c: detailed output scoring - Department for International Development
advertisement
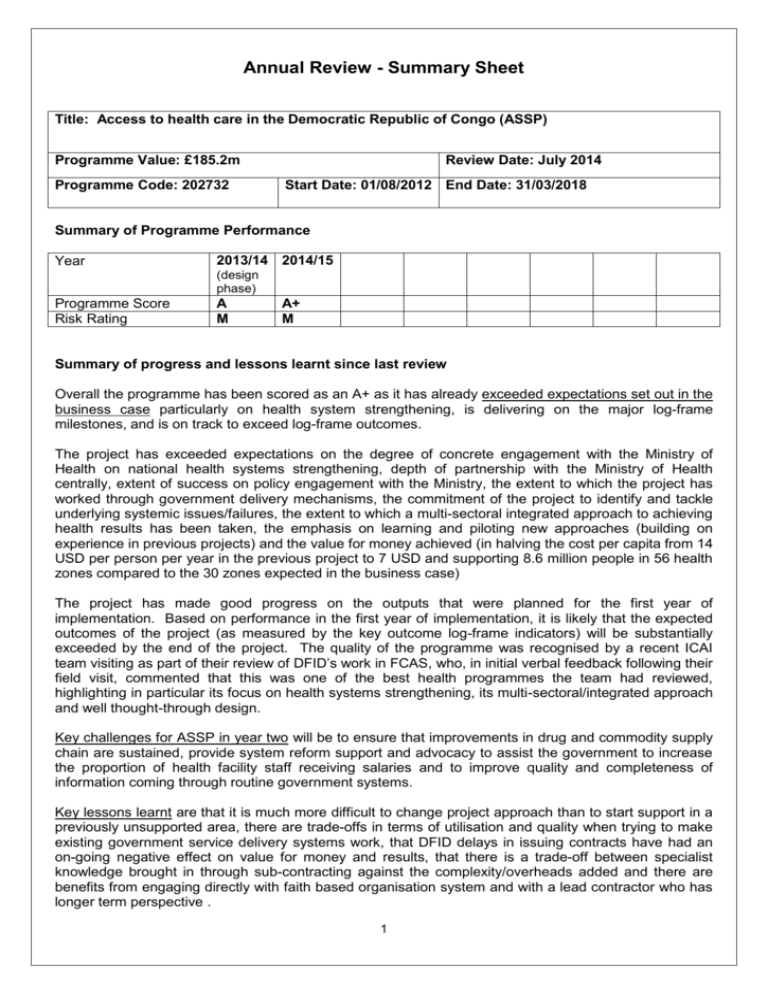
Annual Review - Summary Sheet Title: Access to health care in the Democratic Republic of Congo (ASSP) Programme Value: £185.2m Programme Code: 202732 Review Date: July 2014 Start Date: 01/08/2012 End Date: 31/03/2018 Summary of Programme Performance Year 2013/14 2014/15 (design phase) Programme Score Risk Rating A M A+ M Summary of progress and lessons learnt since last review Overall the programme has been scored as an A+ as it has already exceeded expectations set out in the business case particularly on health system strengthening, is delivering on the major log-frame milestones, and is on track to exceed log-frame outcomes. The project has exceeded expectations on the degree of concrete engagement with the Ministry of Health on national health systems strengthening, depth of partnership with the Ministry of Health centrally, extent of success on policy engagement with the Ministry, the extent to which the project has worked through government delivery mechanisms, the commitment of the project to identify and tackle underlying systemic issues/failures, the extent to which a multi-sectoral integrated approach to achieving health results has been taken, the emphasis on learning and piloting new approaches (building on experience in previous projects) and the value for money achieved (in halving the cost per capita from 14 USD per person per year in the previous project to 7 USD and supporting 8.6 million people in 56 health zones compared to the 30 zones expected in the business case) The project has made good progress on the outputs that were planned for the first year of implementation. Based on performance in the first year of implementation, it is likely that the expected outcomes of the project (as measured by the key outcome log-frame indicators) will be substantially exceeded by the end of the project. The quality of the programme was recognised by a recent ICAI team visiting as part of their review of DFID’s work in FCAS, who, in initial verbal feedback following their field visit, commented that this was one of the best health programmes the team had reviewed, highlighting in particular its focus on health systems strengthening, its multi-sectoral/integrated approach and well thought-through design. Key challenges for ASSP in year two will be to ensure that improvements in drug and commodity supply chain are sustained, provide system reform support and advocacy to assist the government to increase the proportion of health facility staff receiving salaries and to improve quality and completeness of information coming through routine government systems. Key lessons learnt are that it is much more difficult to change project approach than to start support in a previously unsupported area, there are trade-offs in terms of utilisation and quality when trying to make existing government service delivery systems work, that DFID delays in issuing contracts have had an on-going negative effect on value for money and results, that there is a trade-off between specialist knowledge brought in through sub-contracting against the complexity/overheads added and there are benefits from engaging directly with faith based organisation system and with a lead contractor who has longer term perspective . 1 Summary of recommendations for the next year IMA should by the end of year two: i. Update the action plan on pharmaceuticals supply chain. Going forward, the action plan should include both an operational and a strategic plan including starting some procurement through FEDECAM (the national drug procurement agency). ii. Develop a plan on how health zones will be transitioned through different phases of support within the project (e.g. investment, development, and maintenance phases). iii. Build on year one’s successes in policy engagement with the Ministry of Health on faith based providers to strengthen coordination of corels (faith based organisations) and facilitate further discussions on the relationship between faith based providers and government. iv. Improve asset management systems within IMA and used by implementing partners (IPs) and ensure that IPs have adequate security arrangements and communications equipment in place. DFID should by the end of year two: i. Strengthen horizontal links between DFID programmes within geographical areas e.g. links between the SGBV (Sexual and Gender Based Violence) work within DFID’s SSAPR police programme and ASSP. (Responsible: DFID Health Programme Officer) ii. Continue to engage on donor coordination/harmonisation of support within Directions Provinciales de Santé and explore other new co-funding opportunities for ASSP going forward. (DFID Programme Coordinator) iii. Contract some third party monitoring using health programme funds if a cross-office contract has not been tendered by the end of 2014. (DFID Programme Officer) iv. Put in place longer term advisory expertise to oversee construction (either through 10% cadre input or as cross office- consultancy). (Programme Coordinator) v. DFID DRC should explore the feasibility of cross-office support for IMA to further develop their existing conflict analysis and resilience planning (for example through the EACP contract). (Lead Adviser) vi. Ensure that more of the health systems strengthening work that has been successfully taken on by ASSP and which extends their terms of reference is now funded as a cost extension [to IMA’s contract] within the existing envelope of the Business Case (now that the anticipated RCI institutional strengthening project will not be contracted as a stand-alone contract). 2 A. Introduction and Context DevTracker Link to Business Case: DevTracker Link to Log frame: http://devtracker.dfid.gov.uk/projects/GB-1-202732/documents/ http://devtracker.dfid.gov.uk/projects/GB-1-202732/documents/ Outline of the programme Following an allocation of £300,000 for design work, the UK is providing £184.9 GBP million over five years to strengthen basic health service provision in the Democratic Republic of Congo (DRC) in order to improve reproductive, maternal, neonatal and child health (£179.7m), and to strengthen the capacity of the central Ministry of Health to support service delivery (£5.2m). The figure below outlines the key results expected from this programme as outlined in the business case together with progress to date. Figure 1: Results expected from the programme (as outlined in the business case). Expected results Reduce U5 mortality by 50% in target areas: Vaccinate 64,600 one year olds against measles each year. Provide contraception - 155,000 CYPs (couple years protection) cumulatively by 2014/15 and 355,000 CYPs by the end of the five year programme. Ensure that 75,000 births per year are attended by skilled health personnel. Make sure 100% of health facilities in target areas offer appropriate emergency obstetric care. Provide 75,000 pregnant women with Intermittent Presumptive Treatment (IPT) for malaria during ante-natal visits. Provide 600,000 people with access to clean water and sanitation. Progress after year one of implementation Results awaiting end-point household survey. 232,781 in year one Comment 65,473 in year one Expected to exceed target in year two as commodities were not in place until the middle of year one following DFID’s delay issuing the implementation contract. 213,716 Exceeded expectations Exceeded expectations Data awaited from health facility survey 138, 698 in year one Exceeded expectations Not planned for year one Final target has been revised to 374,400 as cost estimates in business case were based on Village Assaini phase I planning estimates which UNICEF found to be significantly underestimated subsequent to the business case. The Access to Healthcare business case funds have been contracted as follows; a) £179.7m for the ASSP (Accès aux soins de santé primaires) project – this was awarded to IMA World Health following an OJEU international competitive tender. SIDA additionally co-fund this project, so the total value of the contract is now £182,899,146. b) £1.3m for the DRC Demographic and Health Survey through a memorandum of understanding with UNICEF (from February 2013 to March 2015). c) £0.4m for Public Financial Management support. This has been contracted through OPM (under DFID’s HEART PEAKS framework agreement) and provides embedded technical assistance in the Ministry of Health. The 6 month initial support ends in August 2014 and we are now seeking to extend support to the Ministry for a further 12 months. 3 d) Funds which are currently un-contracted (originally allocated for the RCI institutional strengthening project in the business case): £3.4m. Prior to the RAR budget review in July 2014 we had planned to contract £2.8m of these for additional systems strengthening work in ASSP. This is now under review pending clarification of the 2015/16 and outer years allocations. The ASSP project is implemented by IMA World Health with a consortium of NGOs and supports 56 health zones (out of 515 nationally) in five of the eleven provinces in DRC, providing an estimated 8.6 million people with access to essential primary and secondary healthcare services. The design phase began in October 2012 with implementation planned to run for five years from April 2013 to March 2018. ASSP builds on DFID’s proven track record of improving access to health care and delivering health results in the DRC as a result of its previous Access to Healthcare programme (A2H2), which ended in March 2013. It differs by covering a significantly larger area (increasing coverage from 20 to 56 health zones), by supporting government delivery systems rather than operating in parallel, focusing more on health systems strengthening and adopting a more sustainable approach (by removing the direct payment of project incentives to front-line health facility staff and shifting to subsidised user fees with some exemptions rather than free health care). IMA subcontract four NGOs (SANRU, World Vision, IRC and Caritas) as Implementing Partners (IPs) to support the Ministry of Health deliver services through a mixture of government, faith-based and, in some areas, private health facilities and build the capacity of the Ministry at provincial, district and health zone levels. The consortium also includes Pathfinder International who provides technical assistance for family planning and reproductive health across the project and Tulane University who lead a £4m Operations Research and Impact Evaluation (ORIE) component. In addition to supporting service delivery, the project has developed a strong focus on governance and health system strengthening as a result of better engagement on both the part of the Ministry and consortium lead than was predicted during business case design; At community level, ASSP aims to increase awareness on expectations of levels of service, pilot community score cards, build the capacity of CODESAs (Community Health committees) and is piloting a “Health Village” scheme which motivates communities to achieve health outcomes on a range of key targets e.g. on vaccination, malaria control, family planning and WASH (through Village Ecole Assaini). ASSP is piloting a hybrid cash/agricultural Community Health Endowment scheme to improve local revenue collection and pool risk/subsidise user-fees. The project has an integrated approach, containing a large WASH (Water, Sanitation and Hygiene) component based on Village Assaini plus additional activities on water quality/cisterns and a nutrition package including both prevention work (home gardening and education) and treatment of malnutrition. At health facility level, ASSP has a large construction programme (including 200 new health centres, two hospitals and over 300 rehabilitations) and provides facilities with essential equipment, drugs/supplies, training and an operational allowance. ASSP is also supporting the piloting of a national MoH system of financial management for HGR (general hospitals). At Health Zone management team level, ASSP is strengthening government capacity to manage health zones through capacity building Equipes Cadres de Zones de Santé to improve supervision of health facilities and use planning tools for the development of the health zone and supporting Conseils d’Administration de Zones de Santé. At Provincial/District level, ASSP is supporting the setting up of the new DPS (Directions Provinciales de Santé) management teams and supports MIPs (Medeçins Inspecteurs de Province), Comités Provinciaux de Pilotage), and is improving capacity and minor rehabilitation of CDRs (regional drug depots). ASSP intends to start procurement through FEDECAM next year (the national drug procurement agency). At central level, work on the set-up and roll out of the new national health management information system HMIS (based on the DHIS2 platform) and HR information system pilot (I-HRIS) are key building 4 blocks of improvements to management. The HR work is an entry point to negotiating norms and standards of staffing levels and also potentially rationalisation and cleaning of the pay-roll. ASSP is facilitating policy dialogue between faith-based providers and the Ministry of Health following negotiation of a new MoU which outlines government commitment on salary provision, tax exemptions etc for faith based providers. Faith based providers (mostly the Catholic and Protestant churches) provide over 40% of care in DRC. 5 B: PERFORMANCE AND CONCLUSIONS This annual review covers the first year of project implementation from April 2013 to March 2014. Support to new health zones did not start until quarter two in year one (pending DFID issuing the full implementation contract). This review was conducted in June/July 2014. Indicator data in the report is given until the end of March 2014 and is collected from quarterly narrative reports. The annual review process consisted of the following components; - Half day workshop between DFID DRC (including cross cutting advisers) and IMA - Two day partners workshop chaired by central MoH including SIDA, IPs, MoH provincial/district medicin chefs and technical partners (including feedback session with implementing partners in absence of IMA). - WASH meeting with IMA and DFID WASH adviser - ORIE oversight committee meeting with DFID and Tulane University - Field visit to three health zones (Ilebo, Mweka and Katende) in Kasai Occidental (See reports Quest numbers 4568786 and 4565653) - Review of year one quarter four financial and narrative reports - Feedback meeting with IMA and planned feedback to DFID DRC in programme board meeting. Annual outcome assessment The outcome for this programme is “increased coverage with essential reproductive, maternal and child health services in DFID-supported health zones” and as measured by the following indicators: Outcome indicator(s) Milestone (March 2014) 17/18 target only Progress (March 2014) Survey planned at end of project Number of births attended by skilled health personnel Number of 1 year old children vaccinated against measles Number of sexual and gender-based violence (SGBV) survivors who have received PEP Kits within 72 hours 218,691 213,716 230,475 232,781 385 236 Number of pregnant women who receive two doses of intermittent presumptive treatment for malaria (IPTp) Number of long-lasting insecticide-treated bed nets (LLINs) routinely distributed to pregnant women and children under one year old (18 HZs) Number of children under five and pregnant women reached through DFID’s nutrition-relevant programmes 137,948 138,698 58,092 33,362 Not applicable year one Not applicable year one 59,625 65,473 Contraceptive Prevalence Rate Number of Couple Years Protection 6 Comment Couple Years Protection target (see below) is already exceeding expectations and is proxy indicator for contraceptive prevalence rate Meets expectations (98% of target). Exceeds expectations Lack of PEP kits in initial quarters were the result of delay DFID issuing the implementation contract required for procurement. These are now in place and training completed and on track for year two. Treatment of fistulae is also in the project. Exceeds expectations Routine distribution suspended by MoH in Maniema during mass distribution. This component was added as cost neutral budget amendment in year one as nutrition was not originally planned within ASSP Exceeds expectations Based on performance in the first year of the project it is likely that the expected outcomes of the project measured by the outcome indicators above will be exceeded by the end of the project. Overall output score and description The project has made good progress on the outputs that were planned for year one (as outlined in section C). Overall, the programme has been scored as an A+ as it has exceeded expectations set out in the business case in the following ways: 1. The degree of concrete engagement on national health systems strengthening. The ASSP project was predominantly set up to support service delivery in a sustainable way. Some institutional capacity building (predominantly though technical assistance to the Ministry of Health centrally) was expected to be contracted separately (through the RCI project). ICAI reviewed the project in June 2014 and in initial verbal feedback following their field visit, commented that this was one of the best health programmes the team had reviewed, highlighting in particular its focus on health systems strengthening, its multi-sectoral/integrated approach and well thought-through design. Examples of valuable health systems strengthening (HSS) work that were not originally anticipated in the ASSP design include the set-up and roll-out of the new national Health Management Information System (HMIS) using the DHIS-2 platform and the work on Human Resources for Health, including supporting the MoH to review staffing norms and standards nationally, and then at provincial level reviewing staffing/payroll lists in a validation exercise and setting up an HR Information System to better manage staff/trainings and certification records. 2. Depth of partnership with the Ministry of Health centrally. Previous DFID health projects, whilst liaising with the MoH centrally, in general did not manage to engage with the Ministry centrally to a significant level. In contrast, most components of ASSP are developed with the Ministry - i.e. the project assists the Ministry to review its national policy/guidance - and then the project assists the MoH in rolling this out across ASSP health zones. Examples of this include ASSP’s approach to reviewing MoH family planning/reproductive health fiches techniques, reviewing CODESA (health committee) guidance and the way in which ASSP construction designs for health facilities have been adopted by the Ministry as template national plans. 3. Extent of success on policy engagement. IMA has used the credibility of ASSP’s large scale support to government service delivery systems on the ground, and its long-standing relationship with the Ministry, to good effect in leveraging policy discussions. Most notably IMA managed to facilitate discussions between faith based providers and the Ministry of Health which led to the negotiation of a new Memorandum of Understanding between the major faith based institutions and the Government (which outlines commitments in terms of salaries, tax exemptions etc). This is a major step forward in policy engagement in terms of a future model of provision in terms of the relationship between state and providers. This is strategically important as it could eventually lead to more formalised commissioning of services by the state in the future. 4. The extent to which the project has worked through government delivery mechanisms. This means for example that the project ensures that all trainings are delivered by the Ministry and drugs are distributed through government supply chains. (DFID does not pass funds directly through the Ministry of Health centrally). DFID’s previous projects tended to provide some support in parallel (as this is often faster and ensures quality in the short term) rather than using and attempting to improve government systems. A good example of this is the approach used in the project to distribute drugs through CDRs (MoH regional drug depots) rather than an NGO-led push system. It continues to be an uphill struggle to make this pull system work, but ASSP has additionally invested resources in upgrading and capacity building CDRs: this which was not specified in the terms of reference, but has significant long term value. 5. The commitment of the project to identify and tackle underlying systemic issues/failures. IMA continues to seize opportunities to harness ASSP resources to address underlying health system inadequacies/failures. For example, responding to continued concern over government hospital 7 management issues, IMA has developed, together with the Ministry of Health, an IT system for hospital management (which integrates the financial, pharmaceutical and HMIS data systems) which the MoH will roll out nationally if the ASSP pilot is successful. Another example is the way in which ASSP seeks to mitigate/provide a local solution where the MoH is unable to pay staff salaries regularly by piloting community health endowments. These essentially work as agricultural cooperatives, the income from which enables health facilities to generate primes (incentives) for staff and also subsidise user fees for families in the scheme i.e. acting as a form of mutuelle/health insurance scheme. 6. The extent to which a multi-sectoral integrated approach to achieving health results has been taken. Whilst funds for WASH activities were expected in the project, nutrition activities were not (beyond general health promotion). IMA identified in year one that DFID would not reach its result targets if nutrition was not addressed as it has such a major impact on child morbidity and mortality. ASSP used a cost-neutral budget amendment to incorporate a significant component on nutrition (with a focus on behaviour change including home based gardening). This is anticipated to reach 1.1 million children under five and pregnant women by the end of the project. ASSP has also identified that household air-pollution from cooking is amongst the top three preventable risks for reducing child mortality and plans to pilot the use of clean cook-stoves after year one. 7. The emphasis on learning and piloting new approaches (building on experience in previous projects). DFID has benefited from IMA’s previous experience delivering projects for other donors, and this has been built on in the design of ASSP interventions. A good example of this is IMA’s previous experience in WASH combined with their findings during the needs assessment which indicated that water quality remains an issue (even with capped springs) which has led to a “hybrid approach” to Village Assaini being piloted. Similarly, findings from initial assessments on nutrition in ASSP revealed that embarking on standard CMAM approaches using Ready to Use Therapeutic Food (RUTF) where commodity supply chains could not be ensured after donor funding ends may do harm in the long run as clinic staff turn away children (as they don’t have supplies) rather than offering basic nutrition advice and follow-up. This has informed the nutrition package now being rolled out in ASSP which includes, at health centre level, behaviour change and home based treatment with high energy porridge. Operations research projects have been set up to evaluate early results from both these approaches, which are novel in DRC. 8. Value for money achieved in terms of population served and cost per capita. Compared to expectations as set out in the business case ASSP has significantly exceeded expectations on cost per capita and population reached. In comparison to the old Access to Healthcare programme, ASSP was a scale up in terms of funding of 83% for service delivery, but ASSP has delivered an increase of 247% increase in population reached. The business case anticipated that these funds would support around 30 zones but ASSP has supported 56 in its first year. The cost per capita for support to basic service delivery has halved, from $14 per capita per annum in the previous project to $7. These economies were achieved by changing the model of service delivery (working more through government delivery systems rather than in parallel). Our estimation is that whilst this change in model has resulted in some initial reduction in utilisation rates in previous DFID project zones, if the project achieves its final target rate of 0.6 consultations per capita per year, the overall result will be an increase of 73,180 people using healthcare per £1m invested by DFID. Key challenges for ASSP moving forward In year two of implementation, the key challenges for ASSP will be to; a. Ensure that improvements in drug and commodity supply chain are sustained. IMA should ensure that the drug and commodity stock-out issues experienced earlier this year continue to be addressed pro-actively. Drugs are crucial in ensuring good utilisation rates and stock-outs place an additional burden on patients (as they have to pay for drugs externally in addition to clinic 8 user-fees during stock-outs). The initial procurements were delayed waiting for DFID to issue the full implementation contract. Although IMA then made prompt procurements and accelerated transportation, it took some time before stocks reached the CDRs (government regional drug depots). The project uses government distribution systems based on a pull system where facilities make requests against credit lines. Both DFID and IMA under-estimated the length of time and difficulty involved in switching from a push to a pull system. In April 2014 DFID asked IMA to produce an action plan to improve the drug supply chain in ASSP health zones. This was completed during a joint workshop between ASSP partners and the MoH. This plan now needs updating to track progress made and assign clear responsibilities and timeframes for further actions. Family planning commodity issues in particular need to be prioritised and it is important that ASSP works to improve monitoring of stock-outs and visibility over the ability of facilities to draw down on their credit lines. IMA should also ensure some contingency stocks e.g. of anti-malarials which rely on other projects such as PMI. At the request of the MoH, IMA plan to move around 25% of procurement through the national procurement agency FEDECAM in year two. This could exacerbate stock issues in the short term, but is likely to pay long term dividends in building capacity of FEDACAM. b. Provide system reform support and advocacy to assist the government to increase the proportion of health facility staff receiving salaries. No single government line ministry has control over this, so this will be extremely challenging and ASSP has only limited influence (predominantly through improving information to allow the government to prioritise who is paid and how). c. Improve quality and completeness of information coming through routine government systems. Currently the preliminary results from the large baseline household survey are awaited and the roll out of the new HMIS system is in its very early stages, so the project is lacking key information. Once information does start coming through routine systems it will take many years to improve the quality and completeness of data coming through and this will be a particular issue in DRC where routine data flows and connectivity have been effectively non-existent. In the longer term, it will be important that construction/rehabilitation work goes ahead on schedule as infrastructure impacts on utilisation and hence results. It will also be important that support for revenue generation in health zones started in ASSP (for example through user fees and community health endowments) are translated into a financing model that can be sustained by government in the longer term together with autonomous internal system management capability which can be sustained after support is withdrawn. Key lessons learnt It has been more difficult to operate in health zones previously supported by DFID than the new ones. New health zones (some with no comprehensive donor support for decades, if ever) have shown dramatic improvements in utilisation rates and other key health indicators after just nine months of implementation. The 20 zones supported under DFID’s previous A2H2 project have had a major adjustment in terms of the new policies on the phased withdrawal of primes for health facility staff, the move from an NGO-led push to a government-run pull system for drugs and the introduction of subsidised user fees. DFID and IMA had predicted that utilisation rates would fall as a result. Utilisation rates have now plateaued and IMA expect them to start recovering in year two. In the long run, DFID’s calculations on VfM show that even if final utilisation rates in these zones are lower than under A2H2, that more people will use services per £1m invested under the new project. This is outlined in more detail in section D on VFM. More broadly, the challenges faced in the “old” health zones may indicate that some degree of dependence was caused by the previous projects and highlights the need to consider long term sustainability of projects. There were some key lessons learnt on the logistics of the transition process from the previous Access to Health 2 project to ASSP. These have been documented in a document accompanying the Year One Annual Review - see quest number 4556726. These relate in particular to management of assets and drugs. 9 There are trade-offs in terms of utilisation and quality when trying to make existing government service delivery systems work. It is easier and faster to deliver higher utilisation rates and improve short-term quality of services using parallel systems: this makes them very attractive for those concerned with demonstrating short term outputs. It will take some years of the new approach before ASSP starts delivering services with similarly high utilisation rates/service quality to the previous projects: but the reward for the change is the exponential increase in coverage. DFID underestimated the time taken for the switch from a push to a pull system in the health zones supported under the previous project and the complexity/challenge of making the existing government drug distribution system improve. DFID delays in issuing contracts have had an on-going negative effect on value for money and results. There was a delay in issuing the full implementation contract for ASSP. This has had knock on effects throughout year one with the delays in procuring pharmaceuticals and commodities impacting on utilisation rates. A key lesson is that contract delays impact on results and hence value for money: therefore DFID country offices are right to expect high levels of service on procurement centrally, and to be open where this has not been received. Designing the log-frame prior to tender may be too early to be optimally effective. It would have been better to agree log-frame outputs after the project was contracted and not during the business case prior to tender1. ASSP has exceeded expectations on major health systems strengthening and community level interventions and it has been difficult to compress the various components of the project into the pre-tender log-frame. With hindsight, WHO’s six pillars of a health system would have been a more effective framework to monitor the project, as it has developed a major health systems character, in addition to delivering on basic service delivery and health outcomes. There is a trade-off between specialist knowledge brought in through sub-contracting against the complexity/overheads added. The technical sub-contracts may not have been the most effective way of contracting the research and family planning components. See detailed discussion in section F on performance of partnerships. In summary, it may have been more appropriate for DFID to contract the research component directly and for the consortium lead to have scaled up in-house capacity on family planning rather than contract it to another organisation. As an example of potential to develop in-house capacity, the Community Empowerment and Accountability component originally planned as a subcontract to another INGO was taken over by IMA following performance issues in the design phase. Whilst it has taken some time for IMA to do the inception work on this, there are now promising signs that this component will produce some valuable work, and has generated much interest from the Secretary General in the Ministry of Health. There are benefits from engaging directly with faith based organisation system and with a lead contractor who has longer term perspective. It has been apparent that IMA’s primary long term objective is to build DRC’s health system rather than having an internal focus on organisational growth/objectives. They have used ASSP as an opportunity to address systems issues which will be a barrier to the country moving forward. Assumptions which have not held. A number of assumptions have not held in respect of this business case, mainly related to the anticipated budget in outer years of the project; a. It was assumed that DFID would contract a separate health systems strengthening project (described as the RCI project in the business case). In October/November 2014 a decision was taken that, given the good progress made on HSS and opportunities that were presenting within ASSP, it would be more cost effective for DFID to invest those funds (around £2.8m GBP) in ASSP to expand the integrated HSS work in the project (mainly on HRH, HMIS and support to the MoH centrally). IMA has embarked on HRH and HMIS work in anticipation of this contract 1 The changes in the DFID SMART rules which give greater flexibility in the timeframe for finalising log-frames support this finding 10 extension. To date it is unclear whether budget pressures within the office will permit these funds to be contracted to ASSP. b. The recent expected changes to the budget were not anticipated. The indicative RAR allocation (i.e. for 15/16) and outer years of the project look likely to be lower than forecast in IMA’s contract. We are anticipating that annual forecasted disbursements will be reduced for ASSP and the project extended by one year. It is likely that this will result in early transition out of some health zones. c. DFID DRC contracted £4.7m to UNICEF for a two year project to support CMAM implementation alongside the ASSP project but it is now unlikely that further funds will be identified for RUTF (Ready to Use Food) after the UNICEF project ends, as originally expected. For this reason the UNICEF project is currently being reconfigured – this is discussed in more detail later in the review. Dissemination of lessons learnt from this Annual Review will be through presentation within DFID DRC and a planned article on Insight (DFID’s intranet). DFID DRC presented some learning on the programme during the fragile states session in the Health Adviser CPD conference in early 2014 and a SmartRules case study on procurement about ASSP has been published. ICAI are likely to make recommendations in their forthcoming report on DFID’s work in Fragile States following their review of ASSP in June 2014. Key actions See summary recommendations on page one. Has the log-frame been updated since the last review? Yes. It was not possible to finalise and approve the log-frame indicators during the design phase, because of the time required to agree which indicators to include (i.e. discuss with the MoH/other donors which HSS activities were priorities and were feasible), time to establish baseline data from the SNIS (National health information data) as the data required cleaning (with agreement on which data to exclude and how) and finally, it took time to monitor demand (which was affected by new user fee tariffs and availability of drugs) in order to predict realistic targets on indicators affected by utilisation. As a result of this, the log-frame and milestones were not approved until May 2014. The log-frame will need to be revised once there is agreement on which health zones will be transitioned out and when, as this will affect milestones/results: this, in turn, depends on the conclusion of DFID’s RAR process, and any contract amendment negotiations. 11 C: DETAILED OUTPUT SCORING The log frame outputs for ASSP were set up as part of the business case process prior to the tender and are relatively limited, reflecting DFID’s expectations on what could be achieved based on experience with partners in the previous programme, which focused more, by design and nature, on health service delivery rather than health systems strengthening. Therefore it has been challenging to condense all the varied activities into the existing four outputs. ASSP itself manages the programme according to the six WHO pillars of health systems strengthening. Whilst the indicators themselves, under the key outputs have been adapted to the project, the four outputs remain. For the purposes of this report the various components of the project are reported under the following outputs; Figure 2: How project activities correspond into the four ASSP outputs No. 1 Output Enhanced health service delivery and quality in DFID-supported health zones 2 Increased empowerment and accountability in health service planning and delivery in DFIDsupported health zones Activities Equipping facilities and management teams Pharmaceutical supply chain Capacity building of health facility staff and health zone management teams Improving family planning Nutrition activities Infrastructure construction/rehabilitation progress 3 Improved access to health services in DFIDsupported health zones - 4 Increased and sustainable access to safe drinking water, improved sanitation, hygiene education and better environmental health in rural and peri-urban communities - Community empowerment and accountability component Set up and roll out of national Health Management Information System Human Resources for health work (to address salary issues) Standardisation of tariffs/user fees, Community health endowments (agricultural mutuelles) Policy engagement on relationship between the Government and faith based providers WASH activities The ORIE (Operations research and impact evaluation) component is reported under the section on Monitoring and Evaluation. Activities in the business case contracted outside ASSP are commented on immediately below (as these smaller components are not included in the log frame for ASSP): Demographic Health Survey (UNICEF) The Demographic Health Survey started implementation at the beginning of 2013, after delays during the planning process. DFID is providing its contribution to the DHS through a Memorandum of Understanding with UNICEF. The Minister of Plan chairs the steering committee on a quarterly basis and this meeting is attended by other donors and ICF Macro, the technical partner for implementation of the DHS. A technical committee also meets once a fortnight to discuss operational issues. The preliminary 12 findings of this study have now been successfully published and demonstrate significant improvement in some key indicators, in particular infant/child mortality. Public Financial Management (HEART PEAKS) As part of the institutional capacity building component of this business case, technical assistance is being provided to the DRC Ministry of Health on Public Financial Management (PFM). Good progress has been made so far, with a technical assistant embedded in the Ministry from the end of February 2014 and a more senior consultant providing direction and oversight through a number of short visits. Building on previous consultancy expertise this assistance has so far helped the Ministry, DFID and other donors to better understand the real issues affecting public financial management in the health sector. For example, analysis of budget execution data has clearly shown that the Ministry does in fact spend the majority of the funding made available to it, contrary to the understanding of some donors, but that the link between budgets and plans remains very weak. The technical assistant has also started to build links between the Ministry of Health and other DFID supported programmes such as the Public Financial Management and Accountability (PFMA) programme which is supporting central government finance reforms which will impact on the health sector. Output 1 Enhanced health service delivery and quality in DFID-supported health zones Output number per LF 1 Output Score A+ Risk: Medium Impact weighting (%): 40 Risk revised since last AR? No Impact weighting % revised since last AR? No This output focuses on (i) ensuring that the full package of services is gradually rolled out in facilities (as recommended in the government’s minimum and comprehensive packages) and (ii) that the quality of service delivery is improved. This output relies heavily on all pillars of the health system functioning and therefore includes all the capacity building work in the project. At the time of writing this review, data is only available on one of the four indicators for this output (whose performance was directly affected by the delay in issuing the implementation contract). Therefore the assessment of this output has drawn upon wider information on progress on the relevant activities in the work-plan (as outlined in figure 2 i.e. equipping facilities and management teams, pharmaceutical supply chain, capacity building of health facility staff and health zone management teams, improving family planning, nutrition and infrastructure construction/rehabilitation). Indicator(s) Number of facilities offering Comprehensive Emergency Obstetric and Neonatal care (LCS, blood transfusion etc) Number of new acceptors of modern methods of family planning (KPI) Milestones 2013/2014 112 Progress (to May 2014) 107,863 88,779. This indicator was affected by delay in procuring commodities as a result in the delay from DFID issuing the implementation contract. Data awaited from end of project household survey Percentage of children under five with diarrhoea who received either ORS or RHS NA Percentage of Health Facilities reporting drug stock-outs for at least one of the following five Data will not be available until year 2 13 Data awaited from health facility survey in year two Not applicable drugs (Depo Provera, Oxytocin, SP, Zinc, Amoxicilin 250mg) Key Points ASSP has managed to support health care services across a population of almost 8.6 million people in its first year of implementation. ASSP is already demonstrating good results from improved services as demonstrated by good performance of outcome indicators such as skilled birth attendance, vaccination coverage, presumptive treatment of Malaria in pregnancy and couple years protection for family planning. This is exceptional, given that roll out of a new project over such a large programme area in this context would probably reasonably be expected to take two years and normally one would not expect improvements in quality until after equipment, supplies and trainings have been put in place during the first year, and clearly reflects IMA’s strong track record and leverage in DRC. IMA has demonstrated the ability to conduct large scale procurements of supplies and equipment and then import and distribute items efficiently2. Time taken to clear imports is considerable faster than expected and distribution to Provinces was rapid (in part from necessity because of lack of warehouse capacity in Kinshasa). The drug stock-out issues in year one were mainly because i) DFID failed to issue the full implementation contract in a timely fashion, which delayed placement of the initial order and ii) because of the policy of distributing through the government pull systems using CDRs – i.e. taking a more long-term sustainable approach. Capacity building of health facility staff and health zone management teams has begun and feedback from health zone management teams has been positive. Teams now have vehicles to conduct supervisions and operational allowances but there are opportunities to promote more supervision by DPS and health zone teams. Training on family planning and reproductive, neonatal and maternal health in particular were extensive with over 50 MoH “fiches techniques” being revised prior to this. Progress on infrastructure has been slower than originally anticipated. But this has been partly because the Ministry of Health were involved in designing and approving the construction plans as they wanted to adopt these nationally – and have done so. Moving forward the number of new constructions and rehabilitations has been revised down due i) the leveraging of extra resources through the inclusion of 80 health centres in ASSP health zones under the Government’s PESS project (which builds and equips health facilities) (ii) contraction of timeframe resulting from time taken to agree designs and (iii) revisions of cost estimates which were impacted by increased specification requested by the MoH. Section D on VFM provides a detailed breakdown on revised targets and unit costs. Feedback from the Ministry of Health and from the annual review field visit has highlighted that construction is both a strategic priority for the Ministry and that lack of ownership of facilities imposes an additional cost barrier for users as facilities are forced to raise user fees to cover rental of buildings from private landlords. Nutrition was not included to any major extent in the terms of reference but activities were added as a cost-neutral budget amendment after IMA identified that this was a significant issue which would hold back delivery on infant/child mortality results. IMA have started rolling out an package of activities which have strengthening home/community capacity on malnutrition at their core in order to promote long term sustainability. The package includes behaviour change communication on nutrition including promotion of household gardens and home based treatment of malnutrition using high energy porridge. This work has drawn attention from other donors and the Ministry and is the subject of an operations research study by Tulane University. Family planning activities have made a good start with strong demand for longer acting methods of contraception (as demonstrated by the Couple Years Protection target exceeding expectations in the first year). Pathfinder have worked through the Ministry of Health to update national protocols/deliver training to health workers and have worked more broadly on a range of reproductive health issues including SGBV and treatment of fistulae (which exceeded expectations as this was not included in the ToR). 2 Confirmed by paragraph 12 Stefan Dercon’s Congo Note 2 report following visit in 2013 to DRC. 14 Summary of responses to issues raised in previous annual reviews Issue raised in previous review 1. IMA need to give on-going high priority to good coordination and effective communication between consortium members, supported by clear definition of roles. Response Communication has improved in general. Terms of reference for the ORIE and FP components have now been agreed. Quarterly partners’ meetings have been strong with emphasis on holding partners to account on delivery of work plans. 2. IMA should give high priority to articulating the programme and its approach to stakeholders, both directly and indirectly through its implementing partners. At the same time, DFID DRC should seek to maintain as high a level of interaction with provincial authorities as possible, in order to strengthen awareness of the programme at that level and generate commitment to it. IMA and DFID have been working on a communications strategy. DFID has had frequent engagement with authorities in Kasai Occidental in particular. DFID plan to travel to South Kivu in July 2014 and will meet with provincial authorities as this province in particular has had limited engagement with DFID. 3. IMA should develop and present an action plan An action plan has been developed in conjunction for managing this risk (particularly in Maniema with the Ministry of Health and stakeholders. where drug management is thought to particular need of strengthening) in order to avoid stockouts and minimise fiduciary risk. Recommendations - IMA should update the action plan on pharmaceuticals supply chain. Going forward, the action plan should include both an operational and a strategic plan with plans for starting some procurement through FEDECAM (the national drug procurement agency). - Develop a plan on how health zones will be transitioned through different phases of support within the project (e.g. development, consolidation and maintenance phases). - DFID should contract some third party monitoring using health programme funds if a cross office contract has not been tendered by the end of 2014. - DFID should put in place longer term advisory expertise to oversee construction (either through 10% cadre input or as cross office- consultancy). Output 2 Increased empowerment and accountability in health service planning and delivery in DFID-supported health zones Output number per LF 2 Output Score A+ Risk: Medium Impact weighting (%): 20% Risk revised since last AR? No Impact weighting % revised since last AR? No Indicator(s) Number of assisted health centre in which a community score card is completed each year (The score card will include measurement of community satisfaction and health services fees) Number of health zones implementing IHRIS Number and Percentage of HZs using DHIS 2 for Routine Health Information reporting Milestones 2013/2014 Not planned until year 2 Not planned until year 2 Not planned until year 2 This output covers community level activities in the empowerment/accountability component of ASSP, the work on setting up and rolling out the new national health information system (DHIS-2) and the work on Human Resources for health (which focuses on using information to improve the proportion of staff who receive salaries). 15 Key Points The Community empowerment and accountability component includes three main activities; reinvigoration of CODESAs (health committees), piloting community score cards and piloting an SMS toll free hotline for citizens to report fraud and service problems. IMA has taken time to build on learning from the DFID-funded Tuungane programme and has conducted some initial research to inform implementation. The Annual Review field visit found that at Mutombo Dibue health centre and Munkamba referral health centre, there was strong commitment and ownership by the community, and the CODESA was very dynamic, being practically involved in drug management and seeking solutions to a range of problems experienced in running the health centre. The work on Human Resources for Health was not originally expected within the project, but was developed after IMA identified that the lack of government salaries of health care workers would affect project results and sustainability long term. IMA have been working in conjunction with IntraHealth to assist the MoH to revise norms and standards on staffing levels using the WHO WISN methodology3. Plans to roll out an HR information system (I-HRIS) have been deliberately slowed down to ensure that the work on validating staffing lists is done in conjunction with work planned with the Ministry of Public Service and the World Bank. This is a very challenging area of work and its inclusion in the project has exceeded expectations in terms of what DFID expected (which was limited to an expectation of local advocacy to include staff on the payroll). ASSP does not pay primes (incentives) to health facility front-line staff, as this is unsustainable. Instead, to maintain health worker motivation, a standard tariff for user fees together with improved access to drugs/commodities has meant that clinic revenues have improved so that staff are able to take an increased “prime locale”. This has exceeded expectations (there had been fears that staff would be unmotivated with the policy on no project primes). The annual review field visit found that all health facilities in the three zones visited had experienced a significant increase in their local revenues, especially at the hospital level than at the health centre level. For example, in llebo, the “prime locale” for a physician working at the general referral hospital increased from 50.000 FC to 200.000 FC, the prime locale for nurses increased from 17,000 FC to 30.000 FC and in Mweka health centre, the prime locale for nurses rose from 2000 FC to 10,000 FC. Alongside this, Tulane University are conducting some operations research on health worker motivation, in particular examining the case of the transition of support in health zones under the previous project. No specific recommendations were made in the last review on this output. Output 3 Improved access to health services in DFID-supported health zones Output number per LF 3 Output Score A Risk: Medium Impact weighting (%): 20% Risk revised since last AR? No Impact weighting % revised since last AR? No Indicator(s) Utilisation per capita per annum (disaggregated by sex) for curative consultations Number of new consultations of pregnant women and children under five (curative consultations) Milestones 2013/2014 0.37 Progress 0.34 Not available Data not available Improving access to health services in ASSP is addressed through activities to ensure tariffs/user fees are regulated, clinics have alternative sources of income to subsidise fees through piloting of community 3 Workload Indicators of Staffing Need 16 health endowments (agricultural mutuelles) and facilitating policy engagement between the Government and faith based providers on what contribution the MoH makes to faith based providers. Key Points The starting point of access to health services is their availability. This project has extended support of health services to 56 Zones, significantly more than the 20 of the predecessor project, or the 30 projected in the business case. The utilisation per capita progress above is in the context of the late signing of the full implementation contract, meaning that full implementation did not start in all health zones until the second quarter of the year. Unhindered by this, utilisation would probably have materially exceeded the year one milestone, and is on track to exceed the eventual target. DFID’s general policy is universal or free health care. However, as DRC is a uniquely challenging context in terms of public financing of basic services and in view of the serious lack of prospects for medium-term sustainability on the government side of the kind one would conventionally move towards, DFID agreed that the use of regulated user fees (with subsidies and exemptions) is a more sustainable locally adapted version of universal health care. The programme has supported the setting of health-zone wide tariffs for user fees negotiated with beneficiaries and provincial authorities. This is set out in the ASSP strategy on user fees and access for vulnerable patients. In general, the revised tariffs are considerably lower than prior to the project. The annual review field visit found that the prices of consultation and medical interventions have significantly decreased: for example the fee for a caesarean section decreased from 130USD to 17USD in Ilebo Health zone, the management of an episode of malaria in Mweka Health zone has decreased from 8000 FC to 1000 FC and the fee for major surgery has decreased from 80,000 FC to 15,000 FC in Katende Health Zone. Of critical importance for results and value for money is ensuring that utilisation rates are adequate and that the poorest and most vulnerable are still able to access care. DFID assessed initially that the benefit of the increase in coverage that the new programme has delivered through its efficiencies outweighs the risk of decrease of uptake per user as a result of user fees. Early modelling by DFID showed that this would not be the case below about 0.4 consultations per person per year in ASSP and therefore it is crucial that utilisation rates continue to rise in the second year of the project. IMA is monitoring the elasticity of demand and barriers to access on utilisation in a number of ways. IMA reports to DFID on utilisation rate by health zone in the health zone score board of four key indicators as part of the quarterly narrative reports, so DFID has good visibility on differences at health zone level. Monitoring use of health care services by the poor and vulnerable is being assessed as part of the user fee operational research study being conducted under the ORIE component by Tulane University. This will ensure appropriate steps will be taken promptly within the project to ensure that fees are not a barrier to access. Progress on improvement in utilisation rates varies according to whether the health zone was supported under the previous project or not. In new health zones utilisation rates have increased markedly. The annual review field visit found that despite some shortages for some medicines, people are satisfied with the availability of essential drugs in all health facilities visited and this has encouraged patients to continue to use health services; For example, in Mweka health zone, the utilisation rate of curative services increased from 7-8% to 13-14% during the first nine months of ASSP’s implementation. The number of new patients rose from 40 to 170 per month. In the health centre at Mutombo Dibue, the use of services increased from 12% to 30%. The general referral hospital of Katende has seen the number of monthly visits increased from 60 to 350-400 since the beginning of the project. As expected by DFID, health zones supported under the previous project experienced a fall in utilisation rates with the change in policy under the new project on the reintroduction of user fees, phased withdrawal of frontline staff primes and moving to a government based pull drug system which has disrupted drug supply. Currently, utilisation rates overall stand at about 0.34 consultations per patient 17 per year with the final target for the project being 0.6 (which is intentionally lower than the 0.65-0.7 target under the previous project). Community health endowments. This component is piloting the use of community cooperative agriculture which generates health facility revenue for local primes and provides subsidised care for contributing households (effectively acting as a risk pooling mechanism). The pilot is being followed by an operations research study. Early findings show that communities may be concealing true yields from the fields and therefore changes have been made in terms of agreement of a minimum rather than percentage contribution to health facilities. Some communities have adapted this to a hybrid cash-based mutuelle as some households prefer to contribute cash rather than labour. At this stage it is too early to predict the results of this pilot. The findings are likely to generate significant interest as few mutuelle schemes have been successful in the poorest most rural areas of DRC. Policy engagement on faith based provision has exceeded expectations in the degree of progress that has been made. IMA facilitated the negotiation of the revised Memorandum of Understanding between the major faith based institutions and the Government (which outlines commitments in terms of salaries, tax exemptions etc.). IMA has also updated a mapping/assessment of faith based services and has engaged on mobilising state support (for example ensuring equal support for faith based facilities through the government’s PESS project). Moving forward the challenge will be to invigorate coordination of the Corels (faith based organisations) and then to continue to keep discussions open on the potential for future commissioning of services by Government through faith based providers. DFID has continued to prompt IMA that this policy engagement is a strategic priority, which was unexpected to IMA as this is not an area that donors have engaged on before: IMA, as a faith-based organisation with extensive government-collaboration experience, is uniquely well-placed to deliver in this area. Summary of responses to issues raised in previous annual reviews None Recommendations IMA should further develop policy engagement with the Ministry of Health on faith based providers to strengthen coordination of corels (faith based organisations) and facilitate further discussions on the relationship between faith based providers and government. Output 4 Increased and sustainable access to safe drinking water, improved sanitation, hygiene education and better environmental health in rural and peri-urban communities Output number per LF 4 Output Score A Risk: Medium Impact weighting (%): 20% Risk revised since last AR? No Impact weighting % revised since last AR? No Indicator(s) Number of villages which have completed the Village Assaini process in targeted Health Zones; Number and Percentage of population (rights holders) with access to safe drinking water; (KPI) Number and Percentage of population (rights holders) who have access to, and use, adequate sanitation; Milestones 2013/2014 Not planned until year 2 Not planned until year 2 Not planned until year 2 Key Points The WASH activities were delayed by a delay in DFID approving the work-plan and approach within ASSP. To date, DFID has mainly funded the Village Assaini approach in WASH in DRC. Whilst it has 18 demonstrated good results, it is quite an intensive, time-consuming process and is quite costly. Currently, less than 15% of DRC has benefitted from Village Assaini and it remains unclear whether the relevant government line ministries will have capacity to continue to roll out this approach in the absence of external donor support in the long-run. Findings from the initial assessment within ASSP also showed that issues of water quality were being insufficiently addressed within the Village Assaini package. After some discussion, DFID approved IMA to roll out a mixture of WASH activities including both Village Assaini and some “hybrid” approach sites with water quality interventions including filters and cisterns. The hybrid approach proposed by IMA is novel and therefore Tulane University is running an operations research study alongside to compare the cost-effectiveness of both approaches. IMA will need to ensure that where Village Assaini is rolled out, that they adhere strictly to the VEA phase II guidance as set out by the Ministry of Health and fully consider the community level work within the package. The end of project milestone is for 370,400 people to access water and sanitation. This is lower than the forecast number in our original business case (which showed for a budget of £17m DFID expected 600,000 to access water/sanitation). This is because the original estimates done by DFID were based on Village Assaini phase I, which underestimated costs considerably. Based on a budget of £17m, the total cost per capita in ASSP currently stands at £45 per person (compared to £30 per person for UNICEF). This is higher because ASSP also includes activities over and above Village Assaini i.e. in particular the construction of latrines/cisterns/filters in health facilities and provision of cisterns/social marketing filters. When these are removed, the planned cost for VA are considerably lower (depending on the definition of what is included in the VA package). This will need to be monitored during the life of the project. Moving forward, there is a risk that the WASH component may need to be scaled down due to budget pressures resulting from the RAR allocation. Summary of responses to issues raised in previous annual reviews None Recommendations The budget will need reviewing moving forward and further analysis on cost per capita (excluding institutional support) should be conducted as part of that. 19 Gender ASSP has now finalised its gender strategy which sets out clearly the objectives of the project (Quest number 4501070). The 2013 ASSP gender review (using standard DFID DRC methodology) gave the programme an amber rating along with recommendations for improvement (see Columns 1, 2 & 3 below). Column 4 summarises actions taken by ASSP in year one of implementation and the updated score agreed in the gender review meeting which was conducted as part of the annual review process on 25th June 2014. Criterion Observations (2013) 1. Does the programme design include comprehensive analysis of the situation of women and girls? Amber: The programme design includes a degree of analysis of the situation of women and girls, but this cannot be considered to be comprehensive. It was anticipated that this would be included in the baseline situational analyses performed in each of the health zones, but it is not clear that this has been done. There is as yet no specific gender strategy for the programme. 2. Does the Amber: The logframe includes logframe include indicators that relate specifically to results and women and girls, and disaggregation indicators relating to of indicators by age is planned. W&G, and those However, the current logframe does that include not fully capture transformative transformative change for women and girls (although change? utilisation rates disaggregated by gender will do so to an extent). 3. Does the Theory of Change explicitly refer to W&G throughout? Amber: The proposed revised TOC presented by IMA refers explicitly to women and girls, but does not demonstrate how outcomes for women and girls are expected to be achieved, and what change will occur as a result. 4. Does programme Amber: Implementation plans have elements that demonstrate some awareness of seek to address discriminatory socio-cultural norms, discriminatory but this is not yet sufficiently socio-cultural systematic, nor is it clear yet to what norms? extent and how these will be challenged through the programme. 5. Does programme contain specific measures on adolescent girls? Green: The programme contains specific measures for providing services to adolescents, including sexual and reproductive health services. Recommendations from 2013 A gender strategy should be developed, and be based upon comprehensive analysis of the situation of women and girls in the health zones to be supported. As the community E+A component is further developed, at least one indicator that captures the transformative impact of this for women and girls should be considered for inclusion in the logframe. A specific theory of change for gender should be developed as part of the gender strategy for the programme. The gender strategy should include an analysis of such norms in the health zones (HZ) that will be supported and present realistic plans for challenging these through the programme. Plans for meeting needs of adolescents now need to be operationalized, and should as much as possible be included in the community empowerment and 20 Actions Taken 2013-14 Amber Green: The ASSP gender strategy has been developed and approved by DFID. It includes a comprehensive situational analysis of women and girls for the five provinces where ASSP is operating. Green: 1) ASSP has included a proxy indicator for delaying first pregnancy by working with the MOH to disaggregate FP data by age group, including a dedicated indicator within SNIS i.e. number of acceptors < 20 years of age. 2) ASSP IPs will measure and disaggregate data on women/girls access to selected health services. 3) An E+A gender indicator was created for the “Village Santé” to track representation of women in CAC (communities committees). 4) Pathfinder’s programme includes education on masculinity as part of its work on VAWG (Violence against Women and Girls). Green: A gender-specific Theory of Change was developed by Pathfinder and is included in the ASSP project Gender Strategy. Green: The gender strategy includes a detailed situational analysis of discriminatory sociocultural norms for the five supported-provinces. The strategy also includes behaviour change approaches and realistic plans to address such norms. Links to La Pépinière have been made by DFID. Green: The integration of Adolescents and youth sexual and reproductive Health (AYSRH) in the ASSP-supported HZs is planned for the year 2 of the project. Pathfinder is currently providing support to the MOH to update/adapt the AYSRH training materials on SRH Youth Criterion Recommendations from 2013 accountability component. The programme should reflect on the extent to which provision of SRH services to adolescents is constrained by the legal framework, and discuss with DFID where there may be opportunities to seek change. 6. Does the Green (provided this is implemented): A clear job description programme have During the annual review, IMA and should be developed, appropriate and Pathfinder confirmed that a gender in order to obtain the adequate plans and lead will be recruited in the coming appropriate scope and resources for weeks, and that this individual will be level of gender gender technical responsible for overseeing expertise. support? development and implementation of a gender strategy for the programme. 7. Do implementing partners demonstrate a strong commitment to gender issues, have adequate gender capacity and a clear gender action plan? Observations (2013) Amber: The evidence for this is currently incomplete. A gender lead and a gender action plan are not yet in place, but commitments to these have been provided by the consortium. 8. Are the Amber: These commitments have programme-specific been partly addressed. commitments in the Action Plan for Gender? OVERALL AMBER Actions Taken 2013-14 Friendly Services and Peer education. ASSP will need to continue to address data issues on monitoring this and clearly define adolescents. Green: A technical Gender advisor has been hired since November 2013. She supported the development of the ASSP gender strategy and is overseeing its implementation. A help-desk literature review was commissioned by DFID on reaching adolescents with sexual and reproductive health services. The level of Amber Green: The ASSP gender commitment to gender strategy includes a gender traffic issues will need to be light table that will make possible to further assessed at the track progress made by IPs on next and subsequent implementing the gender strategy, annual reviews. starting in Year 2. The IPs have been briefed on the gender strategy including the gender traffic light table and have integrated specific gender activities in their Year 2 work plans. The commitments Amber: Program specific need to be addressed commitments in the Action Plan for in the gender strategy Gender are being implemented. for ASSP. These efforts will be strengthened with the integration of AYSRH activities. GREEN 21 D: VALUE FOR MONEY & FINANCIAL PERFORMANCE Key cost drivers and performance DFID’s total expenditure for the financial year 2013/14 has been £27.0m with total expenditure to date running at £35.3m out of a total budget of £184.9 million. £25.7m of the 2013/14 expenditure was through the ASSP programme, and £1.3m was used to support the latest District Health Survey4. The latest financial reports show that the major programme costs incurred by IMA in year one of ASSP were for health supplies, payments to support health zone management and equipment costs as well as transport and staff costs as shown in the table below. This represents a change from the previous annual review as the programme has now moved into its implementation phase. IMA’s expenditure is higher than DFID’s expenditure due to a payment made in the design phase in the previous financial year. Budget Category Health Supplies Malaria Supplies Health Equipment Health Zone support payments Training Health Activities, Meetings and Studies Community Health Endowment Solar Equipment WASH Procurement and Logistics Construction & Rehabilitation Staff and Communications Management Fees Total Total Y1 Expenditure by IMA % of Y1 expenditure by IMA £8,347,376 £895,229 £3,179,207 £3,972,426 £1,331,745 £1,151,441 £47,307 £643,512 £1,900,140 £3,551,206 £201,054 £3,644,858 £1,790,106 £30,655,606 27% 3% 10% 13% 4% 4% 0% 2% 6% 12% 1% 12% 6% 100% In total in ASSP about 20% is spent on indirect costs (including management fees), with another 20% spent on health systems strengthening and the remaining 60% going towards service delivery. VfM performance compared to the original VfM proposition in the business case Cost per capita and population covered have exceeded expectations. In comparison to the old Access to Healthcare programme, ASSP was a scale up in terms of funding, with an increase of 83%, but this delivered a more than proportionate scale up in terms of the population covered, with an increase of 247% by increasing support from 20 to 56 health zones, giving a coverage of 8.6m people. The project exceeded expectations significantly as the business case estimated that at around 30 zones would be supported from this envelope of funds. The cost per capita for support to basic service delivery has halved, from 14 USD per capita per annum in the previous project to 7 USD. DFID achieved such a large increase in the population covered by changing the model of service delivery (working more through government delivery systems rather than in parallel) and changing supplier through an international competitive tender. Our estimation is that whilst this change in model has resulted in an initial reduction in utilisation rates in the 20 ‘old’ (former A2H2) zones, if the project achieves its final target rate of 0.6 per capita per year, the overall result will be an increase of 73,180 people accessing healthcare per £1m invested by DFID. 4 Expenditure on PFM falls outside the period of this review (to March 2014). 22 The business case identified that the main factor which affects cost-effectiveness is the coverage of the intervention i.e. uptake of the specific services. This is affected on the demand side by user fees and on the supply side by the quality and success encouraging uptake e.g. family planning. The business case compared different levels of donor support from 3 USD to 13 USD per capita to provide a package of interventions including child & maternal health, nutrition, family planning, malaria and water & sanitation. The different levels of support were compared by estimating the expected Disability Adjusted Life Years (DALYs) averted which informed the decision to select a mid-cost managed programme model rather than continuing with the previous high cost programme or switching to a lower cost model. Given the above, the business case highlights that the uptake of services will be key to ensuring VfM of the selected model. The business case also sets out a number of measures to be used to track VfM during the programme. Some of this will be tracked through the operational research component specifically looking at VfM. The figure below shows the breakdown of expenditure in year 1 between direct, indirect and capital costs and what this equates to per capita based on an estimated target population of 8.6 million. Direct costs include all drugs, equipment, training as well as the cost of procuring and delivering these interventions. Indirect costs cover all programme staff and office expenses and management fees. Capital costs cover all infrastructure and equipment such as solar panels and vehicles. The figure below shows an estimated 6 USD per capita although in reality it will be closer to 7 USD in year two given that full implementation did not start in all health zones until the second quarter of the year. This illustrates a significant change in comparison with the much higher per capita expenditure under the previous programme and shows that the programme is currently spending roughly in line with the per capita level showed to be most cost-effective in the business case. Figure 3: Direct, indirect and capital investments per capita in year one Y1 Expenditure Per capita Direct costs £18,234,194 $4 Indirect costs £7,067,013 $1 Capital costs £5,354,399 $1 Total £30,655,606 $6 The following figure shows an estimation of how infrastructure costs have changed over the inception phase of the programme. While some unit costs have increased, as plans for what new health centres should look like have been finalised, there has also been a reduction in the overall total due to the government infrastructure programme targeting some ASSP health zones. The cost of constructing health centres through ASSP is currently estimated at 93,000 USD per structure or 465 USD per square meter. This compares favourably with construction costs seen in DFID’s police reform programme of 510-650 USD per square meter and has attracted significant interest from the DRC government. Figure 4: Construction costs as compared to original costs Minor Repairs HCs Original Construction Targets 156 Original Estimated Unit Cost (£) 6,000 936,000 Revised Construction Targets 125 Revised Estimated Unit Cost (£) 6,452 Major Repairs HCs 156 12,903 2,012,903 125 19,355 2,419,355 New HCs 260 3 53,019 13,785,032 200 55,484 11,096,774 322,581 967,742 2 322,581 645,161 Rehab HGRs 104 12,903 1,341,935 52 19,355 1,006,452 Build new HGR Buildings 78 45,161 3,522,581 52 45,161 2,348,387 Repair nursing schools 52 16,129 838,710 25 16,129 403,226 Incinerators 624 780 486,452 624 780 486,452 Placenta Pits 624 323 201,290 624 323 201,290 Total 2057 24,092,645 1829 Construction New HGRs Original Total (£) 806,452 19,413,548 Difference 23 Revised Total (£) 4,679,097 Assessment of whether the programme continues to represent value for money This programme has shown good, if slightly delayed, progress in getting up to full implementation over the course of the first year and has demonstrated that it can manage expenditure at this scale in the challenging context that DRC provides. Overall, we are content that the programme is on track to deliver value for money over the course of the intervention. The delay in hitting utilisation targets will have had an impact on the VfM of this intervention this year but this was expected and is in large part due to the change of approach of using the state drug depots (CDRs) rather than providing drugs directly through an NGO. This approach may take longer to get fully functioning but will have a much more sustainable impact, well after this programme has ended. We will need to follow utilisation rates, along with other indicators of coverage, with care to check that by year 2 of the programme we are meeting the expectations on utilisation rates as well as delivering the strategy set out in the business case in terms of strengthening the health system. Through the Operations Research component contracted to Tulane University, DFID is funding an OR study to look at outcomes for different levels of donor investment per capita using field data from the ASSP project and other donors’ projects. Quality of financial management Despite large variations in quarterly invoices, DFID in fact disbursed almost exactly what was forecast in year one of the programme. The variations against quarterly forecasts were driven by delays to the construction component of the programme and uncertainties over when invoices for large drug and equipment orders would arrive. Given the scale and complexity of the programme we are satisfied that financial management systems that have been put in place are improving and will now be looking for greater accuracy in quarterly forecasts. Reporting requirements have been met although the arrangements for exactly what the narrative reports should contain has been an on-going process. Financial reporting has similarly gone through a number of iterations over the year but has now settled on a format which works well. Auditing arrangements have now been put into place following the recommendations of the Due Diligence Assessment with an internal audit function to start next year. Date of last narrative & financial reports Date of last audited annual statement June 2014 July 2014 E: RISK Overview of programme risk Achieving results The key risks to DFID achieving the planned results were set out in the Business Case: - Insufficient commitment from the Ministry of Health (MoH) at all levels (central, provincial and zonal) particularly financial commitment on salaries; - Insecurity from conflict reducing access; - Corruption and diversion of funds particularly from sub-contracted partners or operational funds delegated for use by health management teams; - Provincial / zonal health authorities not having sufficient capacity to manage or monitor basic service provision to ensure adequate quality care; - Weakness of data collection, quality and processing for monitoring and evaluation making it difficult to judge programme effectiveness. 24 DFID and IMA have secured strong MoH commitment at the central level, and strong commitment from Government at Provincial and Zonal level, both publicly and in practical terms. This greatly mitigates the principal risk identified in the Business Case. The most major concern is whether progress will be made on government salaries. Currently, it is not uncommon to find only 30% of staff in a health facility receiving a salary. IMA’s activities on human resources for health are ambitious and even if these activities are well implemented, the salary situation may not have improved by the end of the project without strong government commitment for change. Insecurity from conflict remains a risk and there have been occasions when implementing agencies have had to temporarily reduce their support to certain zones. To ensure a consistent approach to these situations IMA with implementing partners are developing a Business Continuity Plan (BCP). An assessment of conflict was made during the needs assessment to ensure that they are aware of political/ethnic tensions in the individual areas where they operate. Together with the programme risk matrix that IMA maintains, these will form a package to assure the resilience of DFID’s investment. There remains an opportunity for IMA and implementing partners to do more formal conflict assessments but realistically, DFID would need to provide technical assistance for further in depth work as this is not a core capacity of health NGOs. Communications equipment of IPs was found to be limited on the annual review field visit and IMA should review this. Corruption and diversion of funds by implementing partners is an on-going risk. We consider that the planned and existing programme checks and controls (implemented as outlined in the business case) provide adequate assurance that UK funds are not lost to fraud or corruption. Anti- bribery and corruption policies are in all contractual documents and DFID’s zero tolerance approach to fraud is understood by partners. IMA conducted anti -bribery and corruption training for partners to reinforce the policy provision in their contracts. This is linked to regular financial forecasting and reporting, backed up by internal and external audits. DFID’s financial oversight of the project will be strengthened with the planned recruitment of an A2 finance officer for the office. DFID continues to ensure that the Consortium Lead and implementing partners have robust policy and financial procedures. The results and recommendations of the first of the annual external audits are being finalised. IMA has hired a Deputy Director of Operations to oversee IMA’s procurement and logistics departments, including management and tracking of assets, which are held mainly by partners. Effective data collection is a challenge, both in terms of technical collection and receiving it on a regular and timely basis. Systems are being put in place to improve processes mainly for the MoH to better manage resources through the roll out of the new HMIS system, but this will take time. Data quality reviews (RDQA) are planned for year two to enable MoH officials to audit quality of data received from health zones. DFID should additionally set up some third party monitoring capacity to do spot checks themselves. Outstanding actions from risk assessment A Due Diligence Assessment (DDA) of IMA identified a number of opportunities to optimise the management of fiduciary and other forms of risk in ASSP. Audit and resilience are the two areas in the DDA where there is still work to complete. IMA has made progress on creating its internal audit function. The Director of Compliance and Internal Auditor positions have been filled. The internal auditor will be based at IMA’s headquarters and will report to the board of directors. His first assignment will be in the DRC to focus on the ASSP program. External Audits of the downstream partners have just been completed and the report and recommendations will inform the planned full programme audit. DFID has requested an external project audit and is in the process of agreeing terms of reference for this. Overall risk rating: Medium 25 F: COMMERCIAL CONSIDERATIONS Delivery against planned timeframe There was a significant delay in DFID issuing the implementation contract for IMA which has meant that full implementation across all zones, which was expected to commence in January 2013 did not commence until July 2013 – implementation in the previous 20 health zones commenced in April 2013. Agreement and approval of a number of key components of the project took longer than expected in particular approval of WASH activities, community empowerment and accountability component, Community Health Endowment component. This was due to the time taken to reach agreement between DFID with IMA on approach. This was also affected to some degree by lack of clarity on expectations from DFID and the time taken to consult/draw on expertise of cross-cutting advisers within DFID. (See lessons learnt point on importance of space to pilot/take risks and learn within the project). Figure 5: Timeline of key decisions for ASSP Step Expected date Approval of strategic case Approval of BC Actual date Comments Quest number 20/09/2011 25/05/2012 Director level approval Approval by SoS 3214149 3531143 Preferred bidder selected 02/07/2012 13/07/2012 OJEU ICB Design contract awarded 30/8/2012 18/10/2012 Only £15m contract awarded (Staffing continuity issue in PRG) End of design phase Breakpoint approval 31/12/2012 28/02/2013 28/02/2013 19/03/2013 Implementation contract awarded 01/03/2013 05/06/2013 01/04/2013 01/04/2013 5 months of design phase (longer than predicted 3 month period) Design phase report approval Delay from March to June due to change in policy requiring higher level approval. Implementation started in April for existing zones, July for new zones End of design phase 14/02/2014 Drafted by DFID on behalf of IMA 4367453 21/10/13 Time taken to reach agreement on approach (i.e. extent of use of Village Assaini). 4202350 End of design phase October 2013 Design work by PACT the original partner was not accepted and decision made for IMA to implement this themselves. End of design phase 10/10/2013 Pilot approved with approval for extensions of pilot 17/4/14 Implementation phase Delayed design deliverable: ORIE ToRs Approval of WASH component Approval of Community Empowerment and Accountability component Approval of CHE (Community health endowment component) End of design phase 26 3736131 3911194 3763721 4189995 4446681 Delayed design deliverable: Approval of log-frame End design phase Feb 2013 DFID and IMA underestimated time required to collect and clean SNIS (national data) for indicator baselines 25/5/14 4457436 In terms of impact of these delays on results, since the log-frame was not finalised until May 2014, most milestones already reflect the delays e.g. no WASH milestone was set for the first year of the project. The RAR budget revision has meant that to reduce in year expenditure, it looks likely that DFID will require ASSP to reduce annual forecasts on expenditure and the project will be extended by one year to retain the original value of the contract. Reducing in year expenditure will have an impact on results as delayed investments in construction in year two for example mean that full utilisation rates won’t be realised until later in the project and the number of health zones supported will also be reduced meaning that direct:indirect ratios will be less good value (as overheads will remain): in short, removing elements of an integrated programme will result in reductions in value for money disproportionate to the funds saved. It will be important for DFID DRC to analyse the benefits of projected alternative uses of these funds relative to this opportunity cost. Performance of partnerships There are currently nine direct project partners in the consortium that is implementing ASSP. As consortium lead, the role of IMA is to manage delivery by downstream partners, set the overarching operational framework for the programme, to manage essential activities such as procurement and infrastructure development and provide technical oversight/strategic direction for the project (whilst working closely with the Ministry of Health centrally). Technical partners are responsible for providing the programme with specific expertise in key areas, and for supporting the implementing partners to deliver in each of those areas. The implementing partners in turn are responsible for directly providing support to service delivery at health zone level. IMA continues to perform very strongly as the consortium lead. In particular, it has exceeded expectations on providing technical direction and strategic oversight to the programme. Whilst many funds have fund management agencies which can administrate grants to implementing partners and carry out routine monitoring of implementation, IMA has gone much further, providing strong technical oversight, setting clear directions for IPs (based on government policy), investing resources in understanding the blockages/issues within the health system and then proactively designing and implementing interventions working with the Ministry to address those. IMA has built up a very strong relationship with the Ministry which has resulted in strong Government ownership. Officials from the Ministry have on a number of occasions referred to ASSP as “their” project and have been very actively involved in chairing quarterly partners’ meetings, doing joint field visits and contributing staff to work on key components e.g. HMIS roll out. Components are developed in conjunction with the MoH before being rolled out so that the project is actively contributing to building the government health system rather than just seeking to implement the project. For example work to revitalise CODESAs (community health committees) began by assisting the MoH to redraft their guidance and the construction designs for new health facilities in the project have been adopted by the MoH as a blueprint for future government construction. IMA have demonstrated strong management skills in overseeing implementation partners and feedback from IPs indicates has been generally favourable, particularly now that the pattern of disbursements has become more regular. IPs commented that they received good technical support but that communication could be improved e.g. planning of visits from IMA/technical partners to set up new work on health systems strengthening or nutrition for example. Performance of implementing partners at provincial level has been fairly strong with some variation in capacity between organisations. In particular, SANRU (a local NGO) has performed strongly and has 27 demonstrated flexibility in taking on the newer components in the project as they have been introduced e.g. nutrition. Oversight of the technical contracts has been more varied and probably reflects more on the programme design than IMA’s capacity. With hindsight, it is unclear whether setting up the Operations Research and Impact Evaluation component as a sub-contract was the most optimal way of contracting this. DFID was reluctant to procure and manage a separate contract. It was felt that as the emphasis was on operations/action research i.e. learning and applying findings within the project meant that there was a benefit to the research institution being managed directly by the consortium lead. In practice, the management and oversight of a large research contract is highly specialised (something which even DFID centrally contract out additional technical support for) and it was unrealistic to expect a health NGO to be able to do this. In practice, IMA has been flexible and DFID has practically assumed some of the technical oversight of this sub-contract, whilst IMA continues to do the contract/financial management. For example, DFID drew up terms of reference for Tulane, drafted an improvement plan and set up the oversight committee to ensure strong governance and independence of the research produced. It is unclear whether there are concrete advantages of subcontracting the family planning component as a separate sub-contract to another INGO. DFID did not specify this as a requirement, only that this component had ring-fenced funding and activities. This has conferred an additional layer of administration and overheads when IMA could probably have developed capacity for this in-house. Going forward it may be worth reviewing the cost-benefits of this arrangement particularly with additional cost pressures from the RAR budget revisions. Feedback on how DFID could be a more effective partner has highlighted a number of key issues. The importance of setting out expectations more clearly at the outset in writing (for example on quality of research products) was emphasised and the need for DFID to be explicit on approvals procedures/processes that the project is required to follow (for example on break point approval and SEQAS research approval). Implementation of a number of components in the project was significantly delayed pending approval from DFID on the proposals submitted (see timeline of key decisions). Maintaining momentum in decision making is vital to keep the project moving forward and there are points at which the lead adviser needs to take a decision/set direction potentially in the absence of consensus between cross cutting advisers in the office. Finally, the setting up of both financial and narrative report formats/processes proved unnecessarily protracted and with hindsight, it would have been more effective for partners to propose formats for DFID’s approval, rather than the other way round. Partnerships between DFID funded projects should be explored geographically to exploit synergies. DFID should strengthen horizontal links between DFID programmes within geographical areas e.g. links between the SGBV (Sexual and Gender Based Violence) within DFID’s SSAPR police programme and ASSP. Potential partnerships with other donors should also be explored further (beyond the funds already committed by Sweden). DFID should continue to engage on donor coordination/harmonisation of support within DPS (new provincial health districts) and explore other new co-funding opportunities for ASSP going forward. ASSP interfaces with a number of other health projects. The project has been affected by supply chain issues in PMI’s malaria project which provides bed-nets for health facility use for inpatients and malaria drugs. DFID intends to follow up with USAID. Alongside ASSP, DFID has begun funding UNICEF for two years to support CMAM (Community based Management of Acute Malnutrition) in 39 health zones and support child health days (for vitamin A and deworming). At the moment, discussions are underway to refocus the CMAM component of this project as two assumptions have changed. Firstly funding for commodities of RUTF (Ready to Use Therapeutic Food) cannot be assured beyond an initial 18 months and secondly, ASSP is now piloting home based management of malnutrition with high energy porridge in conjunction with the ANJE (infant feeding) and home gardening behaviour change work. DFID’s centrally funded project implemented by Liverpool Tropical School on neglected tropical diseases has had delays moving from the assessment phase to implementation phase. IMA have maintained 28 close contact with this project and the RTI neglected tropical disease project to monitor how they interface. Asset monitoring and control The programme has inherited assets from the previous Access to Health 2 project and purchased a considerable number of assets and will continue to acquire more in the year two. The construction and rehabilitation of health facilities will expand in the year two and will need careful documentation. The consortium lead – IMA has recruited a director of operations who has, among other responsibilities, the management of ASSP assets. Spot checks on assets are routinely made on field visits. IMA has yet to share with IPs good practice guidance on keeping and maintaining programme assets on the field to comply with DFID policy. IMA should improve asset management systems within IMA and used by implementing partners. G: CONDITIONALITY Update on partnership principles There is not a project MOU in place with the Government and this has been deferred pending a country level agreement between DFID and the GoDRC. We have applied an assessment of the Partnership Principles to ASSP, although DFID DRC is yet to produce a formal assessment for the DRC country programme. We consider that the commitment of the Government to health sector development, commitment of the Secretary General to strengthen accountability/governance within the sector, engagement of the Ministry of Health on improving Public Financial Management and improving transparency through roll out of new information systems (such as HR information and HMIS) is very promising. The project works through strengthening government systems and the Ministry has taken strong ownership over the project. We feel that this provides us a sound basis for continuing our partnership with the Government of the DRC through ASSP. H: MONITORING & EVALUATION Evidence and evaluation To date, there have been no key changes to evidence that have had implications on the programme design or implementation. In the past year, a Theory of Change (TOC) document was completed. It has not been directly examined in the past year’s monitoring and evaluation. The TOC, in particular the health systems strengthening programme model will be focus on the mid-term process evaluation. Within the overall ASSP budget, DFID has allocated £4.7m for an Operations Research and Impact Evaluation sub-component. This subcomponent is implemented by Tulane University as a sub-contract to IMA. An impact evaluation is planned for this programme, and the baseline study fieldwork was conducted from March-June 2014. Data is currently being processed and preliminary results are expected in October 2014. Since the initial set up of the subcontract, DFID and IMA realised the complexity of managing a research contract, which may be more than is realistically possible from an implementing agency. Therefore, since September 2013, DFID has become more closely involved in the oversight and direction of the ORIE component, ensuring in particular that the governance and quality assurance of the impact evaluation is aligned with DFID evaluation policy. IMA has been receptive to DFID’s deeper involvement in the management of the research component of the project, as it reflects recognition from all parties that since this is a specialised function requiring appropriate technical support. 29 An Improvement Plan for the ORIE component was put in place in December 2013, stating outputs and deliverable dates for the Impact Evaluation, Operational Research and the Governance and Management of the ORIE. In June 2014, DFID concluded that the issues, objectives and actions in the improvement plan were being satisfactorily addressed and expects to approve and close the improvement plan in August 2014. In December 2013 the TOR for the ORIE component, including requiring an ORIE plan, was drafted and submitted to SEQAS (DFID’s external quality assurance service). This was 14 months after the inception phase started and therefore reflected some of the discussion and work that had already been done within the project. The TOR was agreed in February 2014. The ORIE Oversight Committee was established to guide the strategic direction of the independent evaluation and operational research and to ensure its quality. The members consist of representatives of DFID, Tulane, IMA, the DRC Ministry of Health and an external research/evaluation expert. To ensure the impartiality of the evaluation quality assurance (QA), the external consultant will not provide the formal QA services via DFID’s SEQAS contract. The first meeting was held on June 2014. Quality Assurance for the evaluation studies is via SEQAS, in accordance with Evaluation Department QA procedures at entry and exit. Operational research QA is conducted by the ORIE Oversight Committee. At entry, a three-step approval process for the OR studies has been established. This serves to provide clarity about the research topic/theme of each study; a concept note outlining in 3-4 pages the key features of the study; a full study protocol. SEQAS QA templates are currently being adapted for use as QA templates for OR study protocols and reports. The ORIE Plan was drafted by Tulane University and accepted in May 2014. A total of 10 studies are included in the ORIE component as shown below: Figure 6: Progress on research studies in the ORIE component to date Study Baseline Impact Evaluation Mid-term Process evaluation Endline Impact Evaluation CHE User Fee Community Empowerment Health Worker Motivation WASH Value For Money Family Planning Nutrition (additional funding) Start date Topic/ Questions Concept Note Protocol Field Work May-14 Y Y Y Y Oct-15 Y Y n/a Apr-14 Apr-14 Y Y Y Y Apr-14 Y Aug-14 Y Aug-14 Sep-15 Jan-15 Y Y tbd Y Report Y Y Y DFID and Tulane set the target of having all concept notes completed and approved by August 2014. No research findings have been reported to date. 30 Monitoring progress throughout the review period Direct feedback from stakeholders and beneficiaries The MoH was closely engaged in the design and early implementation of the programme and has maintained this. The steering group for the programme (with joint membership from GoDRC, donors and IMA) was not progressed as there were concerns that the Ministerial Decree drafted by the MoH implied that a parallel oversight body for DFID’s project would be set up. Instead, the quarterly two day partners’ workshops which are chaired by the Ministry of Health and include IPs, technical partners and provincial/district officials have provided this oversight function. The field visit for the annual review spoke with patients, staff, local authorities and health management teams. Feedback from the central Ministry of Health on the progress and approach of the programme has consistently been positive. The Secretary General commented that in general ASSP is well aligned with government plans. He has identified that there is good cooperation between DFID and the Ministry of Health, particularly on implementation, highlighting that senior MOH officials have participated in previous field visits including the annual review field visit. Within health zones, concerns were raised by local authorities and facility staff about the importance of accelerating the work on rehabilitation and or construction of infrastructure and equipment, including access to drinking water and lighting in health facilities. Earlier during year one of implementation DFID received feedback from a number of stakeholders on stock-outs of drugs. This situation seems to have improved to some extent more recently. Staff continue to raise the issue about lack of reliable government salaries and DFID/IMA continue engagement with the Ministry of Health on this issue but do not plan to reconsider the use of primes at health facilities. During the annual review field visit patients gave positive feedback on improvements in health facilities (such as availability of drugs) but commented on the need for improvements on buildings/lighting. Monitoring activities throughout review period DFID has regular meetings with the Ministry of Health and has attended a number of workshops/trainings implemented by the project during the year. The figure below outlines field visits in 2013/14. Figure 7: Field visits during year one of implementation Date Field visit – Province Purpose of visit March 2013 Kasai Occidental – Access to Health (IRC) Province Orientale ASSP Maniema-ASSP Kasai Occidental – Nutrition programme Equateur – ASSP with participation of Stephan Dercon and Head of Office Kasai – ASSP and Support to Malaria Control in DRC Kasai Occidental - ASSP Kinshasa clinics – ASSP ORIE Component by Evaluation adviser Kasai Occidental Monitoring of handover (IRC to SANRU) July 2013 July 2013 July 2013 October 2013 October 2013 December 2013 April 2014 July 2014 4-8th Aug 2014 (planned) South Kivu Monitoring ASSP implementation/handover issues Lubutu hospital transfer to ASSP Scope ideas for new nutrition programme Monitoring ASSP implementation in North Ubangui Monitoring of ASSP in Tshikapa and announcement of new malaria programme to Kasai provincial officials Monitoring ASSP implementation in new health zones Monitoring Tulane’s household baseline survey training ASSP annual review field visit to Mweke and Ilebo Kasai Occidental Itombwe and Minembwe 31 DFID DRC has not yet put in place a planned contract for third party monitoring or national external audit. In late 2013 the health team devised detailed ToRs for two programme funded monitoring officers (one technical and one financial) who would be field based. We have not pursued recruitment of these posts following a decision to implement this capacity cross-office. In the event that third party monitoring is not imminent by the end of the year, the health team should consider contracting this using funds from the Access to Health care in the DRC business case. _______________________________ 32