Appendix Members of SAFE-PCI for Women Trial committees
advertisement
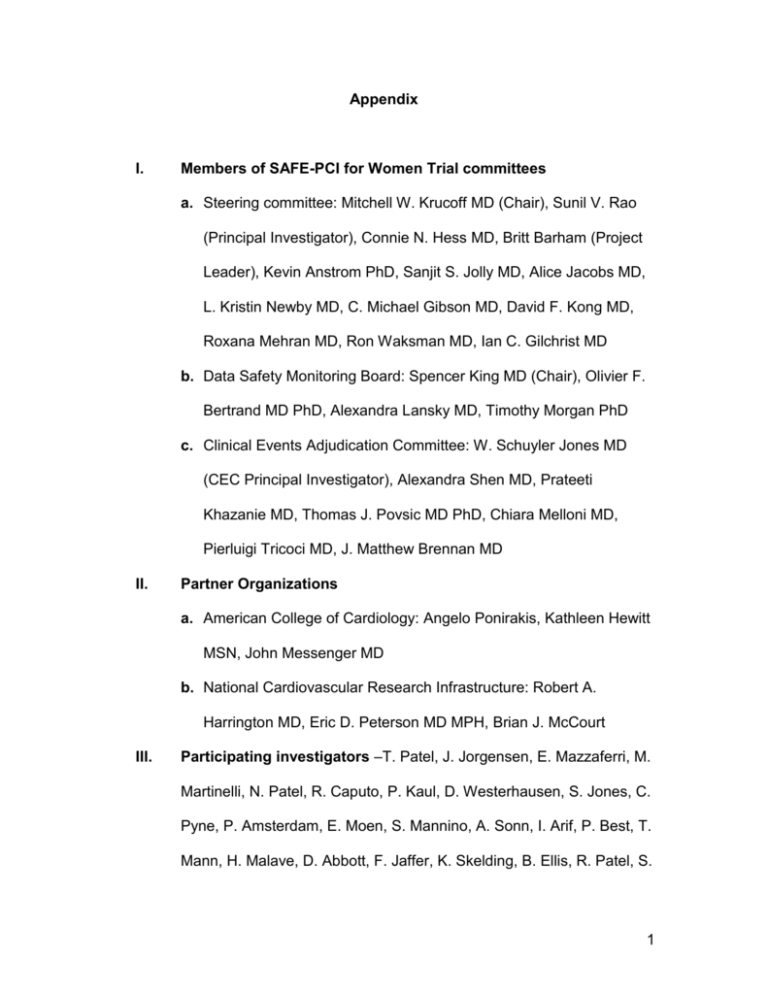
Appendix I. Members of SAFE-PCI for Women Trial committees a. Steering committee: Mitchell W. Krucoff MD (Chair), Sunil V. Rao (Principal Investigator), Connie N. Hess MD, Britt Barham (Project Leader), Kevin Anstrom PhD, Sanjit S. Jolly MD, Alice Jacobs MD, L. Kristin Newby MD, C. Michael Gibson MD, David F. Kong MD, Roxana Mehran MD, Ron Waksman MD, Ian C. Gilchrist MD b. Data Safety Monitoring Board: Spencer King MD (Chair), Olivier F. Bertrand MD PhD, Alexandra Lansky MD, Timothy Morgan PhD c. Clinical Events Adjudication Committee: W. Schuyler Jones MD (CEC Principal Investigator), Alexandra Shen MD, Prateeti Khazanie MD, Thomas J. Povsic MD PhD, Chiara Melloni MD, Pierluigi Tricoci MD, J. Matthew Brennan MD II. Partner Organizations a. American College of Cardiology: Angelo Ponirakis, Kathleen Hewitt MSN, John Messenger MD b. National Cardiovascular Research Infrastructure: Robert A. Harrington MD, Eric D. Peterson MD MPH, Brian J. McCourt III. Participating investigators –T. Patel, J. Jorgensen, E. Mazzaferri, M. Martinelli, N. Patel, R. Caputo, P. Kaul, D. Westerhausen, S. Jones, C. Pyne, P. Amsterdam, E. Moen, S. Mannino, A. Sonn, I. Arif, P. Best, T. Mann, H. Malave, D. Abbott, F. Jaffer, K. Skelding, B. Ellis, R. Patel, S. 1 Yakubov, D. Steinbgerg, L. Gruberg, J. Aji, N. Mejevoi, B. Stein, S. Gandhi, N. El-Gharib/H. Dauerman, M. Vidovich, K.Tummalapalli, R. Quesada, P. Patel, R. Yaryura, J. Tremmel, S. Guidera, G. Revtyak, G. Ramaswamy, M. Ahmed, R. Nelson, M. East, G. Nseir, C. Barker/H.V. Anderson, K. Gibbs, V. Iyer, J. Pap, D. Allen, D. Lewis, S. Maraboyina, S. Martin, I. Gilchrist, M. White, P. Mason, C. Panetta, R. Shetty, D. Sporn, D. Linert, J. Safirstein, R. Mazhari, C. Maniu IV. Definitions of the primary and secondary endpoints a. Primary efficacy endpoint - Bleeding Academic Research Consortium (BARC) Types 2, 3, or 5 bleeding or Vascular complications requiring intervention 2 Type 2 - Any overt, actionable sign of hemorrhage (e.g., more bleeding than would be expected for a clinical circumstance; including bleeding found by imaging alone) that does not fit the criteria for Types 3, 4, or 5, but does meet at least one of the following criteria: 1) Requiring nonsurgical, medical intervention by a health care professional 2) Leading to hospitalization or increased level of care 3) Prompting evaluation ii. Type 3 1. Type 3a - Overt bleeding plus hemoglobin drop of 3 to <5 g/dL (corrected for transfusion) provided hemoglobin drop is related to bleed; Any transfusion with overt bleeding 2. Type 3b - Overt bleeding plus hemoglobin drop ≥ 5 g/dL (corrected for transfusion) provided hemoglobin drop is related to bleed; Cardiac tamponade; Bleeding requiring surgical intervention for control (excluding dental/nasal/skin/hemorrhoid); Bleeding requiring intravenous vasoactive agents 3. Type 3c - Intracranial hemorrhage (does not include microbleeds or hemorrhagic transformation; does include intraspinal) confirmed by autopsy or imaging or LP; Intra-ocular bleed compromising vision iii. Type 5 - Fatal Bleeding 1. Type 5a - Probable fatal bleeding: no autopsy or imaging confirmation, but clinically suspicious 2. Type 5b - Definite fatal bleeding: overt bleeding or autopsy or imaging confirmation. iv. Vascular complications defined as a composite of arteriovenous fistula, or arterial pseudoaneurysm, or arterial occlusion requiring intervention Definitions of TIMI Major, TIMI Minor, ACUITY Major, and CathPCI bleeding a. TIMI major bleeding - Hemoglobin drop > 5 g/dL (with an identified site of bleeding, not associated with CABG) or Intracranial hemorrhage or cardiac tamponade. b. Modified TIMI minor bleeding - Hemoglobin drop > 3 g/dL but <= 5 g/dL, with a known site (not associated with CABG) or Spontaneous gross hematuria. i. V. 3 VI. c. Modified ACUITY bleeding - At least one of the following not associated with CABG: Intracranial bleeding, retroperitoneal bleeding, intraocular bleeding, access site hemorrhage requiring surgical intervention, > 5 cm diameter hematoma at puncture site, reduction in hemoglobin concentration of > 4 g/dL without an overt source of bleeding, reduction in hemoglobin concentration of > 3 g/dL with an overt source of bleeding, re-operation for bleeding or use of any blood product transfusion d. Modified CATHPCI bleeding definition - Bleed is not associated with CABG and at least one of the following: 1. Hemoglobin drop of >=3 g/dL 2. Transfusion of whole blood or packed red blood cells 3. Procedural intervention/surgery at the bleeding site to reverse/stop or correct the bleeding (such as surgical closures/exploration of the arteriotomy site, balloon angioplasty to seal an arterial tear, endoscopy with cautery of a GI bleed). Reasons for access site conversion (access site crossover) a. Total randomized cohort i. Conversion from radial access to femoral access other than arterial spasm 1. Unable to gain arterial access (14 patients) 2. Arterial tortuosity limiting engagement of coronary ostia (6 patients) 3. Poor catheter support (2 patients) 4. Referring physician requested bi-plane procedure after pt was randomized, case was done femorally 5. Radial arterial loop, unable to advance the catheter 6. Allen and Barbeau test abnormal in cath lab. 7. Had both spasm in left radial and poor guide support in right radial 8. Hx of lumpectomy & axillary node dissection on right in the past ii. Conversion from femoral to radial access 1. Femoral pulse too weak 2. Significant candida infection in groin 3. Unable to complete procedure 4. High grade stenosis (2 patients) b. PCI cohort (subset of the total randomized cohort) i. Conversion from radial to femoral access for reasons other than arterial spasm 4 VII. 1. Unable to gain arterial access (15 patients) 2. Arterial tortuosity limiting engagement of coronary ostia (2 patients) 3. Poor guide catheter support 4. Referring physician requested bi-plane procedure after pt was randomized, case was done femorally 5. Radial arterial loop, unable to advance the catheter 6. Allen and Barbeau test abnormal in cath lab. 7. Had both spasm in left radial and poor guide support in right radial 8. Hx of lumpectomy & axillary node dissection on right in the past ii. Conversion from femoral to radial access 1. High grade stenosis 2. Weak pulse 3. Significant candida infection in groin Primary efficacy endpoint results by actual treatment received a. Total randomized cohort i. Radial 0.6% vs. Femoral 1.6%, OR 0.36 (0.13-1.99), P=0.05 b. PCI cohort i. Radial 0.9% vs. Femoral 3.1%, OR 0.29 (0.08-1.06), P=0.06 5