2016 Program Grant Application Form
advertisement
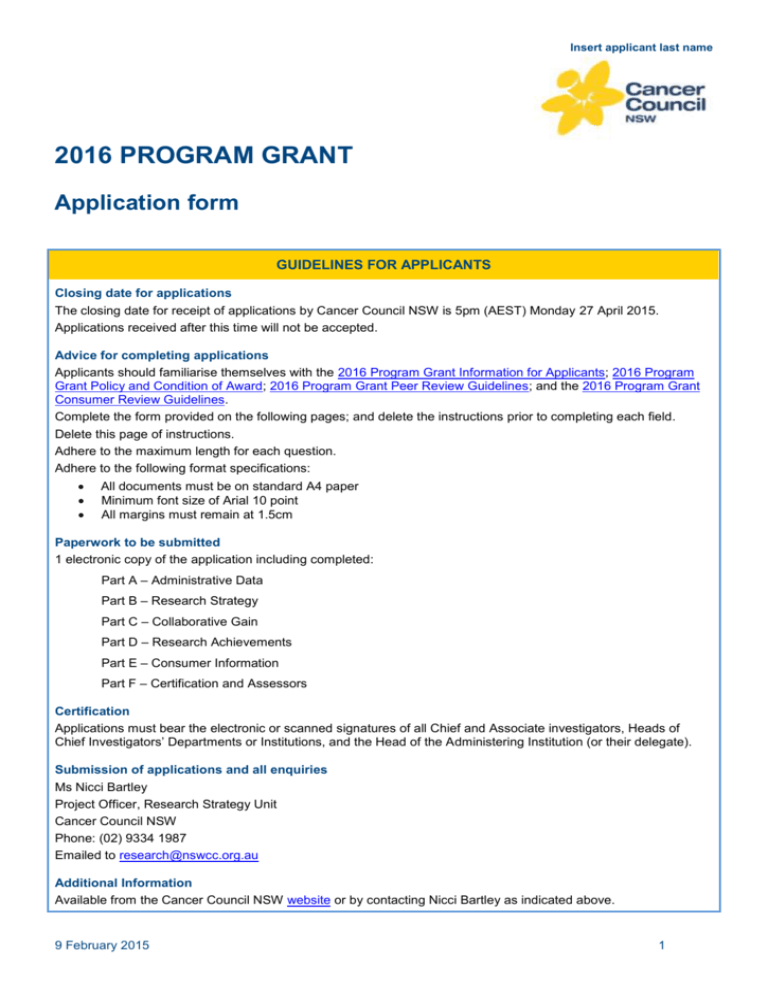
Insert applicant last name 2016 PROGRAM GRANT Application form GUIDELINES FOR APPLICANTS Closing date for applications The closing date for receipt of applications by Cancer Council NSW is 5pm (AEST) Monday 27 April 2015. Applications received after this time will not be accepted. Advice for completing applications Applicants should familiarise themselves with the 2016 Program Grant Information for Applicants; 2016 Program Grant Policy and Condition of Award; 2016 Program Grant Peer Review Guidelines; and the 2016 Program Grant Consumer Review Guidelines. Complete the form provided on the following pages; and delete the instructions prior to completing each field. Delete this page of instructions. Adhere to the maximum length for each question. Adhere to the following format specifications: All documents must be on standard A4 paper Minimum font size of Arial 10 point All margins must remain at 1.5cm Paperwork to be submitted 1 electronic copy of the application including completed: Part A – Administrative Data Part B – Research Strategy Part C – Collaborative Gain Part D – Research Achievements Part E – Consumer Information Part F – Certification and Assessors Certification Applications must bear the electronic or scanned signatures of all Chief and Associate investigators, Heads of Chief Investigators’ Departments or Institutions, and the Head of the Administering Institution (or their delegate). Submission of applications and all enquiries Ms Nicci Bartley Project Officer, Research Strategy Unit Cancer Council NSW Phone: (02) 9334 1987 Emailed to research@nswcc.org.au Additional Information Available from the Cancer Council NSW website or by contacting Nicci Bartley as indicated above. 9 February 2015 1 Insert applicant last name 2016 PROGRAM GRANT Application form: Part A Administrative Data PROGRAM TITLE CHIEF INVESTIGATOR(S) DETAILS Chief Investigator 1 (Chief Investigator 1 will be considered to be the contact point for the application and will be understood to be acting for and in concurrence with all Chief Investigators) Full name and title Department Institution Address City/Suburb, State, Postcode Telephone Email Current appointment Academic qualifications (degree, year, institution) Percentage of working time to be devoted to this Program % Percentage of working time to be devoted to all other Projects % % Percentage of working time to be devoted to all other Projects % Anticipated period(s) of absence (if any) and reason Chief Investigator 2 Full name and title Department Institution Address City/Suburb, State, Postcode Telephone Email Current appointment Academic qualifications (degree, year, institution) Percentage of working time to be devoted to this Program Anticipated period(s) of absence (if any) and reason Chief Investigator 3 Full name and title Department 9 February 2015 2 Insert applicant last name Institution Address City/Suburb, State, Postcode Telephone Email Current appointment Academic qualifications (degree, year, institution) Percentage of working time to be devoted to this Program % % Percentage of working time to be devoted to all other Projects Anticipated period(s) of absence (if any) and reason Please copy above table block and complete details for any additional Chief Investigators ASSOCIATE INVESTIGATOR(S) DETAILS Associate Investigator 1 Full name and title Department Institution Address City/Suburb, State, Postcode Telephone Email Current appointment Academic qualifications (degree, year, institution) Percentage of working time to be devoted to this Program % Percentage of working time to be devoted to all other Projects % % Percentage of working time to be devoted to all other Projects % Anticipated period(s) of absence (if any) and reason Associate Investigator 2 Full name and title Department Institution Address City/Suburb, State, Postcode Telephone Email Current appointment Academic qualifications (degree, year, institution) Percentage of working time to be devoted to this Program Anticipated period(s) of absence (if any) and reason 9 February 2015 3 Insert applicant last name Associate Investigator 3 Full name and title Department Institution Address City/Suburb, State, Postcode Telephone Email Current appointment Academic qualifications (degree, year, institution) Percentage of working time to be devoted to this Program % Percentage of working time to be devoted to all other Projects % Anticipated period(s) of absence (if any) and reason Please copy above table block and complete details for any additional Chief Investigators ADMINISTERING INSTITUTION CONTACT DETAILS Full name and title Department Institution Address City/Suburb, State, Postcode Telephone Email INSTITUTION(S) WHERE RESEARCH WILL BE CONDUCTED Institution Department Percentage of research effort Please copy above table block and complete details for any additional participating institutions 9 February 2015 4 Insert applicant last name COMMON SCIENTIFIC OUTLINE The common scientific outline is a classification system organised around seven broad areas of scientific interest in cancer research. It provides a framework to improve coordination among research organisations, making it possible to compare and contrast the research portfolios of public, non-profit, and governmental research agencies. Identify (x) the common scientific outline category(s) relevant to your Program. 1. Biology: Research included in this category looks at the biology of how cancer starts and progresses as well as normal biology relevant to these processes. 1.1 Normal Functioning – Developmental biology (from conception to adulthood) and the biology of ageing; Normal functioning of genes, including their identification and expression, and the normal function of gene products, such as hormones and growth factors; Normal formation of the extracellular matrix; Normal cell-to-cell interactions; Normal functioning of apoptopic pathways. 1.2 Cancer Initiation: Alterations in Chromosomes – Abnormal chromosome number; Aberration in chromosomes and genes (e.g., in chronic myelogenous leukemia); Damage to chromosomes and mutation in genes; Failures in DNA repair; Aberrant gene expression; Epigenetics; Genes and proteins involved in aberrant cell cycles. 1.3 Cancer Initiation: Oncogenes and Tumour Suppressor Genes – Genes and signals involved in growth simulation or expression, including oncogenes (Ras, etc.), and tumour suppressor genes (p53, etc); Effects of hormones and growth factors and their receptors such as estrogens, androgens, TGF-beta, GM-CSF, etc. 1.4 Cancer Progression and Metastasis – Latency, promotion, and regression; Expansion of malignant cells; Interaction of malignant cells with the immune system or extracellular matrix; Cell mobility, including detachment, motility, and migration in the circulation; Invasion; Malignant cells in the circulation, including penetration of the vascular system and extrasavation; Systemic and cellular effects of malignancy; Tumour angiogenesis and growth of metastases; Role of hormone or growth factor dependence/independence in cancer progression. 1.5 Resources and Infrastructure – Informatics and informatics networks; specimen resources; Epidemiological resources pertaining to biology; Reagents, chemical standards; Education and training of investigators at all levels (including clinicians), such as participation in training workshops, advanced research technique courses, and Master’s course attendance (this does not include longer-term research-based training, such as Ph.D or post-doctoral fellowships). 2. Etiology: Research included in this category aims to identify the causes or origins of cancer – genetic, environmental, and lifestyle, and the interactions between these factors. 2.1 Exogenous Factors in the Origin and Cause of Cancer – Lifestyle factors such as smoking, chewing tobacco, alcohol consumption, parity, diet, sunbathing, and exercise; Environmental and occupational exposures such as radiation, second-hand smoke, radon, asbestos, organic vapors, pesticides, and other chemical or physical agents; Infectious agents associated with cancer etiology, including viruses (Human Papilloma Virus-HPV, etc.) and bacteria (helicobacter pylori, etc.); Viral oncogenes and viral regulatory genes associated with cancer causation. 2.2 Endogenous Factors in the Origin and Cause of Cancer – Free radicals such as superoxide and hydroxide radicals; Genes known to be involved or suspected of being mechanistically involved in familial cancer syndromes, for example BRAC1, Ataxia Telangiectasia, and APC; Genes suspected or known to be involved in ‘sporadic’ cancer events, for example polymorphisms and/or mutations that may affect carcinogen metabolism (e.g., CYP, NAT, glutathione transferase, etc.). 2.3 Interactions of Genes and/or Genetic Polymorphisms with Exogenous and/or Endogenous Factors – Gene-environment interactions; Interactions of genes with lifestyle factors, environmental, and/or occupational exposures such as variations in carcinogen metabolism associated with genetic polymorphisms; Interactions of genes and endogenous factors such as DNA repair deficiencies and endogenous DNA damaging agents such as oxygen radicals or exogenous radiation exposure. 2.4 Resources and Infrastructure Related to Etiology – Informatics and informatics networks (e.g., patient databanks); Specimen resources (serum, tissue, etc.); Reagents and chemical standards; Epidemiological resources pertaining to etiology; Statistical methodology or biostatistical methods; Centres, consortia, and/or networks; Education and training of investigators at all levels (including clinicians), such as participation in training workshops, advanced research technique courses, and Master’s course attendance (this does not include longer term research based training, such as PhD or post-doctoral fellowships). 3. Prevention: Research included in this category looks at identifying interventions which reduce cancer risk by reducing exposure to cancer risks and increasing protective factors. Interventions may target lifestyle or may involve drugs or vaccines. 9 February 2015 5 Insert applicant last name 3.1 Interventions to Prevent Cancer: Personal Behaviours that Affect Cancer Risk – Research on determinants of personal behaviours, such as diet, physical activity, sun exposure, and tobacco use, that affect cancer risk; Interventions to change personal behaviours that affect cancer risk. 3.2 Nutritional Science in Cancer Prevention – Quantification of nutrients and micronutrients; Studies on the effect(s) of nutrients or nutritional status on cancer incidence; Dietary assessment efforts questionnaires and surveys; Development, characterisation, and validation of dietary/nutritional assessment instruments. 3.3 Chemoprevention – Chemopreventive agents and their discovery, mechanism of action, development, testing in model systems, and clinical testing. 3.4 Vaccines – Vaccines for prevention, their discovery, mechanism of action, development, testing in model systems, and clinical testing. 3.5 Complementary and Alternative Prevention Approaches – Discovery, development, and testing of complementary/alternative prevention approaches such as diet, herbs, supplements, or other interventions that are not widely used in conventional medicines or are being applied in different ways as compared to conventional medical uses. 3.6 Resources and Infrastructure Related to Prevention – Informatics and informatics networks (e.g., patient databanks); Specimen resources (serum, tissue, etc.); Epidemiological resources pertaining to prevention; Clinical trials infrastructure; Statistical methodology or biostatistical methods; Centres, consortia, and/or networks. 4. Early Detection, Diagnosis, and Prognosis: Research included in this category focuses on identifying and testing cancer markers and imaging methods that are helpful in detecting and/or diagnosing cancer as well as predicting the outcome or chance or recurrence. 4.1 Technology Development and/or Marker Discovery – Discovery of markers (e.g., proteins, genes), and/or technologies (such as fluorescence, nontechnology, etc.) that are potential candidates for use in cancer detection, staging, diagnosis, and/or prognosis; Use of proteomics, genomics, expression assays, or other technologies in the discovery of markers. 4.2 Technology and/or Marker Evaluation with Respect to Fundamental Parameters of Method – Development, refinement, and preliminary evaluation (e.g., animal trials and Phase 1 clinical trials); Preliminary evaluation with respect to laboratory sensitivity, laboratory specificity, reproducibility, and accuracy; Research into mechanisms assessing tumour response to therapy at a molecular or cellular level. 4.3 Technology and/or Marker Testing in a Clinical Setting – Evaluation of clinical sensitivity, clinical specificity, and predictive value (Phase II or III clinical trials); Quality assurance and quality control; Inter- and intra-laboratory reproducibility; Testing of the method with respect to effects on morbidity and/or mortality; Study of screening methods, including compliance, acceptability to potential screenees, and receiver-operator characteristics; Research into improvements in techniques to assess clinical response to therapy. 4.4 Resources and Infrastructure Related to Detection, Diagnosis, or Prognosis – Informatics and informatics networks (e.g., patient databanks); Specimen resources (serum, tissue, images, etc.); Clinical trials infrastructure; Epidemiological resources pertaining to risk assessment, detection, diagnosis, or prognosis; Statistical methodology or biostatistical methods; Centres, consortia, and/or networks; Education and training of investigators at all levels (including clinicians), such as participation in training workshops, advanced research technique courses, and Master’s course attendance (this does not include longer term research based training, such as Ph.D. or post-doctoral fellowships). 5. Treatment: Research included in this category focuses on identifying and testing treatments administered locally (such as radiotherapy and surgery) and systemically (treatments like chemotherapy which are administered throughout the body) as well as non-traditional (complementary/alternative) treatments (such as supplements, herbs). Research into prevention of recurrence is also included here. 5.1 Localised Therapies: Discovery and Development – Discovery and development of treatments administered locally that target the organ and/or neighbouring tissue directly, including but not limited to surgical interventions and radiotherapy; Therapies with a component administered systemically but that act locally (e.g., photodynamic therapy, radioimmunotherapy and radiosensitizers); Development of methods of drug delivery; Research into the development of localised therapies to prevent recurrence. 5.2 Localised Therapies: Clinical Applications – Clinical testing and application of treatments administered locally that target the organ and/or neighbouring tissues directly, including but not limited to surgical interventions and radiotherapy; Clinical testing and application of therapies with a component administered systemically but that act locally (e.g., photodynamic therapy and radiosensitisers); Phase I, II, or III clinical trials of promising therapies that are administered locally; Side effects, toxicity, and pharmacodynamics; Clinical testing of localised therapies to prevent recurrence. 5.3 Systemic Therapies: Discovery and Development – Discovery and development of treatments administered systemically such as cytotoxic or hormonal agents, novel 9 February 2015 6 Insert applicant last name systemic therapies such as immunologically directed therapies (vaccines, antibodies), gene therapy, angiogenesis inhibitors, apoptosis inhibitors, and differentiating agents; Defining molecular signatures of cancer cells; Identifying molecular targets for drug discovery (includes mechanistic studies of cellular metabolism, combinatorial chemical synthesis, drug screening, development of high-throughput assays, and testing in model systems; Investigating the molecular mechanisms of drug resistance and pre-clinical evaluation of therapies to circumvent resistance; Development of methods of drug delivery; Research into the development of systemic therapies to prevent recurrence. 5.4 Systemic Therapies: Clinical Applications – Clinical testing and application of treatments administered systemically such as cytotoxic or hormonal agents, novel systemic therapies such as immunologically directed therapies (vaccines, antibodies), gene therapy, angiogenesis inhibitors, apoptosis inhibitors, and differentiating agents; Phase I, II or III clinical trials of promising therapies administered systemically; Side effects, toxicity, and pharmacodynamics; Clinical testing of systemic therapies to prevent recurrence. 5.5 Combinations of Localised and Systemic Therapies – Development and testing of combined approaches to treatment; Clinical application of combined approaches to treatment such as systemic cytotoxic therapy and radiation therapy; Development and clinical application of combined localised and systemic therapies to prevent recurrence. 5.6 Complementary and Alternative Treatment Approaches – Discovery, development, and clinical application of complementary/alternative treatment approaches such as diet, herbs, supplements, natural substances, or other interventions that are not widely used in conventional medicine or are being applied in different ways as compared to conventional medical uses; Complementary/alternative approaches to the prevention of recurrence (please note that primary prevention using complementary or alternative approaches should be coded under 3.5). 5.7 Resources and Infrastructure Related to Treatment and the Prevention of Recurrence – Informatics and informatics networks (e.g., clinical trials networks and databanks); Mathematical and computer simulations; Specimen resources (serum, tissue, etc.); Clinical trial groups; Epidemiological resources pertaining to treatment; Statistical methodology or biostatistical methods; Drugs and reagents for distribution and drug screening infrastructures; Centres, consortia, and/or networks; Education and training of investigators at all levels (including clinicians), such as participation in training workshops, advanced research technique courses, and Master’s course attendance (this does not include longer-term research-based training, such as Ph.D. or post-doctoral fellowships). 6. Cancer Control, Survivorship, and Outcomes Research: Research included in this category includes a broad range of areas: patient care and pain management; tracking cancer cases in the population; beliefs and attitudes that affect behaviour regarding cancer control; ethics, education and communication approaches for patients and health care professionals; supportive and end-of-life care; and health care delivery in terms of quality and cost effectiveness. 6.1 Patient Care and Survivorship Issues – Quality of life; Pain management; Psychological impacts of cancer survivorship; Rehabilitation; Reproductive issues; Long-term morbidity; Symptom management, including nausea, vomiting, lymphedema, neuropathies, etc.; Prevention of treatment-related toxicities and sequelae, including symptom management, prevention of mucosities, prevention of cardiotoxicities, etc. 6.2 Surveillance – Epidemiology and end results reporting (e.g., SEER); Surveillance of cancer risk factors such as diet, body weight, physical activity, sun exposure, and tobacco use; Analysis of variations in risk factor exposure by demographic or other factors; Registries that track incidence, morbidity, and/or mortality related to cancer; Trends in use of interventional strategies; Method development for risk factor surveillance. 6.3 Behaviour – Behavioural medicine research and interventions; Influence of social factors such as community, policy, education, and legislation, on behaviours related to cancer control; Attitudes and belief systems and their influence on psychological health and on behaviours related to cancer control (e.g., how beliefs can alter attempts to seek screening, detection, and treatment); Interventions to change attitudes and beliefs that affect behaviour related to cancer control and cancer outcomes; Influences of attitudes and beliefs on compliance with treatment and prevention protocols; Psychological or educational interventions to promote behaviours that lessen treatmentrelated morbidity and promote psychological adjustment to the diagnosis of cancer and to treatment effects; Burdens of cancer on family members/caregivers and psychological/behaviour issues. 6.4 Cost Analyses and Health Care Delivery – Analyses of the cost effectiveness of methods used in cancer prevention, detection, diagnosis, prognosis, treatment, and survivor care/support; Development and testing of health service delivery methods; Interventions to increase the quality of health care delivery; Impact of organisational, social, and cultural factors on access and quality of care; Studies of providers such as geographical or care-setting variations in outcomes; Effect of reimbursement and/or insurance on cancer control, outcomes, and survivorship support; Access to care issues; Health services research, including health policy and practice; Analysis of health service provision, including the interaction of primary and secondary care; cost effectiveness of treatments. 6.5 Education and Communication – Development of communication tools and methods; Education of patients, health care providers, at-risk populations, and the general 9 February 2015 7 Insert applicant last name population about cancer; Communication to patients regarding therapeutic options; Educational interventions to promote self-care and symptom management; Communicating cancer risk to underserved populations, at-risk populations, and the general public; Alternative teaching methods to communication therapeutic options and risk-reduction behaviour to patients and the general public; Communication of lifestyle models that reduce cancer risk, such as communication of nutritional interventions; Communicating smoking and tobacco cessation interventions; Special approaches and considerations for underserved and at-risk populations; Education, information, and prevention/screening/assessment systems for the general public, primary care professionals, or policy makers; Training, predictive cancer models, pain management, and surveillance systems for primary care professionals, telehealth/telemedicine applications; Communication regarding cancer genetics, managed oncology care, and communicating with survivors; Barriers to successful health communication. 6.6 End-of-Life Care – End-of-life care issues, including palliative care, psychological interventions with families at end of life, hospice care, and pain management for terminally ill patients. 6.7 Ethics and Confidentiality in Cancer Research – Informed consent modelling and development; Quality of Institutional Review Boards (IRBs); Protecting patient confidentiality and privacy; Research ethics. 6.8 Complementary and Alternative Approaches for Supportive Care of Patients and Survivors – Hypnotherapy, relaxation, transcendental meditation, imagery, spiritual healing, massage, biofeedback, etc., as used for the supportive care of patients and survivors; Discovery, development, and testing of complementary/alternative approaches such as diet, herbs, supplements, or other interventions that are not widely used in conventional medicine or are being applied in different ways as compared to conventional medical uses. 6.9 Resources and Infrastructure Related to Cancer Control, Survivorship, and Outcomes Research – Informatics and informatics networks; Clinical trial groups related to cancer control, survivorship, and outcomes research; Epidemiological resources pertaining to cancer control, survivorship, and outcomes research; Statistical methodology or biostatistical methods; Surveillance infrastructures; Centres, consortia, and/or networks; Psychological, economic, political and health services research frameworks and models; Education and training of investigators at all levels (including clinicians), such as participation in training workshops, advanced research technique courses, and Master’s course attendance (this does not include longer-term research-based training, such as Ph.D. or post-doctoral fellowships). 7. Scientific Model Systems: Research included in this category looks at the development of new animal models, cell cultures and computer simulations and their application to other studies across the spectrum of cancer research. 7.1 Development and Characterisation of Model Systems – Development and characterisation of model systems, including but not limited to: Computer simulation model systems and computer software development; In vitro models systems; Cell culture model systems; Organ and tissue model systems; Animal model systems such as drosophila and c. elegans, zebra fish, mouse, etc. 7.2 Application of Model Systems – Research into new ways of applying model systems, including but not limited to: Computer simulations model systems and computer software development; In vitro model systems; Cell culture model systems; Organ and tissue model systems; Animal model systems such as drosophila and c. elegans, zebra fish, mouse, etc. 7.3 Resources and Infrastructure Related to Scientific Model Systems – Models made available for distribution to the scientific community; Centres, consortia, and/or networks; Education and training of investigators at all levels (including clinicians), such as participation in training workshops, advanced research technique courses, and Master’s course attendance (this does not include longer-term research-based training, such as Ph.D. or post-doctoral fellowships). 9 February 2015 8 Insert applicant last name BURDEN OF DISEASE – LEVEL 2 Identify (x) the cancer specific Level 2 Burden of Disease that best describes the area of research of the application. You can select up to three Level 2 Burden of Disease types and you must allocate a percentage of time against each. The percentage total must not exceed 100%. Level 1 Level 2 Cancer and other malignant neoplasms Bone and connective tissue cancers Check (x) Brain cancer Breast cancer Childhood cancers (may include some leukaemia/ lymphoma and other cancer types) Colon Endocrine cancers Gastrointestinal cancers Genitourinary cancers Gynaecological cancers Haematological cancers Health system issues related to cancer Leukaemia Lung cancers Lymphomas Melanoma Mental health and psychosocial factors related to cancer Other non-specific Basic Science cancer research Other non-specific Clinical Science cancer research Prostate cancer Public and population health related cancer issues Skin cancers (non-melanoma) Total Per cent 9 February 2015 9 Per cent (%) Insert applicant last name 2016 PROGRAM GRANT Application form: Part B Research Strategy PROGRAM SUMMARY (maximum 1 page) Summarise the aims, hypotheses, research plan and potential significance of the overall program. 9 February 2015 10 Insert applicant last name RESEARCH STRATEGY (maximum 8 pages) Provide detail on the proposed research program. This section should be organised under the following headings: Background: Outline the scientific background to the applications, critically evaluate existing knowledge, and identify the gaps in knowledge that the Program is intended to fill. Objectives: State the scientific objectives that the Program aims to achieve, the hypotheses that will be tested, and the significance of the proposed Program to cancer control. Research design and methods: Address in detail the design and methods to be used for each component of the proposed Program. Make clear how these components will individually and collectively test the hypotheses and achieve the aims of the Program. Specify the data that will be collected and how they will be collected, analysed and interpreted. Describe and justify any new methods to be developed in terms of their advantages relative to existing methods. Identify potential difficulties and limitations of the proposed procedures, and alternative approaches that might be used to achieve the aims. References (in addition to the 8 page maximum for the Research Strategy): A list of all references cited in the Research Strategy must be provided. BUDGET a) Provide a maximum 1 page budget per year of funding requested (maximum 5 pages), itemising the support requested under the headings below. A 1-2 sentence description and/or justification should be provided for each budget line item. The maximum budget that can be requested is $450,000 per annum. Staff: List whatever salary you deem appropriate for grant-supported personnel; you are not restricted to NHMRC’s pre-defined Personnel Support Package salary levels. Amounts requested for grant-supported personnel must cover all salary and salary on-costs (e.g., payroll tax, workers compensation, leave loading, compulsory and contributory superannuation). Provide the proposed level of appointment, the annual fraction of full-time for the appointment, the annual full-time equivalent salary level, and the amount requested. If a staff member is also an investigator, identify him/her by name. CVs must be supplied for all staff for whom funding is requested at the level of Academic Level B or higher. Equipment: Specify individually all items of equipment that cost more than $5000 and attach a written quotation in support. Maintenance and consumable items: Itemise in readily understood terms such as interviews, travel costs, laboratory animals, reagents, etc. b) Support from Institutions: Describe existing resources and infrastructure critical to the proposed Program’s success, with a view to reassuring assessors of the Program’s feasibility. You have an additional maximum of ½ a page to provide this information. 9 February 2015 11 Insert applicant last name 2016 PROGRAM GRANT Application form: Part C Collaborative Gain COHERENCE OF THE RESEARCH TEAM AND PROGRAM (maximum 1 page) Describe the extent to which the proposed Program of research activities works towards a common scientific end or ultimate practical application by, for example, addressing a set of inter-related research questions. RESOURCE MANAGEMENT (maximum 1 page) Describe how the integration of teams and the distribution of resources will be managed, including an outline of previous strategies and new collaborative arrangements. Highly regarded applications will demonstrate that the Administering Institution already has in place the processes by which grant funds and other resources will be shared between research teams, such that delays in the development of such agreements do not lead to unnecessary delays in the conduct of the research. Describe how intellectual exchange will be facilitated between the teams that contribute to the Program. MULTIDISCIPLINARY AND MULTI-INSTITUTIONAL COLLABORATION (maximum 1 page) Describe the extent and quality of proposed multidisciplinary and multi-institutional collaboration and its prospects for adding value to the research proposed. CHIEF INVESTIGATOR(S) ROLE IN THE PROPOSED PROGRAM (maximum ½ page per CI) Outline the role of each Chief Investigator in the proposed Program. Provide justification for why each Chief Investigator is needed, including the specific expertise and experience that each brings to the Program. TRAINING, CAREER DEVELOPMENT AND MENTORING (maximum 2 pages) Describe the track records of the Chief Investigator(s) in the provision of research training, career development and mentoring; and opportunities for these activities to be undertaken within the proposed Program, including the training and mentoring strategies that will be adopted. 9 February 2015 12 Insert applicant last name 2016 PROGRAM GRANT Application form: Part D Research Achievement CURRICULUM VITAE OF CHIEF INVESTIGATOR(S) Chief Investigator 1 1. Brief (maximum 1 page) biography, including career disruption 2. List of publications/high quality technical reports since January 2010, including those under review. Highlight publications especially relevant to this application 3. Research support from all sources for all projects completed since January 2010, currently held or pending funding decisions. Use the following headings and under each, tabulate: funding body, title of grant, chief investigators, time commitment (%) (current and requested applications only), period of support and total funding for the grant period a) Completed since January 2010 b) Support currently held (at time of submission of this application) c) Requested (for next year excluding this submission. For NHMRC Project Grants, please provide NHMRC application number). 4. Invitations/prizes/awards 5. Research application 6. Community Engagement Chief Investigator 2 1. Brief (maximum 1 page) biography, including career disruption. 2. List of publications/high quality technical reports since January 2010, including those under review. Highlight publications especially relevant to this application. 3. Research support from all sources for all projects completed since January 2010, currently held or pending funding decisions. Use the following headings and under each, tabulate: funding body, title of grant, chief investigators, time commitment (%) (current and requested applications only), period of support and total funding for the grant period. a) Completed since January 2010 b) Support currently held (at time of submission of this application) c) Requested (for next year excluding this submission. For NHMRC Project Grants, please provide NHMRC application number). 4. Invitations/prizes/awards 5. Research application 6. Community Engagement Chief Investigator 3 1. Brief (maximum 1 page) biography, including career disruption. 2. List of publications/high quality technical reports since January 2010, including those under review. Highlight publications especially relevant to this application. 3. Research support from all sources for all projects completed since January 2010, currently held or pending funding decisions. Use the following headings and under each, tabulate: funding body, title of grant, chief investigators, time commitment (%) (current and requested applications only), period of support and total funding for the grant period. a) Completed since January 2010 b) Support currently held (at time of submission of this application) c) Requested (for next year excluding this submission. For NHMRC Project Grants, please provide NHMRC application number). 4. Invitations/prizes/awards 5. Research application 6. Community Engagement Please copy above table block and complete details for any additional Chief Investigators 9 February 2015 13 Insert applicant last name 2016 PROGRAM GRANT Application form: Part E Consumer Information CANCER COUNCIL NSW RESEARCH OUTCOMES Identify (x) the ONE of the following four Cancer Council NSW research outcomes to which the proposed Program will ultimately contribute most strongly: Decreased cancer incidence Increased cancer survival rates Improved treatment effectiveness Enhanced quality of life for cancer patients and/or their carers and support networks LAY DESCRIPTION (maximum 1 page) Describe the research proposal in lay terms, including how the proposed Program contributes to the Cancer Council NSW research outcome you selected above. This information will assist the Cancer Council NSW Consumer Review Panel to understand the significance of your work. CONSUMER REVIEW CRITERIA (maximum 2 pages) 1. Extent of benefit: Explain how the results of your research will have an important positive impact on human lives, including any of the following aspects: disease causation, prevention, diagnosis; treatment; physical and/or mental and/or social wellbeing; quality of life, dignity, and survival 2. Pathway for realising the benefit: Provide a clear description of the steps required to reach the stated end benefits of the research 3. Potential for application of findings: Explain how the research will be applied in the real world (over the short, medium or long term), the barriers you need to address to be successful, and how you propose to address them. 4. Equity: Justify the selection of the study sample and explain why you have included and excluded particular groups who could potentially benefit from the outcomes of this research. If relevant, outline how the proposal addresses an under-studied or under-served population and/or a population with a high burden of disease or poorer outcomes. 5. Consumer involvement: Outline how relevant informed consumers (e.g. from consumer or cancer groups such as Cancer Voices NSW, Breast Cancer Action Group NSW, Consumers Health Forum, cancer support groups, organisational in-house research consumer panels, etc) have been involved during the development of the research proposal; and the plan for ongoing consumer involvement in the research. Explain how this/these consumer(s) are ‘qualified’ to be involved. 9 February 2015 14 Insert applicant last name 2016 PROGRAM GRANT Application form: Part F Certification and Assessors CERTIFICATION Certification by Chief Investigator(s) In signing this page, you certify that all details given in this application are correct; and you agree to conduct the Program according to Cancer Council NSW’s 2016 Program Grant Policy and Conditions of Award. Electronic or scanned signatures are acceptable. Chief Investigator Name (please print in block letters) Signature 1 2 3 Certification by Associate Investigator(s) In signing this page you certify, as an Associate Investigator on the Program, to participate in this collaboration. Electronic or scanned signatures are acceptable. Associate Investigator Name (please print in block letters) Signature 1 2 3 Certification by Head of Department I certify that the Program is appropriate to my Department; that my Department can accommodate the Program as proposed; and that I will support the conduct of the Program in my Department. Name (please print in block letters) Department Signature Electronic or scanned signatures are acceptable. Date Certification by Head of Institution (or delegate) I certify that this request satisfies the requirements of this institution, and that this institution has established administrative processes for assuring sound scientific practice in accordance with the Australian Code for the Responsible Conduct of Research. Name (please print in block letters) Title/Position Signature Electronic or scanned signatures are acceptable. Date 9 February 2015 15 Insert applicant last name This page will be removed prior to forwarding to assessors for review. Please ensure that all attachments are inserted prior to this page and that the reverse of this page remains blank. NOMINATION OF ASSESSOR FOR THIS APPLICATION Nominate at least three assessors who are suitable for peer review of this application. At least one international assessor At least one assessor in Australia outside NSW State any beneficial relationship that exists between the applicant and the nominated assessors Nominated Assessor 1 Name Position Department, Institution Address City/Suburb, State, Postcode Country Phone Email State any beneficial relationship that exists between the nominee and the applicant Nominated Assessor 2 Name Position Department, Institution Address City/Suburb, State, Postcode Country Phone Email State any beneficial relationship that exists between the nominee and the applicant Nominated Assessor 3 Name Position Department, Institution Address City/Suburb, State, Postcode Country Phone Email State any beneficial relationship that exists between the nominee and the applicant 9 February 2015 16 Insert applicant last name Please copy above table block and complete details for any additional nominated assessors Declaration of assessor agreement I have contacted all of the above nominated assessors; and all have agreed to review this application if selected by the Cancer Council NSW Program Grant Selection Committee. Signature Electronic or scanned signatures are acceptable Date: Consent to provide information to International assessors I consent to Cancer Council NSW sending my personal information overseas, for the purpose of the peer review of applications. Signature Electronic or scanned signatures are acceptable 9 February 2015 Date: 17 Insert applicant last name INAPPROPRIATE ASSESSOR(S) Nominate any assessors who are not suitable to peer review this application. Please include reasons e.g. conflict of interest, close association, etc. Inappropriate Assessor 1 Name Position Department, Institution Address City/Suburb, State, Postcode Country Phone Email Reason Inappropriate Assessor 2 Name Position Department, Institution Address City/Suburb, State, Postcode Country Phone Email Reason Inappropriate Assessor 3 Name Position Department, Institution Address City/Suburb, State, Postcode Country Phone Email Reason Please copy above table block and complete details for any additional inappropriate assessors 9 February 2015 18