Case #1:
advertisement

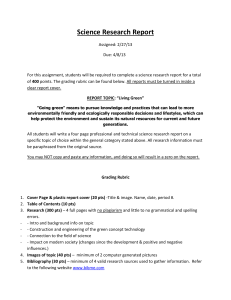
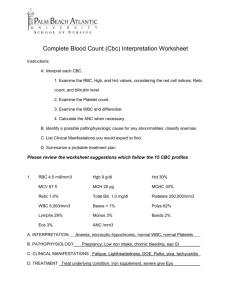
Assignment: To prepare an individual paper (2-3 pages) and a group presentation for one of the following cases. Paper: 25 pts Presentation 25 pts Due: Wednesday Aug 11 Probable cause of symptoms: what is happening in the body that could account for the each of the observed symptoms? Be specific. For example: a runny nose observed in a person who has the flu is the result of the body attempting to rid itself of the respiratory cells that have been damaged and ruptured by the influenza virus. 8 pts What homeostatic set points have been altered? 8 pts How is the body attempting to restore homeostasis? 8 pts Diagnoses: What is the overall causative agent. 10 pts Treatment: What would advise the patient to do and how would this help alleviate the symptoms 8 pts Paper/Presentation: Organization, clarity, citations, slide effectiveness: 8 pts Case #1: Ann, who is 35 years old, complains of progressively worsening, fluctuating pain at her knees and joints of her hand for several weeks. The pain is at its worst early in the morning. The symptoms are symmetrical- the same joints on both sides of her body are affected. She reports a low grade fever and fatigue at times. Physical examination revels limited of her wrists and inflammation with spongy swelling around her knee joints. Slight ulnar deviation of the fingers at the painful metacarpophalangeal joints of her hands is noted. There are no skin lesions present. Many different disorders can cause joint pain. Medical tests revealed: 1. Synovial fluid analysis: cloudy, reduced viscosity, absence of bacteria, no uric acid crystals. 2. X-ray studies of the hand: detectable deterioration of articular cartilages in metacarpophalangeal joints 3. Serum rheumatoid factor: 1”60 titer, elevated Erythrocyte sedimentation rate Case #2 Jose, a 50 year old office worker, is brought to the E.R. by his wife. Jose complains of shortness of breath on exertion over the last few months; it has become so severe that he now needs to rest after walking only a short distance. He recently almost fainted in the front yard after he checked the mailbox. Jose had been a heavy smoker for 25 years; he has a persistent cough with heavy mucus production. He has had several respiratory infections over the last few months. Jose is placed on oxygen. A chest X-ray and the following blood tests results were obtained: 1. RBC count: 6.2 million/mm3 2. 3. 4. 5. 6. 7. HCT: 55 MCV 98 mm3 MCV: 30 pg WBC: 10,000 / mm3 Platelets: 250,,/ mm3 Arterial Blood gases: before oxygen was given: pH: 7.25 Pco2 48 mm Hg Po2 55 mm Hg HCO3 > 30 mEq/ L Chest X- ray: normal with expanded lungs with small areas of probable fibrotic changes Case #3: Nicole Smith, a 32 housewife living in Tucson Arizona. She is pregnant with her second child- late in her first trimester. During the last two weeks she has been tried and often becomes short of breath from even the slightest exertion. Nicole has been prone to periods of light-headedness, but has not fainted. She has also noticed cramping in her legs, thirst, and a sore tongue. Her physician notes tachycardia, pale gums and nail beds, and a enlarge tongue. Her doctors orders a blood sample be taken. These are her test results: Table 1. Blood Sample Results Red Blood Cell Count 3.3 million/mm3 Hemoglobin (Hb) 6.8 g/dl Hematocrit (Hct) 32% Serum Iron low Mean Corpuscular Volume (MCV) low Mean Corpuscular Hb Concentration (MCHC) low Total Iron Binding Capacity in the Blood (TIBC) high Case #4 Jane, a 27 year old woman, awakens one morning with blurred vision and pain in her right eye. She sees her family physician, who determines that her sclera, conjunctiva, cornea, and ocular tension are normal, but her visual acuity is markedly reduced in that eye. An ophthalmologist is consulted and, after an exam, diagnoses optic neuritis Jane is then referred to a neurologist, who learns that she had earlier forgotten episode of weakness and clumsiness of her left arm. The problem persisted for only two days, and Jane attributed it to lifting heavy suitcases on a trip. An MRI of her brain revealed several plaque type lesions in the white matter of the brain but no other abnormalities. A lumbar puncture is preformed, and the results are: Pressure: 150 cm/H20 Color: clear, colorless Protein: 50 mg/dl Gamma globulin: 20 of the total protein level Cells: no RBC’s WBC count 6/ mm3 IgG: high ratio of IgG to other proteins Culture: no bacteria Case #5 Theresa, a 20 year old woman lost consciousness while in a shopping mall. She had no identification with her. In the emergency room the physician assessed her comatose state, noting among other physical findings, rapid respirations, and then ordered blood and urine studies. The following results were obtained: CBC: with normal limits Serum electrolytes: Sodium: 135 mEg/L Pco2 30 mmHg Potassium: 4.1 mEg/L HCO3 : 12 mEg/L Chloride: 100 mEg/L Blood urea nitrogen (BUN) 9mg/dl Blood glucose: 800 mg/dl Urinalysis: pH 4.6 Blood ph: 7.23 Glucose (+) Protein (-) Blood (-) Ketones (+) Case #6 Michael, a 32 old man, was feeling pain in his chest after eating his dinner, which he attributed to heartburn. The pain was often more server at night and after exertion. He sometimes also felt pain shooting down his back after eating. His doctor ordered X-rays, which show small section of Michael’s stomach protruding the diaphragm. The doctor also preformed an endoscopic biopsy, which indicated mucosal inflammation. An esophageal manometry showed decreased lower esophageal pressure.(LES). The pH in the esophagus was 5.5.