs: As the logistics systems for MH commodities are underdeveloped and the MH supply situation in Tanzania is not yet clear, MH logistics support will be included in the intervention package to ensure a steady supply of MH supplies. As with output 2, what this support will consist of is not yet defined. Strengthening MH logistics is likely to look very similar to the support for family planning commodities but there are additional complications such as the necessary cold chain for oxytocin and the fact that maternal health commodities can be used for other indications. DFID plans to invest in improving logistics for five products (at $100,000 per product as part of the contract). In working with the lead agency in partnership, there will be flexibility, especially to fill gaps of other donors, if necessary. Output 4 Political commitment and appropriate policies sustain maternal and reproductive health commodity supply and use will help to build political commitment to sustaining these essential RMH supplies. This sort of focused intervention on core public health priorities should not be necessary – they should be fully funded as priority health interventions The reasons that they are not are complex – associated with lack of female empowerment and religious issues as well as weak management capacity and general lack of prioritisation. The political interest and advocacy around reproductive and maternal health is increasing at international levels. At this stage, and in advance of more analysis of the politics and drivers of change around the issue it is not possible to be prescriptive as to exactly what this project will do, and how it will fit with other initiatives. It will combine support for high level political advocacy with more technical and localised work on accountability. Potential advocacy entry points might include: Budget monitoring for RMH supplies; Looking at how RMH supplies are prioritised and engage in discussion; Locate national champions that policy-maker will heed; Raising awareness of the problem at community level; Using presence of RMH supplies as an indicator of a successful RMH programme; Mobilising support for the DFID ‘golden moment around family planning’ Linking up with the Commission for information and accountability and reproductive for women and children’s health – and supporting country level activities in Tanzania Linking with the regional project evidence for action, to ensure family planning issues are adequately reflected in country plans D. What measures can be used to assess Value for Money for the intervention? To assess value for money, the two different types of commodities will be discussed in turn: a) family planning commodities (where there are well developed tools to measure) and b) maternal health supplies (where there has been little research done as yet to determine good measures). FAMILY PLANNING SUPPLIES Family planning is good value for money. At a global level, the Guttmacher Institute has undertaken research which demonstrates that increasing the coverage of modern family planning methods is a highly cost effective interventionl. They calculate that meeting the need for family planning methods for 818 million women in developing countries would cost: $ 28 to avert an unintended pregnancy $ 3050 to save the life of a woman or newborn $ 62 to save a DALY (women and newborns combined) Putting this in the context of other common health care interventions in developing countries they demonstrate that such a cost-benefit figure represents relatively good value for money: Table 7: DALY costs by intervention Intervention Insecticide-treated bed nets Malaria prevention for pregnant women Tuberculosis treatment (epidemic situations) Modern contraceptive methods Antiretroviral therapy (Africa) BCG vaccination of children Oral rehydration therapy Cholera immunisation Cost per DALY saved in US$ 13-20 29 6-60 62 252-547 48-203 1268 3516 Furthermore the Guttmacher Institute in 2009 demonstrated that in Sub-Saharan Africa, providing modern contraceptives to all women who need them would more than pay for itself, saving $1.30 in the cost of maternal and newborn care for each dollar invested. The expected results for the family planning commodities alone will be the commodities to contribute to 0.4 million couple years of protection (CYPs) in total. (NOTE: these commodities are considered to contribute to one third of a full CYP as service delivery costs are not included.) This will avert 139,455 pregnancies, prevent 19,697 unsafe abortions and save 488 maternal lives. The maternal health commodity interventions measurements are less well developed. When the measurements for maternal health commodities are determined, the results for this programme will increase further. Long acting methods, such as implants, have higher unit costs than methods such as sterilisation or iUCD insertion that require more sophisticated clinical delivery systemsli. The importance of a broad family planning method mix that offers women a non-coercive choice of family planning methods has already been acknowledged, Long-acting and permanent methods LAPM are more effective and, as a result, save more lives, and implants and injections are particularly important where clinical capacity is limited, . Short-term methods rely on the users to remember to take their pills or go to the health facility for their injections. This higher degree of user dependence lowers a contraceptive’s effectiveness. Many countries in sub-Saharan exhibit a high proportion of women contracepting (contraceptive prevalence rate) but this high CPR does not translate into lower fertility rates. This implies that use of family planning is less effective—in the case of Tanzania, this is partly due to a high proportion of women using injectable contraceptives. A modelling study lii has shown that if one-fifth of African women contraceptors switched to LAPM, more than 10,000 maternal deaths would be averted. This health benefit to women is a compelling argument on its own but there are additional benefits to the woman such as less time spent resupplying her short-term family planning. Poor patterns of short-term hormonal contraceptive use (high discontinuation rates and incorrect use) contribute significantly to the problem of unintended pregnancy in sub-Saharan Africa. Increased availability and use of more effective methods, such as implants, will improve reproductive health in sub-Saharan Africaliii. As women may be using injectable contraceptives because they can use them surreptitiously, there should be continued work in Tanzania to increase the acceptability and acceptance of family planning to husbands. Table 8: Costs of contraceptive methods Contraceptive method Male condom Pill IUD Female condom Injectable Vasectomy Sino-implant* Female sterilization Implant (Jadelle) Implant (Implanon) Unit cost ($US) 0.025 0.21 0.37 0.77 0.87 4.95 8.00 9,09 24.09 24.09 Cost per CYP ($US) Na 7.80 1.75 Na 7.90 2.25 4.00 4.00 8.15 12.25 Source: Wickstrom and Jacobstein (2011)liv *Not yet internationally quality assured. Results from contraceptive supplies only (Total spent: £6m). At the moment there is some flexibility around proportions of contraptives and MH product purchased, to ensure complimentality with other donors, and that all needs are met. We have therefore modelled the use of more expensive methods and a significant spend on advocacy and policy work that does not yield directly quantifiable results in terms of lives saved. The cost per CYP will be £15.23. This cost per CYP is more expensive than a full FP programme with a rounded method mix. Implants are expensive medical devices but, in return, yield one of the best longacting contraceptive methods—important for increasing the effectiveness of Tanzanian women’s contraceptive use.(See strategic case for more information on the importance of the method mix and long-acting contraception.) This therefore is a ‘worst case scenario’ and cost effectiveness may increase if spend is higher on commodities, and if cheaper products are procured. Reproductive Health Supplies Coalition (RHSC) increasing VFM DFID is currently chairing the RHSC, a group of organisations working together to reduce contraceptive prices and increase their efficient delivery. In 2011, the RHSC had a major victory when the drug companies reduced the unit price of their implants (see table). This work is directly increasing the VFM for this Business Case as DFID is able to purchase implants at the new price. Increased volume in the future may allow DFID to purchase implants at an even lower price. This reduction in contraceptive commodity price can be directly attributed to the cross-DP advocacy work carried out by the RHSC. Table.9 RHSC is responsible for price reduction in implants Type of implant Old price New price (2011) Jadelle Implenon $21.18 $19.60 $19.50 $18.00 Possible lowest price $16.50 $16.50 MATERNAL HEALTH SUPPLIES What is known about determining results from ensuring the presence of MH supplies? There has been little work and research to date on MH supplies as a whole although several groups are looking at specific drugs We know that the marginal cost of having ocytocin and misoprostol in facilities is low, and use of oxytocin or misoprostol has a cost effectiveness of $35-50 which is compatible with other ‘best buys in health’ An economic assessment of interventions to reduce postpartum haemorrhage in developing countries found these new interventions are cost-effective and cost-beneficial technologies with great potential to reduce PPH and its consequenceslv. The Magipie study in 33 countries looked at the use of magnesium sulphate for pre-eclampsia and found that magnesium sulphate was cost effective and costs less and prevents more eclampsia in poorer countries than in richer ones. With little research on which to base the results that may be obtained from the presence of MH supplies in facilities, the next paragraph attempts a crude estimate. Results from maternal health supplies. Offering emergency obstetric care involves a functioning health system which includes health personnel, facilities and medical supplies. The African Science Academy has estimated that offering emergency obstetric care to all women who needed it in Tanzania would save 3500 maternal lives per year lvi. Approximately 30% of these women (1050) died from haemorrhage. It is safe to say that the absence of maternal health supplies would be responsible for a proportion of these deaths. The Abt study on preventing post partum haemorrhage PPH suggested on the basis of metanalysis that prophylactic uterotonics have a 50% risk reduction. These are based on clinical studies – and under routine conditions low efficiency e.g. suboptimal distribution and administration etc, may, pessimistically decrease overall impact by 50% This would result in 260 lives being saved 260 £576,919.00 £149,692.00 £200,000.00 £200,000.00 £1,126,611.00 Number of women saved from haemorrhage by health supplies All oxytocin purchased for one year All misoprostol purchased for one year Logistics support (two commodities) for one year advocacy (proportion 40%) for one year DFID spend (total) £4,333 Cost per maternal live saved This is a very conservative estimate, as in addition to lives saved from haemorrhage, lives will be saved from eclampsia and other causes, and there will be a very significant number of DALYS saved through reduced anaemia and pre eclamsia. This would imply that supporting MH supplies offers as good or better value as family planning (at £12,283). (Recall that this estimate for FP is high as it assumes that DFID is buying the most expensive contraceptive in a range of methods.) Investing in logistics for MH supplies. Logistics support good value as it improves the efficiency of the system over the longterm, in particular because it decreases wastage. Supporting systems that determine the bottlenecks currently operating in the delivery of MH supplies will sort problems in the longterm. Improving the medical supply system will support the entire health system. Supporting political advocacy. Ensuring that RMH supplies are present in the health system is not simply a technical problem. Unless RMH services and supplies are understood, acknowledged, and acted upon, maternal mortality will remain high in Tanzania. DFID will invest £1.5m over three years to shore up political support and understanding for RMH. E. Summary Value for Money Statement for the preferred option Investing in Reproductive and Maternal Health commodities is going to be very good value for money for DFID as the investment in RMH health is well documented and ensuring the presence of RMH supplies where they are needed will save both maternal and child/infant lives. Table 10 VFM metrics to monitored Intervention Economy FAMILY PLANNING Programme cost for a CYP is £15. Price of implants is reduced Price of all commodities MATERNAL tracked in HEALTH logframe significant Programme cost economies of of maternal life scale saved: £4,333 anticipated Commodity costs – relative to international benchmarks Logistics support cost per product line monitored Efficiency Effectiveness Avoiding stockouts and logistic support increases the overall efficiency of RMH services Increase in CYPs delivered by the programme (Target: 0.4m CYPs) Long acting methods are more effective particularly for rural women Cost effectiveness of maternal health drugs is v high, particularly given ‘sunk costs ‘ in MH services by govt and other donors Build on evidence base LAPM are more expensive but increase family planning effectiveness. MH supplies are poorly studied and there are no models that determine results from seeing that the health system is supplied. DFID can begin to ask the relevant questions. Commercial Case Direct procurement A. Clearly state the procurement/commercial requirements for intervention There is no direct procurement in this programme by DFID. B. How does the intervention design use competition to drive commercial advantage for DFID? NA C. How do we expect the market place will respond to this opportunity? NA D. What are the key cost elements that affect overall price? How is value added and how will we measure and improve this? NA E. What is the intended Procurement Process to support contract award? NA F. How will contract & supplier performance be managed through the life of the intervention? NA Indirect procurement A. Why is the proposed funding mechanism/form of arrangement the right one for this intervention, with this development partner? DFID will be contracting USAID to deliver RMH supplies and logistical support. DFID will be contributing to pooled funding with other donors for joint policy work. The activities of this RMH supplies programme will be procured indirectly, through USAID. This programme is for both programming and commodities and will use USAID procurement policy and guidelines. . Up to 0.4% (i.e. £60,000) of the programme cost will be used by USAID to cover the cost of staff for the additional work. DFID Tanzania has not been active in the health sector until 2010 when it began supporting the sector where there are gaps in provision that could not be filled by other partners. In 2010, DFID Tanzania decided to respond to a contraceptive shortage with support to the Tanzanian family planning programme. However, as there was no dedicated DFID health adviser or administrative support to supervise such a programme, it was decided to provide the required resources through USAID—the donor in Tanzania who has the most experience in family planning, using a Memorandum of Understanding (MOU). It is intended that this collaboration is continued for the RHM supplies with a new agreement to be called an Arrangement on Delegated Co-operation (ADC) between the Government of the United States of America and the Government of the United Kingdom of Great Britain and Northern Ireland regarding Support for RMH supplies in Tanzania. (See Annex1.) This programme involves intense involvement in supply procurement; expertise that DFID does not possess so would be unable to deliver the interventions directly. By partnering with USAID, DFID Tanzania is able to deliver improved results in CYPS and reduced maternal deaths. USAID Tanzania has the history, staff, engagement with the MoHSW and robust management, monitoring and supervision systems to deliver the expected results. USAID Tanzania has a formal project management protocol that assures the necessary support and oversight. The activities proposed here fit into USAID’s larger programme. The indirect procurement component of the programme will be managed under an ADC with USAID, who will enter into a contractual agreement with the Implementing Agency and other development partners and is appropriate for the following reasons: It provides effective means of reducing the management burden to DFID that would be imposed through the use of commercial contracts; It enables existing activities by USAID to be harnessed and expanded through the provision of additional resources to these organisations; and The use of USAID to manage this programme including financial management, procurement management, M&E and reporting provides better value for money under the current DFID environment of doing more development work with less resources. It minimises fiduciary risk by using existing USAID procedures to manage DFID’s funds. These instruments will deliver value of money through the assets that USAID will bring to the programme. These include technical expertise in family planning, contraceptive commodities procurement, distribution, utilisation and safe disposal and ability to expand quickly. USAID provides the monitoring of the programming and robust procurement procedures. In addition, with an ACD with USAID there are very strong and transparent organisational and financial management processes. If, during the course of implementation, it would be considered beneficial (and better VFM) to adjust these funding arrangements, it is agreed that funding could be adjusted, by mutual agreement between DFID and USAID. The potential financial risks of using these instruments (as opposed to commercial contracts) will be mitigated through the use of semi annual tranche releases to USAID, including quarterly progress and financial reports that are reviewed by programme staff, to ensure that the services provided are appropriate and of high quality. The programme will procure goods and services from this partnership using USAID’s procurement mechanisms and delivery channels. DFID have reviewed the procurement strategy of USAID and find that it is robust and rigorous and focused on achieving the best VFM. USAID will also conduct cross-checking on the prices of goods and services against those of similar inputs in Tanzania and the region, when goods are being purchased as part of their procurement procedures. Cost consideration is also part of an award negotiation and will be a key activity in selecting the next tender. Value for money is a key element in this process. An alternative approach would be to work through UNFPA, as is done in other countries UNFPA do have procurement capacity, and a mandate to work on these issues. In Tanzania they procure through the health basket and MSD and are not seen as the lead agency on commodity security. There current spending is relatively low, and so rapid scale up would be a challenge. DFID would be keen to see them working more in this role, and it is hoped that the joint donor working group might facilitate this B. Value for money through procurement USAID purchases contraceptives worldwide and their bulk purchases greatly drive down the unit price of family planning supplies. MH supplies have not been purchased by USAID in the past but they have robust competitive processes. USAID procurement is not tied to US products. Where it is going to be cheaper and/ or faster, the in country team will work with MSD to procure supplies locally. At a global level, USAID is known for having robust mechanisms in place to ensure good value for money and quality. DFID Tanzania’s experience of working with USAID at country level has been good. DFID Tanzania has already three times worked with USAID through an MOU to provide health services to Tanzania: to support the hang-up malaria bednet campaign for children under five in 2009 (£800,000), to fill the gap in the supply chain for the purchase of contraceptive commodities in 2010 (£6.5 million), and to deliver family planning outreach services via Marie Stopes Tanzania (£8 million). All of these programmes have performed well and highlight the strong effectiveness of USAID’s management capacity. Control of administrative costs: The Implementing Agency will develop an annual workplan and objectives for key performance indicators that will be approved by USAID and reviewed by DFID Tanzania. On a quarterly basis, they will provide a summary overview of key activities and outputs to USAID and DFID. This report will also include financial data and updates on key indicators. USAID Tanzania staff meets regularly with implementing agencies and the annual planning and quarterly reporting are a formal part of the project management process, as detailed in the Agency’s formal policy directives and guidelines. VFM in purchase of programme goods: The Implementing Agency’s procurement policy and guidelines set out organizational procedures for procuring goods, and services globally. All procurement will be required to fulfil USAID’s standards and procedures. Partnership with USAID. The partnership with USAID/ Tanzania will also serve to mitigate further any fiduciary risk. USAID’s regulation and policy guidelines are rigorous. Prior to making the central award, The Implementing Agency is fully required to satisfy the Agency that they have the capacity to adequately perform in accordance with the principles established by USAID and the US Office of Management and Budget (OMB). A positive responsibility determination means that they possess or have the ability to obtain the necessary management competence to plan and carry out the assistance programme to be funded, and that the applicant will practice mutually agreed upon methods of accountability for funds and other assets provided by USAID. Financial Case A. What are the costs, how are they profiled and how will you ensure accurate forecasting? The expected cost of the programme is £15million over three years. The approximate allocation of funds to components of the programme will be as follows: Payment Schedule Annual funding breakdown FY 11/12 FY 12/13 Total FY 13/14 FY14/15 (£) Feb-12 Aug-12 Mar-13 Sep-13 Mar-14 Mar-15 Output 1: Contraceptive supplies 2m 0 2m 0 2m 6m Output 2: MH Supplies 2.5m 0 2m 0 2m 6.5m Output 3: MH Logistics 0.25m 0.25m 0.25m 0.25m 0.25m 1.25m Output 4: RMH supply policy/advocacy 0.25m 0.23m 0.23m 0.25m 0.23m 1.19m 0.02m 0.02m 0.06m 4.48m 0.02m 15m USAID - Management fees Annual Total 0.02m 5m 0.5m 4.5m 0.5m NB: There will be some flexibility in the funding between outputs depending on other donors contributions and emerging needs. B. How will it be funded: capital/programme/admin? All required resources will be programme funds—which will cover procurement of goods and services. This is part of the budget allocated within the Operational Plan for DFID Tanzania covering F/Ys from 2011/12 up to 2014/15. There are no contingents or actual liabilities. C. How will funds be paid out? Funds will be paid by DFID to USAID on a six-monthly basis in February 2012 and every six months thereafter, on receipt of a formal request which includes a financial statement of need for the forthcoming six month period. This will minimise risks that funds are disbursed in advance of need at any time. Payments for procurement of goods will be made in compliance with USAID Procurement Policy. Funds will be disbursed according to the terms of the ACD between DFID and USAID, which have a semi-annual disbursement schedule. USAID will then fund the Implementing Agency and supervise the programme and provide report back to DFID every quarter. Reports will be available 30 days after the end of each quarter. USAID and DFID are currently using this mechanism for other activities to mutual satisfaction. If there are policy changes for USAID that make their administration of this family planning contract untenable, and therefore could not guarantee that the funds would be released in a timely manner to ensure delivery of the programme, DFID will engage UNFPA and directly contracting JSI through accountable grant arrangement during the course of the three year period (extendable to five years). This transition could be managed smoothly with minimal impact on project implementation though with some transaction costs to DFID. While this is unlikely, as it would take a Presidential change, as well as a congressional change (i.e. with a Democrat for President, they could continue support for family planning, even with a republican majority in the Congress). The fact remains that family planning is a contentious issue in American politics and a different presidential administration could have implications for USAID and its administration of family planning projects. If the programme is terminated early, through no fault of the implementing partners, USAID, using its procurement policy and guidelines, will give back any unspent funds to DFID, who then could either choose to enter into a direct agreement with the implementing partner, reimburse the suppliers for any costs they have already incurred or that will be necessarily incurred (and the supplier can’t be expected to avoid or recover). D. What is the assessment of financial risk and fraud? As most of the procurement will be done using USAID systems and the Implementing Agency will be providing Technical Assistance support, we judge the overall level of fiduciary risk for this programme to be low given the extensive financial controls in place for USAID contract management. This judgement is based on DFID’s corporate knowledge of USAID globally, satisfactory experience of working with and through USAID systems in comparable contexts (e.g. in Tanzania). Any potential risks of using these instruments as opposed to DFID- managed commercial contracts will be mitigated through the use of six-monthly tranched releases to USAID, based on quarterly financial and progress reports that are reviewed by programme staff, to ensure that the services provided are appropriate and of high quality and to ensure that funds are released only on clear evidence of financial need. E. How will expenditure be monitored, reported, and accounted for? Rigorous monitoring and accounting of expenditure will take place using ARIES in accordance to the ADAMANT principle to ensure value for money and compliance with Blue Book requirements and programme arrangements. USAID will monitor and account for expenditure and will submit to DFID a certified annual statement showing funds received and expended including quarterly financial and progress reports. The Implementing Agency will submit an annual audited account. The reporting will be a single process, with updates as required. Whilst primary accountability for DFID funds will reside with USAID through the agreed ACD, the implementing agency will be accountable to USAID. Management Case A. What are the Management Arrangements for implementing the intervention? The overall oversight of this project will be through the emerging government donor working group on reproductive and maternal health which is jointly lead by the GOT, USAID, and UNFPA. (This also means that DFID can work through USAID on high level political advocacy and gives DFID a seat at the policy discussion table.) This programme is a good example of donor coordination as DFID embarks on its fourth collaboration with USAID. Working with the lead RMH agency in partnership will allow certain flexibility to fill gaps of other donors from an overall menu of RMH supplies. While this programme will be managed by USAID, DFID will need to continue to engage with UNFPA and other DPs as multi-donor coordination will continue to be very important for this programme. (It is possible that another DP might be in a better position to carry out some activities and the programme needs to maintain the flexibility to do that.) The Donor-Government Joint Working Group has oversight of these activities. In addition, DFID and USAID will need to ensure synergies with other projects such as E4A. USAID will have general oversight of JSI and the USAID Family Planning Adviser (Activity Manager for the global A/OTAR) will supervise. The Agreement Officer’s Technical Representative (A/OTR) is at Headquarters and the Family Planning Advisor at USAID will serve as the local Activity Manager (AM) for the award in Tanzania. Specific certification requirements are outlined in USAID’s policies, Automated Directives System which is a web-based catalogue of USAID rules and regulations). Locally, the AM will: oversee the technical activities on the ground; develop and monitors the statement of work; is the Mission point of contact for visitors; is the Partner point of contact (responding to submitted reports); is responsible for writing up minutes for quarterly meetings and placing them on file; is responsible for site visits and submitting reports; and is responsible for tracking finances. When the agreement moves to a local one, the AM role will become that of the Agreement Officer’s Technical Representative (A/OTR), or C/AOTR which is the representative under a contract) who will work to ensure that USAID exercises prudent management over funds. The relevant sections of Automated Directives System (ADS) Chapter 303, "Grants and Cooperative Agreements to Non-Governmental Organizations," state the specific duties, authorities, and limitations that accompany this designation. The ADS 303; 22 CFR 226, "Administration of Assistance Awards to U.S. Non-Governmental Organizations"; and Contract Information Bulletins (CIBs) or Acquisition and Assistance Policy Directives (AAPDs) issued periodically lays out the role and responsibility USAID mandates for oversight of its agreements http://www.usaid.gov/policy/ads/300/ Page 34 of the ADS describes the pre award survey as we would move to a new agreement- the survey team examines the applicant’s systems to determine whether the prospective recipient has the necessary organization, experience, accounting and operational controls, and technical skills — or the ability to obtain them — in order to achieve the objectives of the programme. USAID’s Family Planning Strategy and how this programme fits. The USAID Health and Population Office have updated its strategic vision under the BEST programme. USAID’s Family Planning priorities include (in order of priority): improve contraceptive security and advocate for supportive government policies including sufficient financing and budget line items (continued and expanding) under the NFP CIP and fund new partnerships with private and faith- based/non-governmental sector for commodities; increase access to a broad method mix (provide a regular supply of a complete range of methods) through scale-up of outreach services under a coordinated ‘Catch-Up’ Campaign and through scale up of partnership with local faith based and private sector partners; scale up youth friendly communication and services including a focus on adolescent pregnancy; broaden communication efforts to include promotion of healthy timing and spacing and address persistent myths and misconceptions; increase availability and skills of providers to deliver long-acting and permanent methods and expanded access of post-partum intrauterine contraceptive device delivery; introduce programming to access emergency contraception and scale up post-abortion care services from the current 21 districts to all 131 districts; counsel all women and couples on the range of FP methods when accessing MCH and HIV/AIDS services; and initiate training and task shifting of minilaparotomy under local anesthesia to clinical officers, and continued outreach services. Management structure within DFID: This programme will be managed by the DFID MDG Advisor, with the support of Deputy Programme Manager, based in Tanzania. The DFID programme team will meet at least quarterly with the COTAR in USAID. Quarterly or other reports on the programme will be shared with DFID. Quarterly progress and financial reports will be produced as well as annual reviews. Regular monitoring will be conducted and reports shared with DFID on a semi-annual basis. DFID will undertake annual project reviews. Any revision of the KPIs will be done as part of the annual review process and this will be linked and jointly conducted. Financial reports, compliance and administrative functions will be managed by the USAID and shared with the DFID programme team. Management by USAID. Management by USAID will be as described above as mandated by USAID regulations and policies. Additional information is provided below for financial management, for family planning compliance, and for site visit and environmental compliance. The Mission’s Site Visit Checklist, the Environmental Impact Evaluation and mitigation plan, The Family Planning Compliance checklists for the Mission have all been provided to DFID for documentation in detail of oversight procedures. Financial oversight includes: Ensuring that all funding actions comply with USAID's forward funding guidelines (ADS 602, Forward Funding of Program Funds). Reviewing the recipient's request for payments or financial reports and providing or denying administrative approval if required by the procedures in ADS Chapter 630, Payables Management. Monitoring the financial status of the award on a regular basis to ensure that the level of funding is the minimum necessary. Developing accrued expenditures on a quarterly basis in accordance with ADS 631, Accrued Expenditures, and instructions from M/FM or the mission controller. Reviewing and documenting the review (for example, signing and dating a copy of the financial report) of financial status reports for U.S. organizations with letters of credit and periodic advance payments to monitor financial progress. Initiating a request to the agreement officer to deobligate funds if at any point it is apparent that the amount of available funds is more than will be necessary to complete the cooperative agreement activities (see ADS 621 Obligations and Internal Mandatory Reference “Deobligation Guidebook”). Monitoring recipient compliance with the requirement for them to obtain any host country tax exemptions for which they are eligible; and Upon completion of the work under the award, reviewing any unliquidated obligation balance in the award and working with the agreement officer to deobligate excess funds before beginning close-out actions. Site visits are an important part of effective award management because they usually allow a more effective review of the project. When USAID makes a site visit, the AO or AOTR must write a brief report highlighting his or her findings and put a copy in the official award file. Family planning compliance is an area of great importance to the USG and principles of voluntarism and informed choice guide USAID's family planning programme. These principles are articulated in programme guidelines and a number of legislative and policy requirements that govern the use of U.S. family planning assistance. USAID works with partners to ensure compliance with the family planning requirements in their programmes. This is mandatory and must be well documented and reviewed on an on-going and stringent basis. B. What are the risks and how these will be managed? Table 16: Assessment of risks Risk Description Risk 1 Fiduciary risks Impact on Success (L,M,H) M Probability of Occurring (L,M,H) L Mitigating Actions Main procurement is through USAID that has robust process for managing procurement and funds Maintain good dialogue with USAID and suggest additional junior staff, if required Undertake consultative meetings with GOT at all levels to galvanize support and ownership Risk 2 USAID staff may be overstretched Risk 3 Inadequate engagement and support from GOT L-M M Risk 4 Fragmentation of work in health sector with many priorities and DPs Political risks: US Government political change makes funding of family planning impossible Change of provider by USAID during course of support M M DFID is working with lead partner in the RH sector. USAID will be coordinating priorities and partners. M M DFID will consider the option of switching funding to another partners – such as UNFPA if this occurs L M DFID will consider the option of directly funding JSI or to remain funding through JSI Risk 5 Risk 6 Monitoring Mechanism DFID will monitor USAID will oversee and JSI responsible for monitoring USAID will coordinate and DFID will monitor DFID will monitor policy changes within USAID DFID will keep in close contact with USAID Risk 7 Conservative backlash toward family planning activities in Tanzania M L Political advocacy is built into programme activities DFID and USAID will monitor. C. What conditions apply (for financial aid only)? Not applicable, as the programme does not involve financial aid to government. D. How will progress and results be monitored, measured and evaluated? There are strong synergies between this project and evidence for action the regional project that will operate in Tanzania, focusing on maternal health data quality and use. This project is in the design phase. It is likely that they may develop indicators that will be more reliable, and the logframe should be reviewed once this project is operational. JSI the logistics contractor regularly surveys 640 facilities across the country on a six monthly basis to review the availability of malaria drugs. They will add reproductive and maternal health commodities to this process. Monitoring advocacy and policy change is more difficult and these indicators in particular will be refined with the evidence for action programme The results of this project will be fed directly into DFID framework for results around maternal and reproductive health . USAID Tanzania has formalized monitoring and evaluation plans as part of their approach for Managing for Results. The Mission rigorously and systematically assesses progress towards desired results using a results framework and performance management plan (PMP). USAID also requires portfolio reviews for investments and partnerships, field visits, data quality assessments, evaluations and quarterly and annual reports. All partners would have a PMP, which measures output and outcome levels and are gender sensitive. The central agreement’s PMP is on file at headquarters and with a new local award, the PMP will be developed and managed from USAID Tanzania. USAID/Tanzania’s Mission Order for Performance Monitoring and Evaluation Framework has been made available to DFID. An M&E plan is currently in place to which JSI is accountable to USAID. JSI submits quarterly summary reports to USAID and DFID documenting progress against the annual workplan, monitoring plan and logframe. The programme will be reviewed internally on an annual basis through DFID systems. At this stage DFID Tanzania is not planning an independent evaluation. It is possible that it may be included in some of the learning and evaluation that is being co-ordinated across the organisation around maternal heatlh Lograme Quest No of logframe for this intervention: i ibid SCIENCE IN ACTION: Saving the lives of Africa’s mothers, newborns and children (2009). Tanzanian Demographic and Health Survey (TDHS), 2010. iv ibid v TDHS 2010 vi UN population estimates 2011 vii TDHS, 2010. viii PRB (2010) Contraceptive security for policy audiences: An Overview. Washington, DC, Population Reference Bureau. ix SCIENCE IN ACTION: Saving the lives of Africa’s mothers, newborns and children (2009). x Tanzania DHS 2010. xi Kruk, ME et al (2009) Women’s Preference for place of delivery in rural Tanzania: A populationbased discrete choice experiment. American Journal of Public Health Vol 99, No 9. xii TDHS 2010. xiii World Health Organisation (2007) Maternal Mortality in 2005. Estimates developed by WHO, UNICEPF, UNFPA and the World Bank. xiv Cleland, J (2006) Op cited. xv Population Reference Bureau (2009) Family planning Saves Lives. xvi The National Road Map Strategic Plan to Accelerate Reduction of Maternal, Newborn and Child Deaths in Tanzania 2008 – 2015 (2008). xvii Ibid xviii Contraceptive Method Mix (1994) Geneva: World Health Organisation. xix Singh, s et al (2009) Adding it up: the benefits of investing in sexual and reproductive healthcare. UNFPA: Guttmacher Institute. xx African Science Academy Development Initiative (2009) Science in Action: Saving the lives of Africa’s mother, newborns, and children. xxi International Confederation of Midwives (ICM) and International Federation of Gynaecology and Obstetrics (FIGO) (2006). Prevention and treatment of postpartum haemorrhage: New advances for low resource settings. London: ICM and FIGO. xxii Tse, V and P Coffey (2009) New and underutilised technologies to reduce maternal mortality and morbidity: What progress have we made since Bellagio 2003? British Journal of Obstetrics and Gynaecology 116. xxiii Neilson, JP. (1995) Magnesium sulphate: the drug of choice in eclampsia. BMJ Vol 311. xxiv Altman, D et al. (2002) Do women with pre-eclampsia, and their babies, benefit from magnesium sulphate? The Magpie Trial: a randomised placebo-controlled trial. Lancet 359. xxv Tsu, V and P Coffey (2009) New and underutilised technologies to reduce maternal mortality and morbidity: What progress have we made since Bellagio 2003? British Journal of Obstetrics and Gynaecology 116: 247-56. xxvi Muganyizi, P and M Shagdara (2011) Predictors of extra care among magnesium sulphate treated eclamptic patients at Muhimbili National Hospital, Tanzania. BMC Pregnancy and Childbirth Vol 11. xxvii Tsu, V and P Coffey (2009) New and underutilised technologies to reduce maternal mortality and morbidity: What progress have we made since Bellagio 2003? British Journal of Obstetrics and Gynaecology 116: 247-56. xxviii Seligman, B. And X. Liu. (2006) Economic Assessment of Interventions for Reducing postpartum Haemorrhage in Developing countries. Abt Associates, Inc. xxix WHO (2007) WHO recommendations for the prevention of PPH. Geneva: WHO. xxx WHO, 2004. Making pregnancy safer: The critical role of the skilled attendant. A joint statement by WHO, ICM and FIGO. xxxi The Prevention of Maternal Mortality Network, 1995. Situation analyses of emergency obstetric care: Examples from eleven operations research projects in West Africa. Social Science and Medicine, 40(5), pp.657-67. xxxii World Health Organisation, 2005. World Health Report 2005: Make every mother and child count. Geneva: WHO. xxxiii Sundari, T.K., 1992. The untold story: How the healthcare systems in developing countries contribute to maternal mortality. International Journal of Health Service, 22(3), pp.513-28. xxxiv WHO, 2004. Pregnancy, Childbirth, Postpartum, and Newborn Care (PCPNC): A guide for essential practice. Geneva: WHO. ii iii xxxv WHO, IPPF, JSI Inc., PATH, PSI, UNFPA, WB, 2006. The interagency list of essential medicines for reproductive health. Geneva: WHO Departments of Medicine Policy and Standards and Reproductive Health and Research. xxxvi World Health Organisation, 2002. How to develop and implement a national drug policy. Geneva: WHO. xxxvii Hutin, Y.J., Hauri, A.M., Armstrong, G.L., 2003. Use of injections in healthcare settings worldwide, 2000: Literature review and regional estimates. British Medical Journal, 327(7423), pp.1075; Nazerali, H., Muchemwa, T., Hogerzeil, H.V., 1996. Stability of essential drugs in tropical climates: Zimbabwe. Geneva: WHO; Hogerzeil, H.V., Walker, G.J., 1996. Instability of (methyl)ergometrine in tropical climates: An overview. European Journal of Obstetrics, Gynecology and Reproductive Biology, 69(1), pp.25-9. xxxviii Oyesola, R., Shehu, D., Ikeh, A.T., Maru, I., 1997. Improving emergency obstetric care at a state referral hospital, Kebbi State, Nigeria. International Journal of Gynaecology and Obstetrics, 59 (2), pp.75-81. xxxix The Prevention of Maternal Mortality Network, 1995. Situation analyses of emergency obstetric care: Examples from eleven operations research projects in West Africa. Social Science and Medicine, 40(5), pp.657-67. xl Druce, N., 2006. Reproductive health commodity security (RHCS): Country case studies synthesis: Cambodia, Nigeria, Uganda and Zambia. DFID Health Resource Centre. xli Leahy, E., 2009. Reproductive health supplies in six countries. Themes and entry points in policies, systems and financing. Population Action International. xlii Druce, N., 2006. Reproductive Health Commodity Security (RHCS): Country case studies synthesis: Cambodia, Nigeria, Uganda and Zambia. London: DFID Health Resource Centre. xliii Bradford, C (2011) Tanzania Reproductive and Maternal Health Commodities. Trip Report, November 2011. xliv REPORT OF THE CONTROLLER AND AUDITOR GENERAL ON SPECIAL AUDIT ON DRUGS AVAILABILITY AT MEDICAL STORES DEPARTMENT (MSD) FOR THE PERIOD FROM 30 JUNE 2009 TO 30 JUNE 2011 xlv Interview with UNFPA, 1 November 2011. xlvi 2010 World Population Data Sheet. Washington, DC: Population Reference Bureau. xlvii The Economics of Climate Change in the United Republic of Tanzania. Global Climate Adaptation Partnership. Final Draft 2010 xlviii Wheeler D and Hammer D, The Economics of Population Policy For Carbon Emissions Reduction in Developing Countries. Centre for Global Development Working Paper 22.9 November 2010 xlix http://www.owen.org/blog/4105 last accessed 17th November 2010 l Ibid. li Ross, J. et al (2009) Contraceptive projections and the donor gap: Meeting the challenge. Brussels: Reproductive Health Supplies Coalition. lii Hubacher et al (2008) Unintended pregnancy in sub-Saharan Africa: Magnitude of the problem and the potential role of contraceptive implants to alleviate it. Contraception 78(1). liii Ibid liv Wickstrom, J and R Jacobstien (2011) Contraceptive Security: Incomplete without long-acting and permanent methods of family planning. Studies in Family Planning Vol 42, Number 4. lv Seligman, B. And X. Liu. (2006) Economic Assessment of Interventions for Reducing postpartum Haemorrhage in Developing countries. Abt Associates, Inc. lvi Kinney et al (20019) Science in action: Saving the lives of Africa’s mother, newborns and children. Cape Town, South Africa; Report for the African Academy Science Development Initiative.