Hypertension Mgmt - ETCprotocols.org
advertisement
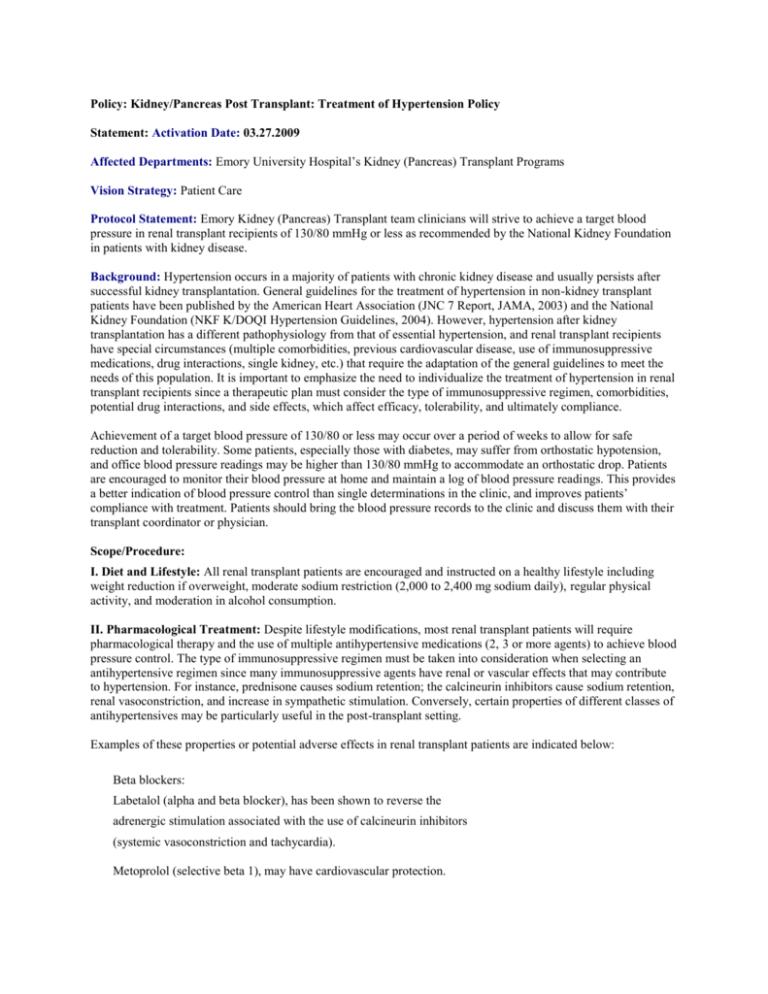
Policy: Kidney/Pancreas Post Transplant: Treatment of Hypertension Policy Statement: Activation Date: 03.27.2009 Affected Departments: Emory University Hospital’s Kidney (Pancreas) Transplant Programs Vision Strategy: Patient Care Protocol Statement: Emory Kidney (Pancreas) Transplant team clinicians will strive to achieve a target blood pressure in renal transplant recipients of 130/80 mmHg or less as recommended by the National Kidney Foundation in patients with kidney disease. Background: Hypertension occurs in a majority of patients with chronic kidney disease and usually persists after successful kidney transplantation. General guidelines for the treatment of hypertension in non-kidney transplant patients have been published by the American Heart Association (JNC 7 Report, JAMA, 2003) and the National Kidney Foundation (NKF K/DOQI Hypertension Guidelines, 2004). However, hypertension after kidney transplantation has a different pathophysiology from that of essential hypertension, and renal transplant recipients have special circumstances (multiple comorbidities, previous cardiovascular disease, use of immunosuppressive medications, drug interactions, single kidney, etc.) that require the adaptation of the general guidelines to meet the needs of this population. It is important to emphasize the need to individualize the treatment of hypertension in renal transplant recipients since a therapeutic plan must consider the type of immunosuppressive regimen, comorbidities, potential drug interactions, and side effects, which affect efficacy, tolerability, and ultimately compliance. Achievement of a target blood pressure of 130/80 or less may occur over a period of weeks to allow for safe reduction and tolerability. Some patients, especially those with diabetes, may suffer from orthostatic hypotension, and office blood pressure readings may be higher than 130/80 mmHg to accommodate an orthostatic drop. Patients are encouraged to monitor their blood pressure at home and maintain a log of blood pressure readings. This provides a better indication of blood pressure control than single determinations in the clinic, and improves patients’ compliance with treatment. Patients should bring the blood pressure records to the clinic and discuss them with their transplant coordinator or physician. Scope/Procedure: I. Diet and Lifestyle: All renal transplant patients are encouraged and instructed on a healthy lifestyle including weight reduction if overweight, moderate sodium restriction (2,000 to 2,400 mg sodium daily), regular physical activity, and moderation in alcohol consumption. II. Pharmacological Treatment: Despite lifestyle modifications, most renal transplant patients will require pharmacological therapy and the use of multiple antihypertensive medications (2, 3 or more agents) to achieve blood pressure control. The type of immunosuppressive regimen must be taken into consideration when selecting an antihypertensive regimen since many immunosuppressive agents have renal or vascular effects that may contribute to hypertension. For instance, prednisone causes sodium retention; the calcineurin inhibitors cause sodium retention, renal vasoconstriction, and increase in sympathetic stimulation. Conversely, certain properties of different classes of antihypertensives may be particularly useful in the post-transplant setting. Examples of these properties or potential adverse effects in renal transplant patients are indicated below: Beta blockers: Labetalol (alpha and beta blocker), has been shown to reverse the adrenergic stimulation associated with the use of calcineurin inhibitors (systemic vasoconstriction and tachycardia). Metoprolol (selective beta 1), may have cardiovascular protection. Carvediol may be particularly useful in patients with heart failure. Calcium channel blockers: Dihydropyridines (i.e., nifedipine, amlodipine): counteract the renal vasoconstriction caused by calcineurin inhibitors. They may be particularly useful in the perioperative period after renal transplantation and in patients with delayed graft function. Nifedipine XL is particularly useful since it allows rapid titration of the dose. Longer acting dihydropyrines (i.e., amlodipine) may be more useful in the outpatient setting, or in patients with mild hypertension. Non-dihydropyridines (diltiazem, verapamil): less potent than dihydropyridines, and should be used carefully since they increase concentration of cyclosporine, tacrolimus and sirolimus due to inhibition of hepatic metabolism. ACE inhibitors or angiotensin receptor blockers (ARBs): are antiproteinuric and have been shown to confer cardioprotection and renal protection in patients with cardiovascular disease and/or diabetes, although these studies have not been conducted in the renal transplant population. For this reason, most patients after kidney transplantation may benefit from the use of an ACE inhibitor or an ARB. They should be used cautiously, or avoided, in patients with delayed graft function or ATN, in patients at risk for volume depletion, and in patients with acute calcineurin nephrotoxicity. ACE inhibitors or ARBs may cause anemia in some renal transplant patients. Diuretics: Should be used carefully in renal transplant recipients because of their tendency to volume depletion and worsening renal function. They are indicated in patients with clinical volume overload (i.e, peripheral edema) or in patients with congestive heart failure. K-sparing diuretics (spironolactone, amiloride, etc) should be avoided because of their tendency to hyperkalemia (potentiated by calcineurin inhibitors and trimetoprimsulfametoxazole) General Guidelines: General guidelines for the management of hypertension in the initial and late post-transplant period are as follows: I. Initial post-transplant period (Months 1-3). First choice agents: Beta blockers (i.e., metoprolol or labetalol), and/or calcium channel blockers (i.e, Nifedipine XL) alone or in combination. ACE inhibitors or ARBs may be used initially in living donor recipients, and in patients with excellent initial renal function and low risk for volume depletion. They should be avoided in patients with delayed graft function, patients with poor oral intake or GI toxicity due to the risk of volume depletion. Diuretics should be avoided initially because of the risk of volume depletion, unless evidence of volume overload. Additional agents may be added as needed: alpha 2 agonists, direct vasodilators (hydralazine) or diuretics. Alpha blockers may be particularly useful in patients with prostatism and urinary retention. II. Long-term management (after Month 3). First choice agents: Beta blockers, Calcium channel blockers, ACE inhibitors or ARBs alone or in combination. Patients with proteinuria: ACE inhibitors or ARBs due to their antiproteinuric effect. Non-dihydropyridine calcium channel blockers (diltiazem and verapamil) have mild antiproteinuric actions, but should be used carefully because they increase calcineurin inhbitor and sirolimus levels by inhibiting their metabolism. Patients with CHF and low ejection fraction: ACE inhibitors and ARBs. Alternatively, hydralazine and oral nitrates. Additional agents: diuretics (if edema), alpha 2 agonists and/or direct vasodilators (i.e., hydralazine). III. Special conditions (ICU setting, inability to take oral medications, etc). In circumstances where oral medications cannot be given or rapid control of blood pressure may be required, intravenous antihypertensives could be given. Examples of intravenous drug preparations are: Hydralazine 10-20 mg iv every 3-6 hours. Labetalol 20-40 mg iv every 3-4 hours, or 0.5-2 mg/min constant infusion. Esmolol, nicardipine or sodium nitroprusside drips are also very effective. NOTE: Caution should be exercised when using nicardipine since it can increase the blood levels of calcineurin inhibitors and sirolimus. References: Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, Jones DW, Materson BJ, Oparil S, Wright JT Jr, Roccella EJ: The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: The JNC 7 report. JAMA 289: 2560–2572, 2003 K/DOQI Clinical Practice Guidelines on Hypertension and Antihypertensive agents in Chronic Kidney Disease. Am J Kidney Dis 43: S1–S230, 2004 Medical Care of the Kidney Transplant Recipient after the First Posttransplant Year. Djamali et al. Clin J Am Soc Nephrol 1: 623-640, 2006 Midtvedt K, Hartmann A: Hypertension after kidney transplantation: Are treatment guidelines emerging? Nephrol Dial Transplant 17: 1166–1169, 2002 National Kidney Foundation: KDOQI Clinical Practice Guidelines and Clinical Practice Recommendations for Anemia in Chronic Kidney Disease. Am J Kidney Dis 47:S1-S145, 2006 (suppl 3) Approved by: Renal Transplant Leadership Group ________________________________________ Thomas C. Pearson, M.D., D.Phil. Director, Emory Kidney and Pancreas Transplant Programs Chair, Renal Transplant Leadership Group Approval Date: 05/21/2008, 10/22/2008 Revised: 12/09/2009