FAQ
advertisement

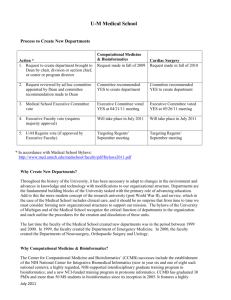
U-M Medical School Frequently Asked Questions & Answers About Creating New Departments 1. What is the purpose of medical school departments? Is the departmental structure still appropriate given sweeping changes to academic medicine? Academic departments are the fundamental functional unit in the organization of this and most universities, tasked with the primary role of advancing education. New fields and sub-fields emerge over time reflecting the growth and change in knowledge. As a result, throughout U-M’s history, it has been necessary to consider modifications to our structure to adapt to changes in the environment and advances in knowledge. Add to this the more modern concept of the research university (post World War II), and service, which in the case of the Medical School includes clinical care, and it should be no surprise that from time to time we must consider forming new organizational structures to support our mission. The bylaws of the University of Michigan and of the Medical School recognize the critical function of departments in the organization and each outline the procedures for the creation and dissolution of these units. The last time the faculty of the Medical School created new departments was in the period between 1999 and 2000. In 1999, the faculty created the Department of Emergency Medicine. In 2000, the faculty created the Departments of Neurosurgery, Orthopaedic Surgery and Urology. 2. Why do we need a Department of Computational Medicine & Bioinformatics? The Center for Computational Medicine and Bioinformatics’ (CCMB) successes include the establishment of the NIH National Center for Integrative Biomedical Informatics (now in year six and one of eight such national centers); a highly regarded, NIH-supported interdisciplinary graduate training program in bioinformatics; and a new NCI-funded training program in proteome informatics. CCMB has graduated 30 PhDs and more than 50 MS students in bioinformatics since its inception in 2005. It features a highly collaborative environment that has successfully built bridges to faculty across U-M in research and training. It is also a home for scholarly research in bioinformatics carried out by the CCMB core faculty who develop and apply computationally intensive techniques (such as computational protein folding, sequence pattern recognition and biomedical literature and data mining) to advance our understanding of biological processes, which are often medically relevant. CCMB works closely with the Michigan Institute for Clinical & Health Research (MICHR) and leads its Biomedical Informatics Program. The Department of Computational Medicine & Bioinformatics will be one of our basic science departments under the FAM III finance model. Recruitment of instructional track faculty in computational medicine and bioinformatics is highly competitive and our peer institutions are building their programs and departments. To remain competitive and attract the emerging scholars in this field to further enhance our faculty expertise, and to maintain our training program for the next generation of bioinformaticians, we propose the creation of the Department of Computational Medicine & Bioinformatics. CCMB will remain as an interdisciplinary center housed within the new department, charged with maintaining our important connections across U-M. July 2011 1 3. What are the pros and cons of creating a new Department of Computational Medicine & Bioinformatics? Pros: Enhanced recruitment and faculty retention Collaborative research is often dependent on bioinformatics and/or clinical informatics expertise; the new department will increase collaborative potential Increased potential to develop a curriculum to serve its growing cadre of trainees, PIBS trainees, and undergraduate medical students Stabilize and grow interactions with information technology groups to provide specialized expertise Sustain and grow national visibility Cons: Challenging financial performance of basic science departments Challenge of managing Bioinformatics inter-disciplinary graduate program (with its different financial model) Potential reduced cross-campus interaction as funds come solely from Medical School 4. Why do we need a Department of Cardiac Surgery? Cardiac Surgery continues to evolve new approaches to the spectrum of cardiac disease from congenital abnormalities to problems of the elderly. The Section of Cardiac Surgery in the Department of Surgery has a robust clinical program and strong participation in the education mission of the Medical School through residency education. Its successful research program will be expanded in the areas of health outcomes research and clinical trials with the recruitment of additional research faculty. The residency program will soon match its own residents separately from those of general surgery. It is anticipated that Cardiac Surgery’s transition to department status will enhance faculty recruitment, expand the clinical footprint, grow an excellent I-6 residency training program with continued collaboration with the Section of General Thoracic Surgery, grow funded research and enhance the faculty’s contributions to the Medical School and Faculty Group Practice. The section’s financial viability will put the new department on a solid financial foundation to meet the demands of independence. Like the four previous departments that emerged from the Department of Surgery between 1999 and 2001 (Emergency Medicine, Neurosurgery, Orthopaedics and Urology), Cardiac Surgery has a distinct and independent conceptual basis, an independent educational program and an independent framework for research. 5. What are the pros and cons of creating a Department of Cardiac Surgery? Pros: Enhanced recruitment and retention of faculty Improved performance and strategic planning within the Cardiovascular Center Facilitation of joint appointments as educational and training paradigms change Development of new paradigms of integrated clinical care and resident education Enhanced research potential July 2011 2 Cons: Negative financial impact on Department of Surgery Potential negative impact on Department of Surgery external image and reputation Challenge of managing Thoracic Surgery residency between two departments: Surgery and Cardiac Surgery Increased administrative overhead and burden 6. If we move forward to create these new departments, how will we identify a department chair for each? The Medical School has an established process whereby the sitting section chief or center director serves as the inaugural chair of a new department. That individual’s appointment is subject to Regent approval. 7. How do we identify faculty within a new department? In the case of the proposed Department of Cardiac Surgery which is currently a division within the Department of Surgery, faculty members who are part of the division will become faculty members of the new department, if approved. In the case of the proposed Department of Computational Medicine & Bioinformatics, there is a core faculty group affiliated with the Center for Computational Medicine and Bioinformatics’ (CCMB), a few of whom may become faculty of the new department. Both new departments will recruit additional faculty. 8. Will any faculty member appointments move from their current department to the Department for Computational Medicine and Bioinformatics? There are two faculty leaders whose appointments will move to the new department if the new department is approved. One additional faculty member is already in the unit with a primary appointment. All other faculty members with a secondary appointment in the Center for Computational Medicine and Bioinformatics will remain with their primary departments. New faculty will be recruited with a primary appointment in the new department. Research faculty in the unit will remain in the unit. 9. Is there a minimum number of faculty members necessary to create a new department? No. 10. If we move forward, when will these new departments become effective? With an affirmative vote by Executive Faculty of the Medical School, the proposal(s) will be submitted to a vote by the U-M Regents, likely at the September meeting. (The Regents do not meet in August.) With an affirmative vote by the Regents, the new department(s) would become effective later this fall. 11. Will the “parent” departments be harmed by this? In the case of cardiac surgery, if approved, the Department of Surgery would lose a portion of its budget and a portion of its overall margin. At the same time, the July 2011 3 Department of Surgery would no longer be responsible for various aspects of its previous management and operations since those would fall under the new department. In the case of Computational Medicine and Bioinformatics, there is no parent department. Instead, if approved, the Center for Computational Medicine and Bioinformatics’ (CCMB) will become an interdisciplinary center housed within the new department, acting as a nexus for collaboration across U-M in computational medicine and bioinformatics. 12. Why is thoracic surgery not being combined with cardiac surgery in this move toward department status? In many cases, cardiac and thoracic surgery activities are combined into a single department, despite their very different educational and clinical practice tracks. Here at the U-M Medical School, we have favored separating the two fields. There is no “right” answer and instead, the proposal is to move forward with two separate units based on clinical and research focus. 13. It is sometimes difficult to ensure adequate educational venues for trainees. What mechanisms are in place to ensure the educational program now split between Surgery and Cardiac Surgery remains intact and that accreditation requirements are met? Leadership of our departments has the responsibility to ensure their educational programs meet the goals of our education mission, including being accredited by the appropriate organizations. They are supported in these efforts by our Graduate Medical Education Office (GME) and the Dean’s Office. If approved, those involved who have any concerns should raise them immediately to department leadership as well as to Lisa Colletti, M.D., Associate Dean for House Officer/Resident Education, and the Dean’s Office. 14. How will a new cardiac surgery department impact the Cardiovascular Center operations? Will there be an impact on the partnership of the current three divisions (cardiology, vascular surgery and cardiac surgery) if one becomes a stand-alone department? The Cardiovascular Center (CVC) is an interdisciplinary unit with leadership that is representative of all participating departments. If approved, the new Cardiac Surgery department will also participate in the leadership of the CVC. 15. How can we afford to create new departments, particularly in this tough economic climate? The better question might be, “how can we afford not to respond to changing knowledge and shifting domains that have occurred in the conceptual framework of medicine?” Over time, the Medical School’s departmental structure has changed to reflect the world of medicine. Consider a time years ago when we had a Department of Syphology, which no longer exists as a result of changes in the way academic medicine and research are conducted and the way we educate students and trainees. Creating new departments requires resources. Investment decisions and trade-offs are part of the normal course of operations for the Medical School and the resources to July 2011 4 create these departments, if approved by faculty, will be identified through existing investment mechanisms. For the proposed Department of Cardiac Surgery, the new department would be well funded based on our early assessment of its operations. For the proposed Department of Computational Medicine & Bioinformatics, we have a funds flow model that is designed to ensure resources to support the basic sciences. In addition, the Dean’s Office would likely contribute funds to aid the leaders with recruiting and developing faculty. It is our responsibility to make the investment trade-offs necessary to fulfill our mission. 16. How can we afford to create a new basic science department, given the financial challenges experienced by most basic science departments and the increasing focus on clinical and translational research? Bioinformatics has become a foundational concept in the structure of medicine today. The Medical School is responsible for providing students and faculty with a robust bioinformatics structure, ensuring we are poised to educate and make major discoveries. The departmental structure is the best way to bring together our best minds and further our teaching and scholarship in this field. Clinical and translational research are dependent upon advances made in bio- and clinical informatics, and maintaining a comprehensive and robust informatics program is instrumental to our vision of creating the future of medicine through discovery. July 2011 5