PEDIAT.GIT

-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
GASTRO-ENTESTINALTRACT [
GIT
] SYSTEM AND ABDOMINAL
EXAMINATION
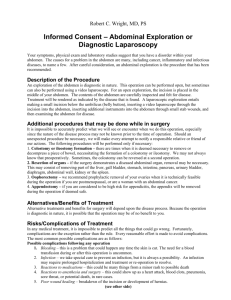
The alimentary or the GIT system and abdominal examination is one of the major part of the art of physical examination.
In the strict saying, there are some differences between the abdominal examination and the
GIT systemexamination, however, many aspects are the similar.
I will point to theses difference in the following paper.
In pediatrics, the sequences of the physical examination of the abdomen may not be strictly applied.
The abdominal examination requires the patient to be supine and fully exposed. However, toddler and young children may find that frightening and be uncooperative.
For that reason, you must try to make friendship with the child whilst making inspection and positioning him appropriately.
Young infants and children may be better examined while they are on their mother knees.
Expose the patient from the nipple to the knees, unless pubertal girl.
Do not expose genitalia of older children.
First before touching the baby, observe him to get as much as information as possible before losing the rapport with him when he start crying after being undressed.
By observation, comment on the following; consciousness level, interest in the surrounding, built [emaciated, under-built or failing to thrive, pale, jaundiced, cyanosed or in respiratory distress ( RD )].
Have a quick look for any dysmorphic findings and look for finger and toe clubbing in both hand and toes.
Be aware that abdominal examination include also the oral cavity. If you are asked to examine the GIT system start by general inspection [dlevel of conscious, state of nutrition, jaundice, cyanosis, pallor, dysmorphic features, RD, IV line monitor and oxygen therapy, then proceed to the oral cavity, however, if the question is abdominal examination, start by the abdomen, and then, the related part as guided by your findings.
INSPECTION
Undress the baby form the middle of the chest or the nipples to the middle of the thigh or the knees and keep him lying supine with knee and hip flexed and without below.
Be on the right side of the patient and try to be on the level of the child. You may need to kneel on your knees.
Wash your hands.
Introduce yourself to the parents and/or the child if he is old enough.
The light should be adequate.
Inspect for the following shownin the table below.
1
2
5
6
3
4
7
8
Contour of the abdomen Symmetrical
Asymmetrical bulge
Generalized distension, localized distension or flank distension
Scaphoid.
Chest and abdomen move Movement of the abdomen with inspiration simultaneously outward during inspiration or there is a paradoxical movement [abdomen moves outward while the chest ins moving inward].
This may be normal up to
5 years of age
Restriction of movement of the whole abdomen or on one part of the abdomen [pain due to peritonitis for instance]
Bulging and its location Location and approximate size
Pulsation and its location Location [aorta pulsation may visible in anxious and thin child]
Pigmentation of the abdominal wall
Discoloration of the abdominal wall
Redness around the umbilicus.
Caput medusa
Discoloration lateral to the umbilicus near the flanks
[pancreatitis]
Prominent vein
Caput medusa is a dilated vein around the umbilicus that drain away from the umbilicus due to portal HTN . If presents look for chronic liver diseases signs
Portal hypertension
Obstruction of the inferior vena cava
Obstruction of portal vein
Obstruction of the hepatic vein [Budd Chiarr]
Over a malignant mass.
Or simply form severe abdominal 7distension in8terfering with ve9nous drainage
Direction The presence of peristalsis waves, if present
From left to right over the right hypogastric area and epigastric area
-
12
13
14
15
16
9
10
11
17
Pupic hair
Umbilicus [everted, inverted or any umbilical hernia
Hernial orifices
Distributuin
Everted umbilicus or umbilical hernia from increased intraabdominal pressure due to a mass or ascitis
Inguinal hernia from increased intra-abdominal pressure due to a mass or ascitis in congenital hypertrophic pyloric stenosis
[ CHPS ]
Scars and its location and measurement
Cutery marks and their distribution striae
Obvious stoma
Abdominal Skin colour Shiny, red and distended
Umbilicus in the neoborn Clean, infected, erythema around it
Necrotizing eneterocolitis
[ NEC ] in newborn
Local infection which may progress to sepsis in newborn or omphalitis [serious condition with high mortality rate]
PALPATION
Tell the child what you are going to do.
-
-
-
-
-
-
-
-
-
Ask him if there is any pain in the abdomen.
Start by superficial, gentleand light palpation away from the pain.
Warm your hand before touching the child abdomen.
Kneel on your knees on the right side of the child to be at his level.
Begin away from you and examine each quadrant in turn.
6
7
8
There are 9 parts or quadrant of the abdomen. These are shown in the table below;
SERIAL AREA BOUNDRIES
1
2
3
Right hypochondrium
Epigastric area
Left hypochondrium
Superiorly, the costal margins, inferiorly line above bot iliac crest and medially; line connecting the manibriumsterni to the symphysis pubis.
Right hypochondrium
Right hypochondrium
4
5
Right lumbararea
Right iliac fossa
Right hypochondrium
Right hypochondrium
Umbilical area Right hypochondrium
Right hypochondrium left iliac fossa
Right hypochondrium
Right hypochondrium
9
Left lumbar area Right hypochondrium
Abdominal distension may be due to any one of the following [can be remembered by 5 F s ; flatus, fat, fetus and fluid] and is summarized in the table below;
SERIAL
Fat
Fluid
Flatus [gas] fetus
AREA
Obisity
Ascitis
Intestinal obstruction
Pregnancy in adolescent girls
REMARKS
Obesity
Nephritic syndrome
[ NS ]
Chronic liver diseases
Congestive heart failure [ CHF ]
Medical
[coagulation disorder
Traumatic
Post-surgery
HAEPTOMEGLLY
The enlargement of the liver can be due to several mechanisms.
The concept of liver size have been based on age related clinical indices.
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
These indices are; 1]- the degree of the extension of the liver below the costal margins
[ BCM ] in the right mid-clavicular line [ MCL ], 2]- the span of the dullness to percussion, 3]- and the length of the liver vertical access,as estimated by imaging techniques such s ultrasonography [ US ].
To examine for hepatomegally, flex the fingers at the metacarpo-phalengyal joint [ MPJ ] using the forefingers to the parallel of the costal margin.
Begin in the RIF and workup toward the costal margin.
You may ask the child to take child to take inspiration while you are going up to meet the edge of the liver.
Young infants, frequently, have a palpable liver edge up to 2 cm BCM .
Measure the distance between the right costal margin and the edge of the liver in the MCL by a measuring tape [you may use finger breadth as a rough estimate].
Describe the texture, [smooth or nodular], the border [sharp or irregular], and wither pulsating or not and any point out to any tenderness.
The following features in the table below differentiate the liver from other organs during palpation;
ORGAN
SITE OF
ENLARGMENT
INSPIRATION
LIVER
To right iliac fossa
[ RIF ]
Descends
CAN GET ABOVE IT
No
SPECIAL FEATURE
None
PERCUSION
Dull
PULSATILE
EXPANSILE
May be
May be
SPLEEN
To right iliac fossa
[ RIF ]
Descends
No
Notch
Dull
No
No
KIDNEY
To Flanks
Descends
Yes
Ballotable
Resonant over the overlying bowel
No
No
SPLEENOMEGALY
Palpate for the spleen from the RIF with your left hand splinting the lower edge of the rib cage posteriorly.
If you have any difficulty, lie the child on his/her right side and palpate the spleen while the child is taking deep inspiration.
The spleen tip may be palpable normally in the neonates.
Measure the distance from the lower costal margin and the lower most edge of the spleen in the MCL by a measuring tape.
Percuss out the border of the spleen at the end.
DETECTION OF KIDNEY ENLARGMENT
The kidney enlargement is evaluated by bi-manual palpation and ballottement.
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
Push your left hand in the renal angle [costo-vertebral angle] over the lateral side of the back and feel the kidney anteriorly with your right hand.
Ballot the kidney between your hands.
A common mistake is to push too laterally with the left hand.
DETECTION OF AN ABDOMINAL MASS
If a mass is found during the palpation of the abdomen, describe the following; 1]- the site,
2]- the shape, 3]- the size, 4]- the consistency [feces are indentible], 5]- the mobility [does it move with respiration], 6]- wither there is any tenderness, 7]- and wither it is pulsatile [such as in the case of abdominal aneurysm].
Finally, percuss for the presence of dullness or resonant if the bowel is overlying it and does this alter after maturation or defecation.
PERCUSSION
The percussion should be performed in the following conditions; 1]- the presence of organomegally, 2]- the presence of abdominal mass, 3]- or the presence of ascites.
To demonstrate ascites, there are 2 different tests.
These tests are; 1]- the fluid thrill, 2]- and the shifting dullness.
In the supine position, the fluid, which is dull to percussion gravitates to the lowermost part of the abdomen and laterally and the intestines which are filled by gases float upward and toward the surface.
Percussion from the umbilicus toward the flanks reveals a line of demarcation between the dullness and the resonance notes.
The position at which the line of demarcation is located will change as the patient is turned to onto his side. This is called shifting dullness.
The fluid thrill is detected in gross ascites by taping the flank toward the examiner by the right index finger while the palm of the left hand is placed over the left flank and an assistant is putting his ulnar side of one of his hand over the umbilicus in a vertical axis.
After tapping with the right index over the right side, you will receive a wave felt on the palm of your left hand because of the fluid movement.
In severe and gross ascites, the following signs as shown in the table below will be evident.
3
Serial SIGNS
1
2
Generalized distension of the abdomen.
Full flanks.
Everted umbilicus.
Full scrotum
Edematous abdominal wall.
There may be an inguinal hernia.
REMARKS
From increased intraabdominal pressure
ASCITIS
Ascites is the accumulation of fluid in the abdominal cavity.
-
-
-
-
-
-
-
-
-
-
While te patient is in the supine position, the fluid will fill the flanks by the action of the gravity and the intestine will move up in the centre of the abdomen.
In massive ascitis, the whole abdominal cavity may be filled with fluid and becomes tense and the umbilicus becomes everted.
Minimal ascitis may not be detected by the physical examination and only detected by ultrasound [ US ] examination of the peritoneal cavity.
Ascitis may be transudate, exudates or hemorrhagic [such as in malignancy or trauma].
The best way to examine for ascitis and differentiate it from localized mass or gas is percussion [fluid thrill and shifting dullness].
If the distension is due to gases, the percussion notes is tympanic [sound like a drum being stroken].
If the abdominal distension is due to fluid, the percussion notes is stonney dullness [mainluy in the flank and lateral aspects of the abdomen with line of demarcation between the dullness of ascitis and the tympany notes over the intestine which lies in the center of the abdomen superficially].
Fluid thrill is valuable in documenting the presence of ascitis.
To perform fluid thrill, the patient should be lying flat on the bed supine with slightly flexed legs. You need to put the palm of your left hand over the patient left flank and ask an assistance to but the ulnar side of one of his hand over the center of the abdomen. Then you flick on the flanck of the patient which is toward you by your right index. You will receive afeeling like a wave hitting the palm of the hand you are placing over the left flank. It is only positive in moderate to massive ascitis
THE CAUSES OF ASCITIS
The causes of ascitis are shown in the table below
1
2
As a part of generalized anasarca from whatever cause hypoalbuminemia 1]- Nutritional [inadequate
-
-
-
-
-
-
-
-
-
-
3 Cardiac disease intake or protein loosing eneteropathy or malabsorption].
2]- Renal loss in nephritic syndrome.
3]- Decreased synthesis of albumin in advanced liver disease
1]- Congestive Heart Failure
[ CHF ].
2]- Constrictive pericarditis.
AUSCULTATION
Auscultation is mainly used for 2 indications.
These indications are; 1]- to document the presence or absence of bowel [peristaltic] movement sounds or bowel sounds[ BS ]; which are called borborygmi, their intensity, especially if there is a nasogastric tube [ NGT ] in place or there is abdominal distension, 2]- and to identify any bruit but this is not a part of routine examination and only performed if the child is hypertensive or has neurofibromatosis, as they are associated with renal artery stenosis.
Bruit may be detected lateral and above the umbilicus and may indicates renal artery stenosis.
For examining for the presence or absence of bowel sound, the diaphragm of the stethoscope is placed above and to the right of the umbilicus.
The time for listening for BS should be not less than 60 seconds, otherwise present but hypoactive BS may be missed.
Absence of BS for 3 minutes or more in various parts of the abdomen indicates paralytic ileus.
The BS are increased [hyperactive] in cases of early stages of intestinal obstruction and during intestinal hurry [such as an episode of gastro-enteritis].
To examine for renal artery stenosis bruit, place the stethoscope above and lateral to the umbilicus in both side.
The other cause of bruit is malignancies of the abdomen.
ABDOMINAL CIRCUMFERENCE MEASURMENT
It is of help when trends are traced, such as comparing the circumference of the abdomen in following patients with intestinal obstruction, necrotizing entercolitis [ NEC ] or ascitis.
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
The measurement should be taken at the same level to avoid false impression.
Use good light.
ANAL AND RECTAL EXAMINATION
Offer to examine the anus and rectum if they are relevant [such as in inflammatory bowel disease (IBD), anal fissure, skin tag, fistula or constipation or when hirschbrung disease is suspected.
Firstly, inspect the anal region a good light.
Place the patient in supine position , abduct the thigh and flex the legs.
In older children, the patient may be placed in semi-prone position or on his side by placing him on his left breast, while his right thigh and knee are drawn up.
Draw aside his buttocks and inspect the anus for position [normal, anteriorly or posteriorly displaced], size [small], any nearby sinus or skin rash and inspect the external anal sphincter.
Use good light.
Inspect the per-anal area for anal position and location [normal or anteriorly displaced, size of the opening [the opening may be not the anus and just an opening of a fistula while there is anal atresia], the external anal sphincter, any obvious fissure or blood coming from it, any diaper rashes or rashes around the anus and is the anus protruded in rectal proplapse.
Look for any chronic sinuses, inflamed swelling or fistula nearby [chron disease].
Scratch lateral to the anal opening in the buttuck inside to see the sphincter reflexes.
Rectal examination should not be omoitted, especially in lower GIT hemorrhage or intestinal obstruction.
Use your well lubricated little finger of your dominant hand.
Insert the finger directing inward and toward the spine. Nor more than half of the finger is inserted.
Feel for the tone of the sphincter an find wether the rectum is tight, empty or full of stool.
Feel for any growth [polyp or tumor], ulcer and thrombosed hemorrhoid [piles].
After removing your finger, look for any blood, mucus or pus on your finger.
Document any tenderness and its location.
The differences between gastric ulcer [ GU ] and duodenal ulcer [ DU ] are shown in the table below;
FACTOR
Onset
Site
DUODENAL ULCER
2 – 4 hours after the meal
Right half of the epigastrium or, even, right
GASTRIC ULCER
15 – 60 minutes after the meal
Mid epigastrium
-
-
-
-
-
-
-
-
-
-
-
Radiation to the back
Relation to the food
Gastric analysis
hypochondrium
Rare
Pain is increased by food
High acid output [increased
HCl ] common
Pain is decreased by food
Normal acid output [normal
HCl ]
THE EXTERNAL GENITALIA, TESTICLES AND HERNIAL ORIFFICES
EXAMINATION
The hernia orifices, testicles and the external genitalia are part of the abdominal examination.
For male check for the following; 1]- the size of the testes, 2]- are the testes already have descended into the scrotum or not, 3]- is there any testicular or scrotal swelling, redness or tenderness, 4]- are the testicles of the same size, 5]- is the urethral meats in its normal position [to exclude hypospadius], 6]- is there any phimosis, paraphimosis or chordate, 8]- and you may need to measure the stretched penile length when indicated.
For adolescent, assess the tanner staging and pubic hair distribution.
Look for abnormally shaped genitalia and bifid scrotum.
For female, the examination must include any ambiguity [clitoris size, fusion of labi] and you must palpate the inguinal ligament for any mass [may be a testicles in a viralized female in congenital adrenal hyperplasia ( CAH )].
For the hernia orifices, inspect for any lump in the inguinal ligament.
Hernia may be already have been reduced spontaneously at the time of your examination.
For that reason, ask the patient to strain to increase the intra-abdominal pressure in older child or rely on the history in infants.
You must differentiate between scrotal swelling, inguinal hernia and hydrocele.
Most of the inguinal hernia in children is indirect.
Examine the child lying down initially, and re-examine him while he is standing up, if he is old enough and you are not certain.
The differences between inguinal hernia and hydrocele are shown in the table below;
THE DIFFERENTIATING
FEATURE
INGUINAL HERNIA HYDROCELE
Transmits the cough impulse
Yes No
You can get above it
The testes can be
No
Yes
Yes
No
palpated separately
Transillumination
No Yes
By Dr: ATTALLAH ABDULLAH AL MUTAIRY
Consultant pediatric intensivist
The head of the pediatric intensive care unit [ PICU ], Yamamah Maternity and Children
Hospital [ YMCH ].