2010/2011
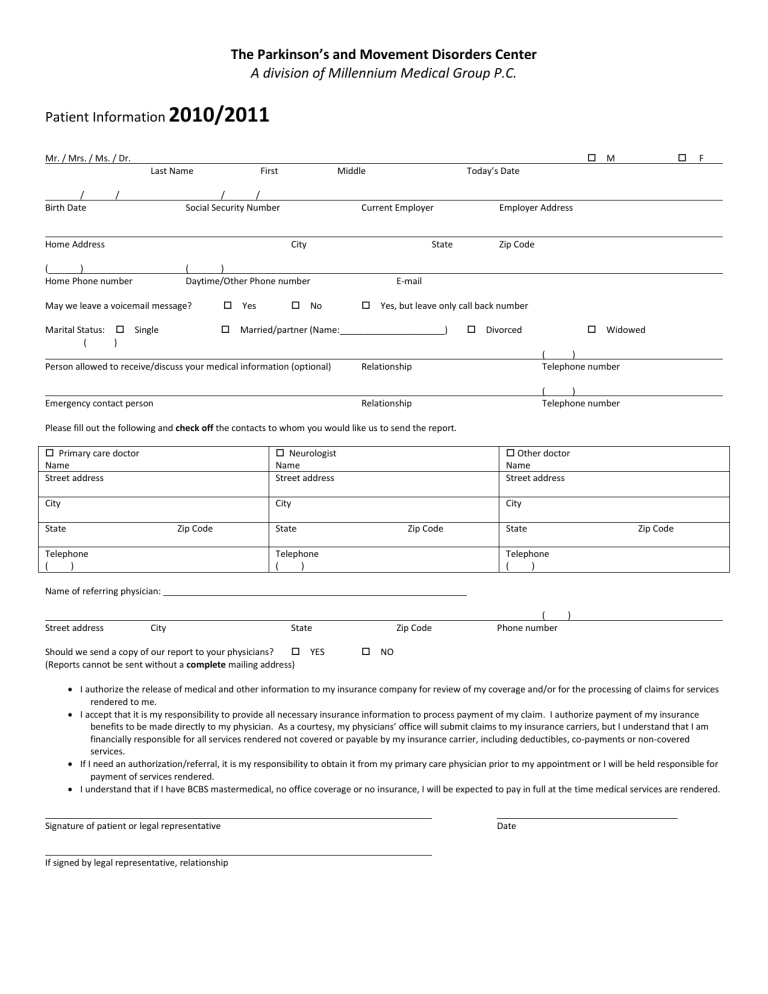
The Parkinson’s and Movement Disorders Center
A division of Millennium Medical Group P.C.
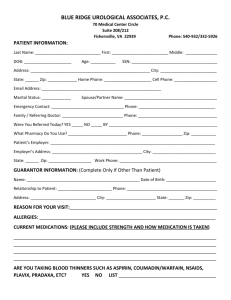
Patient Information
2010/2011
Mr. / Mrs. / Ms. / Dr.
Last Name First Middle Today’s Date
/
Birth Date
Home Address
/
( )
Home Phone number
/ /
Social Security Number
City
Current Employer
State Zip Code
Employer Address
( )
Daytime/Other Phone number
May we leave a voicemail message?
Marital Status: Single
( )
Yes No
Yes, but leave only call back number
Married/partner (Name:_____________________) Divorced
M
Widowed
F
Person allowed to receive/discuss your medical information (optional) Relationship
Relationship Emergency contact person
Please fill out the following and check off the contacts to whom you would like us to send the report.
Primary care doctor Neurologist
( )
Telephone number
( )
Telephone number
Name
Street address
City
State Zip Code
Telephone
Name
Street address
City
State Zip Code
Other doctor
Name
Street address
City
State Zip Code
( )
Telephone
( )
Telephone
( )
Name of referring physician:
Zip Code
( )
Phone number Street address City
Should we send a copy of our report to your physicians?
State
YES NO
(Reports cannot be sent without a complete mailing address)
I authorize the release of medical and other information to my insurance company for review of my coverage and/or for the processing of claims for services rendered to me.
I accept that it is my responsibility to provide all necessary insurance information to process payment of my claim. I authorize payment of my insurance benefits to be made directly to my physician. As a courtesy, my physicians’ office will submit claims to my insurance carriers, but I understand that I am financially responsible for all services rendered not covered or payable by my insurance carrier, including deductibles, co-payments or non-covered services.
If I need an authorization/referral, it is my responsibility to obtain it from my primary care physician prior to my appointment or I will be held responsible for payment of services rendered.
I understand that if I have BCBS mastermedical, no office coverage or no insurance, I will be expected to pay in full at the time medical services are rendered.
Signature of patient or legal representative Date
If signed by legal representative, relationship
Patient Name:______________________________ Date:______________________________
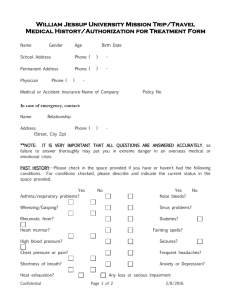
Symptomatic History:
Reason for today’s visit (diagnosis?):___________________________________________ Date of diagnosis:__________
What was/were your first symptom(s)? ________________________________________ When did it occur?__________
Who diagnosed you with the above condition(s)? Primary Care Physician Neurologist Other____
2
Medical History: Please check any of the following illnesses which you have had
___ Stroke
___Heart attack
___ Sleep apnea
___ Seizures
___ High blood pressure
___ Diabetes ___ Asthma
___ Liver hepatitis ___ Pancreatitis
___ Depression/anxiety
___ Migraine
___ Angina
___ Emphysema
___ Anemia
___ Neuropathy
___ Syncope
___ Low/high Thyroid
___ Arthritis
___ Bipolar disorder ___ Schizophrenia
___ Head Trauma
___ High Cholesterol
___ Kidney failure
___ Cancer
___ Alcoholism
List other past or present illnesses not noted above:
____________________________________________________________________________________________________________
____________________________________________________________________________________________________________
____________________________________________________________________________________________________________
Surgeries or Significant Trauma? No Yes (please describe, indicate year):
1. _____________________________________________
2. _____________________________________________
4. _____________________________________________
5. _____________________________________________
3. _____________________________________________ 6. _____________________________________________
Social History:
Years of education/highest degree_______ Most recent/primary occupation __________________________________________
Currently working Retired (year)___________ Disabled (year)___________
Living situation:
Smoking:
At home (with:_______________________)
Never Yes
*If yes - Cigarettes per day: _______
Assisted living and # of years: _______
Nursing facility
Yes, but Quit (date: ________________)
Alcohol: Never Yes
*If yes - Drinks/ week: ________
Gambling addiction?
Yes, but Quit (date: ________________) and # of years: _______
Recreational Drugs: Never Yes (describe): _______________________________________
Are you currently driving? No Yes
No Yes
Family History: Please indicate family members (parents, siblings, children, grandparents, aunt/uncles/cousins) with any of the following conditions
Parkinson’s disease
Tremor
Huntington’s chorea
Obsessive compulsive disorder
Alzheimer’s or other dementia
Tourette/tic disorder
Other movement disorder/genetic disorder
Other neurological condition
Depression/suicide
Mental illness
Gait disorder or ataxia
Mental retardation
Dystonia
Stroke
Heart disease
Other
Parent
Father
Mother
Living
Yes No
Yes No
Present age or age at death Cause of death or significant illness
Allergies: Please list any allergies to prescription medications or x-ray contrast dye: None
____________________________________________________________________________________________________________
____________________________________________________________________________________________________________
Patient Name:_____________________________________________________ Date:______________________________ 3
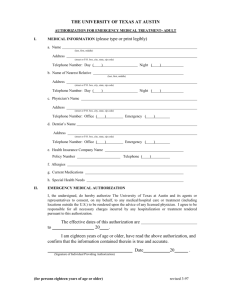
Please list all current Medications:
____________________________________________________________________________________________________________
____________________________________________________________________________________________________________
____________________________________________________________________________________________________________
____________________________________________________________________________________________________________
____________________________________________________________________________________________________________
____________________________________________________________________________________________________________
____________________________________________________________________________________________________________
____________________________________________________________________________________________________________
____________________________________________________________________________________________________________
Activities of Daily Living: Please indicate if you have difficulty in the following areas.
Normal Mild(infrequent, no help needed)
Moderate(occasional, may need some help)
Voice/Speech
Severe(frequent, requires assistance)
Marked(very frequent, unable to do)
Excess saliva/drooling
Swallowing
Handwriting
Feeding
Dressing
Bathing/toileting/hygiene
Turning in bed
Walking
Handling Medications
Shopping
Cooking/household chores
Handling finances/bills
Review of Symptoms: Please circle any current symptoms you currently have.
Constitutional: fatique/weakness, chills, sweats, hot flashes, weight loss, loss of appetite
Eye/ears/nose/throat: blurred vision, dry eyes, double vision, hearing loss, vertigo, choking, clear nasal drainage
Cardiac/pulmonary: chest pain, shortness of breath with activities, dizzy spells, palpitations, fainting, ankle swelling, wheezing, chronic cough
Gastrointestinal: nausea, vomiting, constipation, diarrhea, abdominal pain
Genitourinary: urine incontinence, urinary frequency, awakening to urinate, impotence
Musculoskeletal: muscle pain, joint pain, stiffness
Dermatological/ Allergy: Rash, itching, skin infection, decubitus ulcers
Neurological: headaches, numbness, tingling, limb weakness, lower back pain, cramps, muscle spasms, poor balance, falls, difficulty rising from a chair, tremor, loss of facial expression, word finding difficulty, impaired memory, confusion/disorientation
Endocrine: hair loss, dry skin, weight gain, edema
Hematological: bruising, blood clots, anemia, prolonged bleeding
Psychiatric: hallucinations, depression, anxiety attacks, forgetfulness, disorientation
Sleep: insomnia, sleep apnea/snoring, acting out /yelling in dreams, excessive daytime sleepiness, Restless Legs Syndrome


![[Section 1 - Health] Information - [ For Life/AD&D/Disability Benefits](http://s3.studylib.net/store/data/008027261_1-e3e10efdffb71df5932ae1b23a3d4b6b-300x300.png)