2013 APRN Program Preceptor Interview Results Final February
advertisement

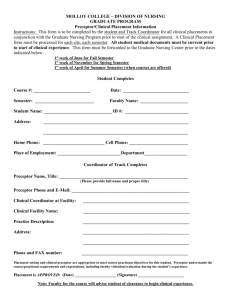
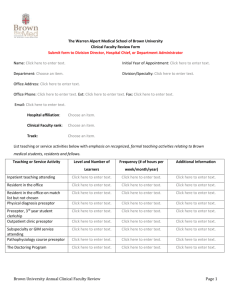
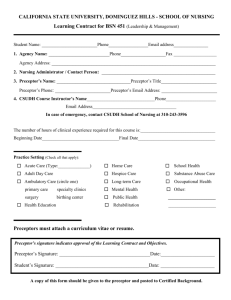
2013 APRN Program Preceptor Interview Results Final February 2014 Programs included: University of North Dakota, North Dakota State University, University of Mary and Minnesota State University Moorhead 1. What graduate programs does your college/university offer? UND- Master’s degrees: AGPCNP, FNP, PMHNP, AGCNS, CRNA, Nurse Educator, APHN, Post- Master’s DNP, PhD NDSU- DNP, Nurse Educator MS U of Mary- FNP soon DNP, Nurse Administrator/Nurse Educator MSUM- Nurse Educator and the Nurse Admin/Organizational Systems Leadership (NAOSL) Which of these include the use of clinical sites and preceptors in North Dakota? UND- AGPCNP, FNP, PMHNP, AGCNS, CRNA, APHN NDSU- DNP- has preceptors in ND, MN, SD U of Mary- FNP MSUM- Both have ‘clinical’ experiences although the number in ND are limited as most of our students are currently living outside ND. 2. Please explain your program’s process for setting up graduate clinical placement sites. UND- AGPCNP, FNP and AGCNS: Students are asked to help identify qualified preceptors and to make an initial contact to determine willingness (may or may not include assistance of faculty in identifying previous preceptors, professional contact – or sometime looking at websites) If preceptors is willing, course faculty make contact to determine if placement and person are appropriate for course and objectives. In some cases (certain facilities) students or faculty are to contact an education or clinical coordinator to request clinical placement in the facility – this process is then totally handled by the coordinator and student is “placed”. Faculty also handle ensuring contracts are in place with facility, getting handbook and info to preceptors and ensuring appropriate paperwork is on file before students start clinical. UND- Post- MS DNP: Has not been determined yet; most likely have students look for sites first UND- APHN: Some student use their work sites (if appropriate) otherwise they are asked to help identify qualified preceptors and to make an initial contact to determine willingness course faculty then make contact to determine if placement and person are appropriate for course and objectives. NDSU-DNP- networking, have a discussion with students on their 1st day that when they start they should anticipate that they will be helping to set up clinical placement sites. Students from a small community will negotiate with the provider in their community. Advantageous for the student as they then have a place to stay during their placement. UND CRNA- Generally this first step is to identify a clinical site that would be good fit for our students and the program. Sometimes we are approached by CRNA’s from an interested site...other times we approach the site. We usually end up doing a site visit to talk more about the potential relationship. Once we determine that the interest exists and the site would be a good fit, the next step is to collect data and submit an application to the Council on Accreditation of Nurse Anesthesia Educational Programs, as all of sites need to be approved. We also have internal agreements that are completed through the College of Nursing and Professional Disciplines. U of Mary-FNP- We work together with student and they complete a preceptor data sheet. They pick three preceptors of choice and submit to our graduate clinical placement liaison. She then calls the sites and negotiate to the placement. U of Mary keeps a database of previous preceptors that they can use or have a personal connection. Usually someone they have had before. MSUM- Generally it is a collaboration between the student (who has some ideas and contacts) and the instructor. One or both contact the potential site to arrange the experience. Ultimately, we have an interagency agreement or Practicum agreement established. The agreement development is done by the faculty. 3. Do you have a coordinator or does individual faculty set up the placements? UND- Individual Faculty from each track NDSU- The program director sets up the contact and coordinates the placements in partnership with the students. UND CRNA- Our students do not work with one specific clinical preceptor – they can work with any CRNA at the clinical site. We do have a clinical coordinator at each site that acts as a liaison between the clinical site and the program. This individual helps to facilitate learning experiences for the students, complete evaluations, and troubleshoot issues that may arise. U of Mary- Graduate clinical placement liaison. This is first year that we have had that and they are full time. MSUM- no 4. Do you have standardized paperwork that you use with all of your clinical placement sites? UND- Yes NDSU- Yes U Mary- Yes MSUM- Yes What type of paperwork does this include? UND- AGNP, AGCNS, FNP, PMHNP, APHN: Clinical Affiliation Agreement (agency), Memorandum of Agreement (preceptor), copy of license and certification (preceptor) NDSU- Contract, Standardized clinical education, preceptor handbook which includes objectives for our program and curriculum. UND-CRNA- Each one of our clinical sites has a binder that contains copies of our Student & Faculty Handbook, Clinical Preceptor Handbook, and Bloodborne Pathogen Exposure protocol. Within these handbooks are examples of the clinical paperwork that is encountered while working with our students – daily care plans, daily evaluations, clinical release time (Days off), and formative/summative clinical evaluations. This paperwork is fairly specific to students in our program. I’m unsure if using standardized clinical placement paperwork would work with our program. U of Mary- Preceptor data sheet, agency agreement (same one for all organizations), liability insurance- rarely do they change, HIPPA MSUM- We have standardized agreements as defined by MnSCU, our parent state organization. It can be a formal ‘interagency agreement’ (between MSUM and the hospital, clinic, etc) or it can be a practicum agreement which is much less complex –but still between the two agencies Would it be helpful to have standardized clinical placement paperwork available through a statewide program? UND- AGNP, AGCNS, FNP, PMHNP, APHN: Yes NDSU- Yes, although there are some unique aspects of each program. U of Mary- Yes, I believe so. MSUM- I don’t believe a ND standardized agreement would always work, but the more standardization possible, the better I think. 5. How do you find preceptors for your graduate program? UND- AGNP, AGCNS, FNP, PMHNP, APHN: Previous preceptors, student identified, faculty identified - Students are asked to help identify qualified preceptors and to make an initial contact to determine willingness (may or may not include assistance of faculty in identifying previous preceptors, professional contact – or sometimes looking at websites) If preceptor is willing, course faculty make contact to determine if placement and person are appropriate for course and objectives. In some cases (certain facilities) students or faculty are to contact an education or clinical coordinator to request clinical placement in the facility – this process is then totally handled by the coordinator and student is “placed”. UND- APHN: Also use student work sites Post- MS DNP: Will look for DNP students to start with their current employers NDSU DNP- It is a collaborative effort with the students. U of Mary- go through alumni quite a bit, maintain a database and utilize students personal connection and through faculty connections with faculty that work across the state-don’t need to go to any cold sites. MSUM- Generally through faculty or student networks, former students, sometimes through formal requests of an agency. 6. Does your program have a requirement that the preceptor be an advanced practice nurse or can a preceptor be an MD? UND- AGNP, AGCNS, FNP, PMHNP: Preceptor can be an MD or DO but some time with and APN is encouraged UND- Post- MS DNP: Will ask for DNPs, MDs, or upper administration UND- APHN: Must be a Mastered prepared nurse MSN or RN with MPH NDSU-DNP- Preceptor can be an MD, but only used as necessary if there are not enough FNPs to be preceptors. UND- CRNA- Yes. Clinical preceptors for our students can be either CRNAs or Anesthesiologists. With that being said, the vast majority of our clinical preceptors are CRNAs. It does depend on the site though – we have larger clinical sites with anesthesia care team models (CRNA/MD) and smaller, more rural sites that are independent CRNAonly practices. U of Mary- they can be an MD or could be a midwife or PA, but 200 of their hours has to be with a nurse pracitioners, use MDs often, really a mix- about ½ and ½ MSUM- The preceptor needs to be as close to the role for which the student is studying as possible. In our case, these are Nurse Educators or Nurse Admin/executives (or their designees). 7. Do you offer standardized orientation/training to your preceptors at all of your clinical placement sites? UND- No NDSU- have a preceptor handbook, the faculty member also contacts the preceptor at the beginning of the placement either on-site or by phone, orientation program UND- CRNA- We have many program alumni throughout our clinical sites that serve as clinical coordinators and preceptors, so there is a fair amount of familiarity with our program. We do an in-person orientation for each new clinical coordinator. In addition, we have a Clinical Preceptor Handbook that is available at each clinical site. The clinical coordinator and program administrators serve as resources for clinical preceptors who have questions or issues regarding students. U of Mary- no training, have an orientation booklet/packet that we send them, but no standardized training- will send to us MSUM- We do not offer preceptor training, as they are generally already ‘trained’ in the larger organizations or they have experience with education. What does it include? UND- n/a NDSU- Preceptor handbook which is under revision includes the role of the nurse practitioner, the NDSU graduate program curriculum including course descriptions and objectives, the role and responsibilities of the preceptor, faculty and student responsibilities to the preceptor and the student-faculty-preceptor agreement, evaluation information and all of the forms. Also includes appendices from NONPF Preceptor manual. U of Mary- expectations for a student, mission and values and what we are looking to get from that clinical- in addition to the handbook, for the specific course- we send them their specific objectives- more in actual handbook Would it be helpful to have a standardized statewide orientation/training program available? UND- YES!!!! NDSU- yes, although there will be components unique to the program UND- CRNA- I think there is potential for a statewide orientation/training program given that many of our preceptors are expert clinicians, but that does not make them expert educators. Perhaps if there were a training program that would cover teaching and evaluation strategies for preceptors? This may be an area of common ground for all APRN clinical preceptors. U of Mary- Yes MSUM- Preceptor training would be an excellent opportunity for many nurses/nurse educators. 8. How many preceptors does your students have over the course of their education program- do they stick with one or do they have many preceptors? UND- AGNP, AGCNS, FNP, PMHNP:: This varies some students have same throughout entire program – but most will rotate at least into some specialties (CV, GYN, ortho, derm etc…) UND- APHN: Try to stick with one preceptor for 500 hours over 3 semesters NDSU- DNP- customized to the student, have 1,000 hours of clinical time, sometimes they stick to a hub and spoke out to specialty areas, occasionally they work with one FNP for the entire time UND-CRNA- Our students typically graduate with around 2300 clinical hours. Each student rotates to between 3-5 clinical sites in rotations that are between 6-16 weeks in length. They don’t stick with one preceptor – they work with many different preceptors. U of Mary- they have multiple, over the course of the program they have about 15 through the different specialties- exposure to many different ways of doing things as possible, can discover different ways to do things. Do 900 hours total. They can request to stay with one. Those in Bismarck- try and request a repeat preceptor if they have a good experience MSUM- Generally they will have at least two or three with different foci in their clinical courses (individual, staff, system level, etc.). 9. How many hours do they spend with each preceptor? UND- AGNP, AGCNS, FNP, PMHNP: Varies, NP student need to complete 630 hours for our program 2-3 preceptors over a year, hours vary can be as few as 40 or as many as 225 UND- Post- MS DNP: will need 500 UND- APHN: 500 NDSU-DNP- customized to each student- need a total of 1,000 hours U of Mary- Between 8 and 300 hours with each preceptor depending on how many times they request a different preceptor and the class 10. Do you have facilities that provide housing and feed the graduate students? Is that something that has been requested or required for a rotation? UND-FNP: We state they may be required to travel. I don’t think it says “rural” UND- AGPCNP: Not yet but we are looking into it. UND- APHN: no NDSU-DNP- none of our facilities have done this, some of the smaller rural facilities might do this UND-CRNA- I would think this would be on the “wish-list” for many APRN programs. We have a couple sites that provide housing and food for students. For the majority of our sites, the student is responsible to cover the housing and food costs. We make sure they know this up front (during admission to the program). We do mention it to clinical sites, especially where affordable housing is an issue (i.e. Minot). But, we do not require it. U of Mary- no, that would be great. Very rarely there is a bed. Students would choose to stay with family or local. Some travel. MSUM- No to both questions. 11. Do you have language in your student handbook that graduate students would be expected to travel to a rural clinical placements? UND- We tell them we will do our best to help them find placements as close to their home as possible – but more and more are telling them that they should expect to have to travel. NDSU- This is a question we ask during their student interview- make sure they are aware that they might have to travel. Majority of our students have gone rural for their clinical placements. U of Mary- not required, encourage them. There is sentence or two that they may be expected to travel depending on supply and demand. Issues with students not wanting to travel. MSUM- No to both questions although this is a good idea! Do you require rural rotations? UND- Not yet – it is in the plans though UND- APHN: No NDSU- No, although most of them do go rural. UND- CRNA- Yes, all of our students are required to have rural clinical experiences. We make sure they are aware of this starting in the admission process and we also remind them when clinical assignments are being made for each class. It is also stated in our handbook. U of Mary- don’t require, looking to increase class sizes may look at requiring students to go rural- supply and demand. 12. What are the reasons students opt not to do a rural placement? Is if family, job, transportation or housing? UND- Family obligations, cost, travel, housing NDSU- convenience, may be working, have family or housing issues U of Mary- I don’t want to drive, because I have a family or I want to stay put, it is inconvenient. MSUM- Generally our students are already working full time, so being gone is difficult for the student and their employer. However, they do manage it when they are motivated and have the support of their supervisors. 13. Please describe any barriers that you have encountered in placing graduate students and in coordinating preceptors. UND- Accessing preceptors – not knowing who is available, organizations processes, deadlines/time constraints NDSU- Frequently it is the availability of preceptors, MSP is difficult right now U of Mary- big issue- everyone wants to stay where they are from in Bismarck, Fargo, Jamestown- challenge when multiple people request the same person- we do first come first serve- that is why they ask them to list three and can accommodate most. We have set dates for them to submit the paperwork that are early. Those with more hours are placed first- they get preference. The graduate student liaison checks back with the preceptor. Had some issues with a facility instituting EPIC and they didn’t want to take any during this period. Compete against med students, and area NPs. Have to look within a 50 or 100 mile radius for someone. Encourage students to look around for others. In Fargo, we request students submit five choices. Some MDs and Pas don’t want NP students, they only want MDs or PA students. MSUM- Understanding the role of the preceptor and the student needs/expectations. The completion of the contracts between agencies has impeded some placements. 14. What additional thoughts do you have about establishing a statewide preceptor program? University of Wisconsin?? Had a preceptor training modules that might be worth checking out –online cost $50 http://phc.portagecollege.ca/phc/course/login.asp http://nursing.uw.edu/academic-services/faculty/preceptors/preceptorclinicalaffiliate-faculty-support.html Consider recognition program as well – perhaps NDAC could sponsor an annual award for outstanding preceptors??? In other states they have used Medicaid/Medicare reimbursement money to pay for preceptors through a residency program (MD?) Compensation for the preceptors would be helpful and/or different productivity expectations Think it would be very important and good it is connecting APRNs. Even though we are connected virtually, feel disconnected and need to work together to support the states. The consistency this would bring would be very helpful for all I think. All the clinical sites and educational programs would be using the same language and have similar expectations of both the preceptors and the students. 15. If you are not already a member of the ND Center for Nursing Leadership Team and a member the preceptor workgroup, would you be interested in joining? Dean Gross-NDSU indicated that he would join. Jenna Herman- U of Mary indicated that she would join